There are four main pesticide application methods, including hydraulic spraying, backpack spraying, basal trunk spraying, and aerial spraying. Pesticide application methods are mainly selected by considering the habits of target pests, the characteristics of target sites, and the properties of pesticides. Humans are directly exposed to pesticides in occupational, agricultural, and household activities and are indirectly exposed to pesticides via environmental media, including air, water, soil, and food. Human exposure to pesticides occurs mainly through dermal, oral, and respiratory routes. People who are directly and/or indirectly exposed to pesticides may contract acute toxicity effects and chronic diseases. Although no segment of the general population is completely protected against exposure to pesticides and their potentially serious health effects, a disproportionate burden is shouldered by people in developing countries. Both deterministic and probabilistic human health risk assessments have their advantages and disadvantages and both types of methods should be comprehensively implemented in research on exposure and human health risk assessment. Equipment for appropriate pesticide application is important for application efficiency to minimize the loss of spray solution as well as reduce pesticide residuals in the environment and adverse human health effects due to over-spraying and residues. Policymakers should implement various useful measures, such as integrated pest management (IPM) laws that prohibit the use of pesticides with high risks and the development of a national implementation plan (NIP) to reduce the adverse effects of pesticides on the environment and on human health.
- human health risk assessment
- pesticide application methods
- pesticide exposure
1. Introduction
2. Routes of Pesticide Exposure
People are not only directly exposed to pesticides in occupational, agricultural, and household activities [37,38,39][16][17][18] through different application methods [40][19], they are also indirectly exposed to pesticides via contaminated environmental media, including air, water, soil, and food [10,11,41,42,43][10][11][20][21][22]. These different types of exposure determine the degree of toxicity of pesticides [6,13,40][6][13][19]. The main ways pesticides come into contact with the human body are through the dermal, oral, and respiratory routes (Figure 21) [10,33,44,45,46,47][10][23][24][25][26][27].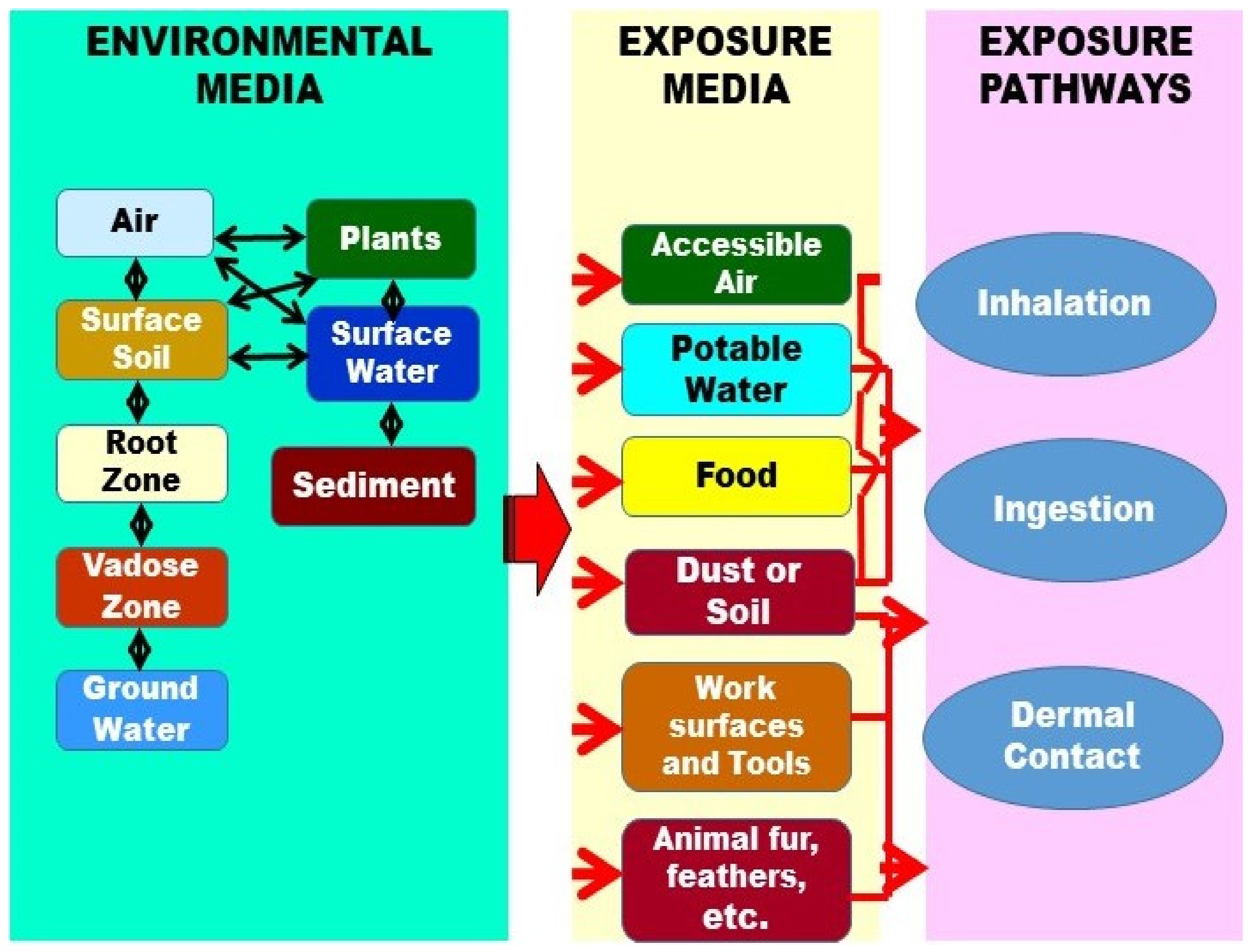
