Biliary atresia (BA) is a progressive fibro-obliterative process with a variable degree of inflammation involving the hepatobiliary system. Its consequences are incalculable for the patients, the affected families, relatives, and the healthcare system. Scientific communities have identified a rate of about 1 case per 10,000–20,000 live births, but the percentage may be