3. Human Health Effects Related to Pesticide Exposure
3.1. Acute Toxic Effects
3.2. Chronic Disease
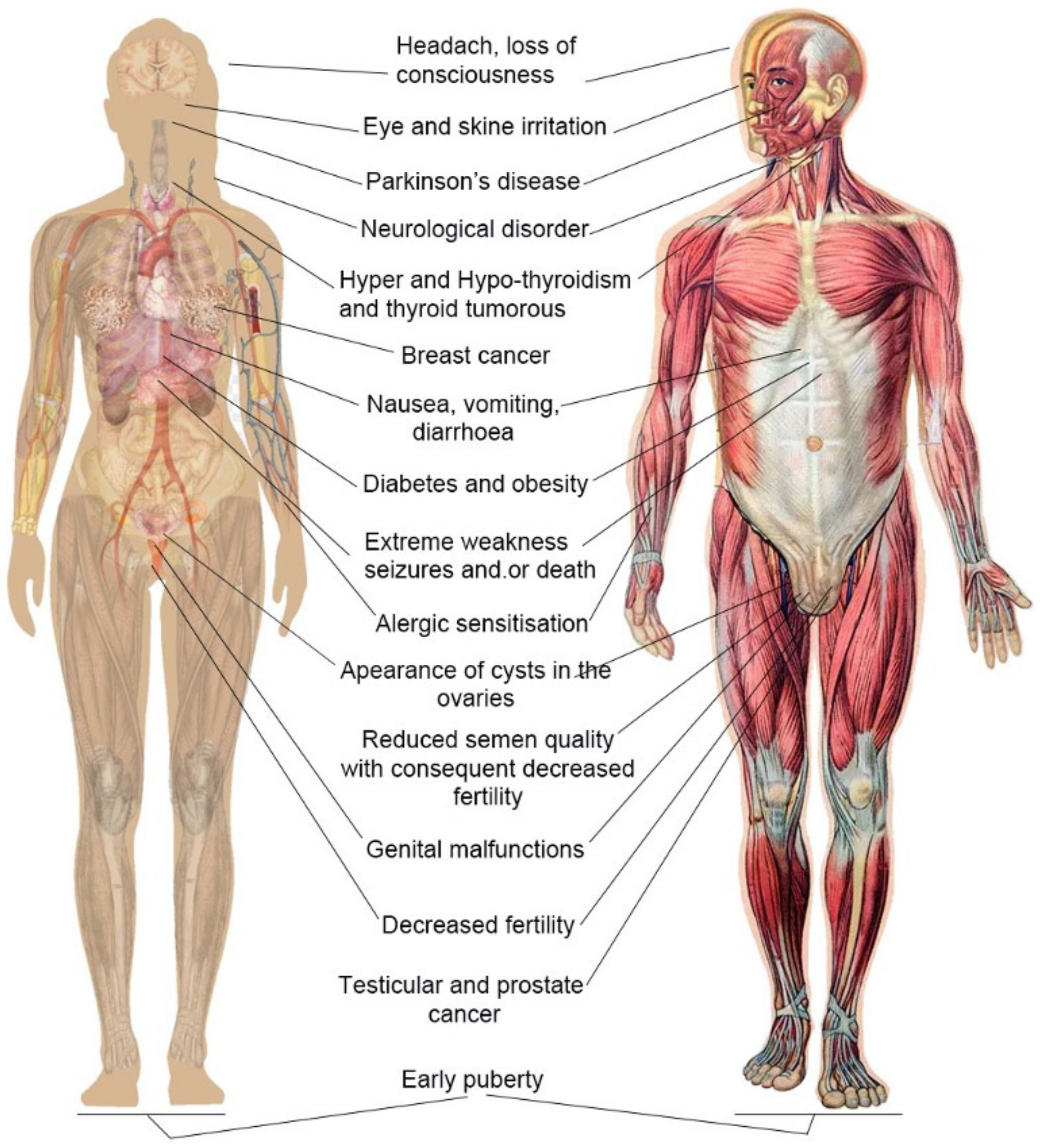
It has been documented that various chronic diseases and disorders occur after people have been exposed to pesticides [117[70][71][72],118,119], including cancers, adverse reproductive outcomes [120][73], male sterility [121][74], peripheral neuropathies [122][75], neurobehavioral disorders [123][76], impaired immune function (Nankongnab et al., 2020) [124][77], and allergic sensitization reactions, particularly of the skin [125,126,127][78][79][80]. Moreover, most of the pesticides examined affect male reproductive systems [124[77][78][79][80][81],125,126,127,128], causing sperm damage [118][71], DNA damage [129][82], and abnormal sperm morphology [13]. As an example, cumulative inhalation of cholinesterase activity as a result of long-term, low-dose exposure to organophosphorus compounds leads to chronic diseases [125][78]. Antonine et al. [121][74] tested the effects of low concentrations of Glyphosate; the decrease observed in levels of Clusterin mRNAs suggested that glyphosate targets the integrity of Sertoli cells. The decrease in the numbers of germ cells from day 14 onward highlighted the chronic effect of glyphosate at 50 nm, 500 nm, or 5 μm. Meltzer et al. [115][83] aimed to evaluate self-reported exposure to the Ringwood Mines/Landfill Superfund Site in relation to chronic health outcomes among members of the Ramapough Lunaape Turtle Clan nation and other residents of Ringwood, New Jersey. The results of the study indicated significant associations among Ringwood residents of Native American ethnicity between health issues and self-declared opportunities for Superfund site exposure. The results also showed a strong association between self-reported Superfund site exposure and the prevalence of bronchitis and asthma. Vanlaeys et al. [128][81] tested glyphostate alone, glyphosate-based herbside formulations, and POEA on an immature mouse Sertoli cell line (TM4) at concentrations ranging from environmental to agricultural-use levels; the results indicated that formulations of glyphosate-based herbicides induce TM4 mitochondrial dysfunction, disruption of cell detoxification systems, lipid droplet accumulation, and mortality at sub-agricultural doses. The results also showed that formulants, especially those present in Glyphogan, are more deleterious than glyphosate. Séralini et al. [78][33] discussed a 90-day feeding study which was conducted by Monsanto in order to achieve commercial release of this GMO, employing the sane rat strain and analyzing biochemical parameters in the animals. The results showed that in the treated males liver congestion and necrosis were 2.5 to 5.5 times higher than in the control groups. Marked and severe nephropathies were generally 1.3 to 2.3 times greater. In females, all treatment groups showed a two- to three-fold increase in mortality, and deaths occurred earlier. Males had more than four times the frequency of mammary tumors of the controls.References
- Aktar, M.W.; Sengupta, D.; Chowdhury, A. Impact of Pesticides Use in Agriculture: Their Benefits and Hazards. Interdiscip. Toxicol. 2009, 2, 1–12.
- Strassemeyer, J.; Daehmlow, D.; Dominic, A.; Lorenz, S.; Golla, B. Synops-Web, An Online Tool for Environmental Risk Assessment to Evaluate Pesticide Strategies on Field Level. Crop Prot. 2017, 97, 28–44.
- Taufeeq, A.; Baqar, M.; Sharif, F.; Mumtaz, M.; Ullah, S.; Aslam, S.; Qadir, A.; Majid, M.; Jun, H. Assessment of Organochlorine Pesticides and Health Risk in Tobacco Farming Associated with River Barandu of Pakistan. Environ. Sci. Pollut. Res. 2021, 28, 38774–38791.
- Carvalho, F.P. Pesticides, Environment, and Food Safety. Food Energy Secur. 2017, 6, 48–60.
- Chang, C.; Chen, M.; Gao, J.; Luo, J.; Wu, K.; Dong, T.; Zhou, K.; He, X.; Hu, W.; Wu, W. Current Pesticide Profiles in Blood Serum of Adults in Jiangsu Province of China and A Comparison with Other Countries. Environ. Int. 2017, 102, 213–222.
- Hernández, A.F.; Parrón, T.; Tsatsakis, A.M.; Requena, M.; Alarcón, R.; López-Guarnido, O. Toxic Effects of Pesticide Mixtures At A Molecular Level: Their Relevance to Human Health. Toxicology 2013, 307, 136–145.
- Tudi, M.; Atabila, A.; Ruan, H.D.; Wang, L.; Lyu, J.; Tong, S.; Yu, Q.J.; Sadler, R.; Phung, D.T.; Connell, D. Natural Dynamics and Residues of Pymetrozine for Typical Rice-Growing Areas of China. Ecotoxicol. Environ. Saf. 2022, 232, 113230.
- Abdel-Halim, K.Y.; Osman, S.R. Cytotoxicity and Oxidative Stress Responses of Imidacloprid and Glyphosate in Human Prostate Epithelial Wpm-Y. 1 Cell Line. J. Toxicol. 2020, 4364650.
- Lozier, M.J.; Montoya, J.F.L.; Del Rosario, A.; Martinez, E.P.; Fuortes, L.; Cook, T.M.; Sanderson, W.T. Personal Air Sampling and Risks of Inhalation Exposure During Atrazine Application in Honduras. Int. Arch. Occup. Environ. Health 2013, 86, 479–488.
- Macfarlane, E.; Carey, R.; Keegel, T.; El-Zaemay, S.; Fritschi, L. Dermal Exposure Associated with Occupational End Use of Pesticides and The Role of Protective Measures. Saf. Health Work 2013, 4, 136–141.
- Kim, K.-H.; Kabir, E.; Jahan, S.A. Exposure to Pesticides and The Associated Human Health Effects. Sci. Total Environ. 2017, 575, 525–535.
- Tudi, M.; Wang, L.; Ruan, H.D.; Tong, S.; Atabila, A.; Sadler, R.; Yu, Q.J.; Connell, D.; Phung, D.T. Environmental Monitoring and Potential Health Risk Assessment from Pymetrozine Exposure Among Communities in Typical Rice-Growing Areas of China. Environ. Sci. Pollut. Res. 2022, 1–14.
- Anderson, S.E.; Meade, B.J. Potential Health Effects Associated with Dermal Exposure to Occupational Chemicals. Environ. Health Insights 2014, 8, EHI-S15258.
- Damalas, C.A.; Eleftherohorinos, I.G. Pesticide Exposure, Safety Issues, and Risk Assessment Indicators. Int. J. Environ. Res. Public Health 2011, 8, 1402–1419.
- Yadav, I.C.; Devi, N.L.; Syed, J.H.; Cheng, Z.; Li, J.; Zhang, G.; Jones, K.C. Current Status of Persistent Organic Pesticides Residues in Air, Water, and Soil, and Their Possible Effect on Neighboring Countries: A Comprehensive Review of India. Sci. Total Environ. 2015, 511, 123–137.
- Tefera, Y.M.; Gaskin, S.; Thredgold, L.; Pisaniello, D. The Role of Formulation Co-Ingredients in Skin and Glove Barrier Protection Against Organophosphate Insecticides. Pest Manag. Sci. 2022, 78, 177–183.
- Simas, J.M.M.; Yamauchi, L.Y.; De Alencar, M.D.B. Risk Factors Associated Among Respiratory Health and Banana Farming. Arch. Environ. Occup. Health 2021, 76, 181–187.
- Sapbamrer, R.; Hongsibsong, S.; Naksata, M.; Naksata, W. Insecticide Filtration Efficiency of Respiratory Protective Equipment Commonly Worn by Farmers in Thailand. Int. J. Environ. Res. Public Health 2021, 18, 2624.
- Yan, X.J.; Zhou, Y.Y.; Liu, X.H.; Yang, D.B.; Yuan, H.Z. Minimizing Occupational Exposure to Pesticide and Increasing Control Efficacy of Pests by Unmanned Aerial Vehicle Application on Cowpea. Appl. Sci. 2021, 11, 9579.
- Liu, S.Y.; Jin, Q.; Ren, R.; Zhu, G.N. Risk Assessment of Endocrine-Disrupting Pesticides Exposure Through Consumption ofcarassius Auratuscollected from Qiantang River, China. Hum. Ecol. Risk Assess. 2021, 27, 865–875.
- Korucu, M.K.; Elibol, P.S.; Isleyen, M. An Environmental Risk Assessment for A Ddx-Contaminated Agricultural Area in Turkey: Soil vs. Plant or Human Vs. Animal. Environ. Sci. Pollut. Res. 2021, 28, 50127–50140.
- Islam, M.S.; Rahman, M.R.; Prodhan, M.D.H.; Sarker, D.; Rahman, M.M.; Uddin, M.K. Human Health Risk Assessment of Pesticide Residues in Pointed Gourd Collected from Retail Markets of Dhaka City, Bangladesh. Accredit. Qual. Assur. 2021, 26, 201–210.
- Tudi, M.; Daniel Ruan, H.; Wang, L.; Lyu, J.; Sadler, R.; Connell, D.; Chu, C.; Phung, D.T. Agriculture Development, Pesticide Application and Its Impact on The Environment. Int. J. Environ. Res. Public Health 2021, 18, 1112.
- Saeed, M.F.; Shaheen, M.; Ahmad, I.; Zakir, A.; Nadeem, M.; Chishti, A.A.; Shahid, M.; Bakhsh, K.; Damalas, C.A. Pesticide Exposure in The Local Community of Vehari District in Pakistan: An Assessment of Knowledge and Residues in Human Blood. Sci. Total Environ. 2017, 587, 137–144.
- Ali, N.; Kalsoom, K.S.; Ihsanullah, R.I.U.; Muhammad, S. Human Health Risk Assessment Through Consumption of Organophosphate Pesticide-Contaminated Water of Peshawar Basin, Pakistan. Expo. Health 2018, 10, 259–272.
- Sampath, S.; Shanmugam, G.; Selvaraj, K.K.; Ramaswamy, B.R. Spatio-Temporal Distribution of Polycyclic Aromatic Hydrocarbons (Pahs) in Atmospheric Air of Tamil Nadu, India, and Human Health Risk Assessment. Environ. Forensics 2015, 16, 76–87.
- Pedroso, T.M.A.; Benvindo-Souza, M.; Nascimento, F.D.; Woch, J.; Dos Reis, F.G.; Silva, D.D.E. Cancer and Occupational Exposure to Pesticides: A Bibliometric Study of The Past 10 Years. Environ. Sci. Pollut. Res. 2022, 29, 17464–17475.
- Yadav, I.C.; Devi, N.L.; Li, J.; Zhang, G.; Shakya, P.R. Occurrence, Profile and Spatial Distribution of Organochlorines Pesticides in Soil of Nepal: Implication for Source Apportionment and Health Risk Assessment. Sci. Total Environ. 2016, 573, 1598–1606.
- Mostafalou, S.; Abdollahi, M. Pesticides: An Update of Human Exposure and Toxicity. Arch. Toxicol. 2017, 91, 549–599.
- Lang, C.; Tao, S.; Wangj, X.J.; Zhang, G.; Fu, J.M. Modeling Polycyclic Aromatic Hydrocarbon Composition Profiles of Sources and Receptors in The Pear River Delta, China. Environ. Toxicol. Chem. 2008, 27, 4–9.
- Das, G.P.; Jamil, K.; Rahman, M. Effect of Four Organophosphorus Compounds on Human Blood Acetylcholinesterase: In Vitro Studies. Toxicol. Mech. Methods 2006, 16, 455–459.
- Phung, D.T.; Connell, D.; Miller, G.; Rutherford, S.; Chu, C. Needs Assessment for Reducing Pesticide Risk: A Case Study with Farmers in Vietnam. J. Agromedicine 2013, 18, 293–303.
- Séralini, G.-E.; Clair, E.; Mesnage, R.; Gress, S.; Defarge, N.; Malatesta, M.; Hennequin, D.; De Vendômois, J.S. Republished Study: Long-Term Toxicity of a Roundup Herbicide and A Roundup-Tolerantgenetically Modified Maize. Environ. Sci. Eur. 2014, 26, 1–17.
- Tsui, M.T.; Chu, L. Aquatic Toxicity of Glyphosate-Based Formulations: Comparison Between Different Organisms and The Effects of Environmental Factors. Chemosphere 2003, 52, 1189–1197.
- World Health Organization. Public Health Impact of Pesticides Used in Agriculture; WHO: Geneva, Switzerland, 1990.
- Zhang, Q.; Fu, C.; Guo, X.; Gao, J.; Zhang, P.; Ding, C. Fluorescent Determination of Butyrylcholinesterase Activity and Its Application in Biological Imaging and Pesticide Residue Detection. ACS Sens. 2021, 6, 1138–1146.
- Lu, P.; Li, Q.F.; Liu, H.M.; Feng, Z.Z.; Yan, X.; Hong, Q.; Li, S.P. Biodegradation of Chlorpyrifos and 3,5,6-Trichloro-2-Pyridinol by Cupriavidus Sp Dt-1. Bioresour. Technol. 2013, 127, 337–342.
- Tyagi, H.; Gautam, T.; Prashar, P. Survey of Pesticide Use Patterns and Farmers’ Perceptions: A Case Study from Cauliflower and Tomato Cultivating Areas of District Faridabad, Haryana, India. Int. J. Medipharm Res. 2015, 1, 139–146.
- Chawla, P.; Kaushik, R.; Swaraj, V.S.; Kumar, N. Organophosphorus Pesticides Residues in Food and Their Colorimetric Detection. Environ. Nanotechnol. Monit. Manag. 2018, 10, 292–307.
- Ding, G.D.; Bao, Y.X. Revisiting Pesticide Exposure and Children’s Health: Focus on China. Sci. Total Environ. 2014, 472, 289–295.
- An, X.H.; Ji, X.F.; Jiang, J.H.; Wang, Y.H.; Wu, C.X.; Zhao, X.P. Potential Dermal Exposure and Risk Assessment for Applicators of Chlorothalonil and Chlorpyrifos in Cucumber Greenhouses in China. Hum. Ecol. Risk Assess. 2015, 21, 972–985.
- Yuan, G.L.; Sun, Y.; Qin, J.X.; Li, J.; Wang, G.H. Chiral Signature of Alpha-Hch and O,P′-Ddt in The Soil and Grass of The Central Tibetan Plateau, China. Sci. Total Environ. 2014, 500, 147–154.
- An, X.H.; Wu, S.G.; Guan, W.B.; Lv, L.; Liu, X.J.; Zhang, W.P.; Zhao, X.P.; Cai, L.M. Effects of Different Protective Clothing for Reducing Body Exposure to Chlorothalonil During Application in Cucumber Greenhouses. Hum. Ecol. Risk Assess. 2018, 24, 14–25.
- Cao, L.D.; Zhang, H.J.; Li, F.M.; Zhou, Z.L.; Wang, W.L.; Ma, D.K.; Yang, L.; Zhou, P.G.; Huang, Q.L. Potential Dermal and Inhalation Exposure to Imidacloprid and Risk Assessment Among Applicators During Treatment in Cotton Field in China. Sci. Total Environ. 2018, 624, 1195–1201.
- Guodong, D.; Pei, W.; Ying, T.; Jun, Z.; Yu, G.; Xiaojin, W.; Rong, S.; Guoquan, W.; Xiaoming, S. Organophosphate Pesticide Exposure and Neurodevelopment in Young Shanghai Children. Environ. Sci. Technol. 2012, 46, 2911–2917.
- Fang, Y.Y.; Nie, Z.Q.; Yang, Y.M.; Die, Q.Q.; Liu, F.; He, J.; Huang, Q.F. Human Health Risk Assessment of Pesticide Residues in Market-Sold Vegetables and Fish in A Northern Metropolis of China. Environ. Sci. Pollut. Res. 2015, 22, 6135–6143.
- Demir, V.; Ergin, S. Occurrence and Assessment of Chemical Contaminants in Drinking Water in Tunceli, Turkey. J. Chem. 2013, 2013, 238374.
- Devi, N.L.; Yadav, I.C.; Qi, S.H.; Chakraborty, P.; Dan, Y. Distribution and Risk Assessment of Polychlorinated Biphenyls (Pcbs) in The Remote Air and Soil of Manipur, India. Environ. Earth Sci. 2014, 72, 3955–3967.
- Devi, N.L.; Yadav, I.C.; Raha, P.; Qi, S.H.; Dan, Y. Spatial Distribution, Source Apportionment and Ecological Risk Assessment of Residual Organochlorine Pesticides (Ocps) in The Himalayas. Environ. Sci. Pollut. Res. 2015, 22, 20154–20166.
- Fang, L.P.; Zhang, S.Q.; Chen, Z.L.; Du, H.X.; Zhu, Q.; Dong, Z.; Li, H.D. Risk Assessment of Pesticide Residues in Dietary Intake of Celery in China. Regul. Toxicol. Pharmacol. 2015, 73, 578–586.
- Farooq, S.; Eqani, S.A.M.A.S.; Malik, R.N.; Katsoyiannis, A.; Zhang, G.; Zhang, Y.L.; Li, J.; Xiang, L.; Jones, K.C.; Shinwari, Z.K. Occurrence, Finger Printing and Ecological Risk Assessment of Polycyclic Aromatic Hydrocarbons (Pahs) in The Chenab River, Pakistan. J. Environ. Monit. 2011, 13, 3207–3215.
- Yang, C.-C.; Deng, J.-F. Intermediate Syndrome Following Organophosphate Insecticide Poisoning. J. Chin. Med. Assoc. 2007, 70, 467–472.
- Mishra, A.K.; Gopesh, A.; Singh, K.P. Acute Toxic Effects of Chlorpyrifos on Pseudobranchial Neurosecretory System, Brain Regions and Locomotory Behavior of An Air-Breathing Catfish, Heteropneustes Fossilis (Bloch 1794). Drug Chem. Toxicol. 2022, 45, 670–679.
- Cui, K.D.; He, L.M.; Zhang, Z.Q.; Zhang, L.Y.; Mu, W.; Liu, F. Effects of Benzothiazole on Survival for Reduced Reproduction and Development in Tribolium Castaneum Herbst (Coleoptera: Tenebrionidae). Pest Manag. Sci. 2020, 76, 3088–3095.
- Debleecker, J.L. The Intermediate Syndrome in Organophosphate Poisoning: An Overview of Experimental and Clinical Observations. J. Toxicol. Clin. Toxicol. 1995, 33, 683–686.
- Uckun, M.; Yologlu, E.; Uckun, A.A.; Oz, O.B. Acute Toxicity of Insecticide Thiamethoxam to Crayfish (Astacus Leptodactylus): Alterations in Oxidative Stress Markers, Atpases and Cholinesterase. Acta Chim. Slov. 2021, 68, 521–531.
- Kwon, H.A.; Jeong, Y.; Jeon, H.P.; Kim, S. Comparing Passive Dosing and Solvent Spiking Methods to Determine the Acute Toxic Effect of Pentachlorophenol on Daphnia Magna. Ecotoxicology 2020, 29, 286–294.
- Vural, K.; Seyrek, O. The Neuroprotective Effect of Pioglitazone on Nb2a Mouse Neuroblastoma Cell Culture. Kafkas Univ. Vet. Fak. Derg. 2019, 25, 1–8.
- Abass, K.; Turpeinen, M.; Pelkonen, O. An Evaluation of The Cytochrome P450 Inhibition Potential of Selected Pesticides in Human Hepatic Microsomes. J. Environ. Sci. Health Part B 2009, 44, 553–563.
- Pereira, L.C.; De Souza, A.O.; Bernardes, M.F.F.; Pazin, M.; Tasso, M.J.; Pereira, P.H.; Dorta, D.J. A Perspective on The Potential Risks of Emerging Contaminants to Human and Environmental Health. Environ. Sci. Pollut. Res. 2015, 22, 13800–13823.
- Mosiichuk, N.; Husak, V.; Storey, K.B.; Lushchak, V. Acute Exposure to The Penconazole-Containing Fungicide Topas Induces Metabolic Stress in Goldfish. Chem. Res. Toxicol. 2021, 34, 2441–2449.
- Snow, N.P.; Horak, K.E.; Humphrys, S.T.; Staples, L.D.; Hewitt, D.G.; Vercauteren, K.C. Low Secondary Risks for Captive Coyotes from A Sodium Nitrite Toxic Bait for Invasive Wild Pigs. Wildl. Soc. Bull. 2019, 43, 484–490.
- Brown, M.D.; Carter, J.; Thomas, D.; Purdie, D.M.; Kay, B.H. Pulse-Exposure Effects of Selected Insecticides to Juvenile Australian Crimson-Spotted Rainbowfish (Melanotaenia Duboulayi). J. Econ. Entomol. 2002, 95, 294–298.
- Chen, H.L.; Yao, J.; Wang, F.; Bramanti, E.; Maskow, T.; Zaray, G. Acute Toxic Effects of Three Pesticides on Pseudomonas Putida Monitored by Microcalorimeter. J. Environ. Sci. Health Part B-Pestic. Food Contam. Agric. Wastes 2009, 44, 157–163.
- Lo, S.; King, I.; Alléra, A.; Klingmüller, D. Effects of Various Pesticides on Human 5α-Reductase Activity in Prostate and Lncap Cells. Toxicol. In Vitro 2007, 21, 502–508.
- Forsythe, S.D.; Devarasetty, M.; Shupe, T.; Bishop, C.; Atala, A.; Soker, S.; Skardal, A. Environmental Toxin Screening Using Human-Derived 3d Bioengineered Liver and Cardiac Organoids. Front. Public Health 2018, 6, 103.
- Kanu, K.C.; Ogbonna, O.A.; Mpamah, I.C. Acute Toxicity and Biological Responses of Clarias Gariepinus to Environmentally Realistic Chlorpyrifos Concentrations. Pollution 2019, 5, 839–846.
- Palkhade, R.; Yadav, S.; Mishra, S.; Muhamed, J. Acute Oral Toxicity of Pesticide Combination (Acephate 50% and Imidacloprid 1.8% As Active Ingredients) in Sprague-Dawley Rats. Vet. World 2018, 11, 1291–1297.
- Arias-Andres, M.; Ramo, R.; Torres, F.M.; Ugalde, R.; Grandas, L.; Ruepert, C.; Castillo, L.E.; Van Den Brink, P.J.; Gunnarsson, J.S. Lower Tier Toxicity Risk Assessment of Agriculture Pesticides Detected on The Rio Madre De Dios Watershed, Costa Rica. Environ. Sci. Pollut. Res. 2018, 25, 13312–13321.
- Petarli, G.B.; Cattafesta, M.; Sant’anna, M.M.; Bezerra, O.; Zandonade, E.; Salaroli, L.B. Multimorbidity and Complex Multimorbidity in Brazilian Rural Workers. PLoS ONE 2019, 14, e0225416.
- You, L.; Zheng, F.J.; Su, C.; Wang, L.M.; Li, X.; Chen, Q.Q.; Kou, J.; Wang, X.L.; Wang, Y.F.; Wang, Y.T.; et al. Metabolome-Wide Association Study of Serum Exogenous Chemical Residues in A Cohort with 5 Major Chronic Diseases. Environ. Int. 2022, 158, 106919.
- Conti, C.L.; Borcoi, A.R.; Almanca, C.C.J.; Barbosa, W.M.; Archanjo, A.B.; Pinheiro, J.D.; Freitas, F.V.; De Oliveira, D.R.; Cardoso, L.D.; De Paula, H.; et al. Factors Associated with Depressive Symptoms Among Rural Residents from Remote Areas. Community Ment. Health J. 2020, 56, 1292–1297.
- Meng, S.L.; Chen, X.; Song, C.; Fan, L.M.; Qiu, L.P.; Zheng, Y.; Chen, J.Z.; Xu, P. Effect of Chronic Exposure to Pesticide Methomyl on Antioxidant Defense System in Testis of Tilapia (Oreochromis Niloticus) and Its Recovery Pattern. Appl. Sci. 2021, 11, 3332.
- Antonine, B.; Guillaume, M.; Philippe, D.; Marie-Helene, P. 2022. Low Concentrations of Glyphosate Alone Affect the Pubertal Male Rat Meiotic Step: An in Vitro Study. Toxicol. In Vitro 2022, 79, 105291.
- Meshkini, S.; Rahimi-Arnaei, M.; Tafi, A.A. The Acute and Chronic Effect of Roundup Herbicide on Histopathology and Enzymatic Antioxidant System of Oncorhynchus Mykiss. Int. J. Environ. Sci. Technol. 2019, 16, 6847–6856.
- Ludwig-Borycz, E.; Guyer, H.M.; Aljahdali, A.A.; Baylin, A. Organic Food Consumption Is Associated with Inflammatory Biomarkers Among Older Adults. Public Health Nutr. 2021, 24, 4603–4613.
- Nankongnab, N.; Kongtip, P.; Tipayamongkholgul, M.; Bunngamchairat, A.; Sitthisak, S.; Woskie, S. Difference in Accidents, Health Symptoms, and Ergonomic Problems Between Conventional Farmers Using Pesticides and Organic Farmers. J. Agromed. 2020, 25, 158–165.
- Wesseling, C.; Mcconnell, R.; Partanen, T.; Hogstedt, C. Agricultural Pesticide Use in Developing Countries: Health Effects and Research Needs. Int. J. Health Serv. 1997, 27, 273–308.
- Uram, C. International Regulation of The Sale and Use of Pesticides. Nw. J. Intl L. Bus. 1989, 10, 460.
- Phung, D.T.; Connell, D.; Miller, G.; Rutherford, S.; Chu, C. Pesticide Regulations and Farm Worker Safety: The Need to Improve Pesticide Regulations in Viet Nam. Bull. World Health Organ. 2012, 90, 468–473.
- Vanlaeys, A.; Dubuisson, F.; Seralini, G.-E.; Travert, C. Formulants of Glyphosate-Based Herbicides Have More Deleterious Impact Than Glyphosate on Tm4 Sertoli Cells. Toxicol. In Vitro 2018, 52, 14–22.
- Cayir, A.; Coskun, M.; Coskun, M.; Cobanoglu, H. Comet Assay for Assessment of Dna Damage in Greenhouse Workers Exposed to Pesticides. Biomarkers 2019, 24, 592–599.
- Meltzer, G.; Avenbuan, O.; Wu, F.; Shah, K.; Chen, Y.; Mann, V.; Zelikoff, J.T. The Ramapough Lunaape Nation: Facing Health Impacts Associated with Proximity to A Superfund Site. J. Community Health 2020, 45, 1196–1204.
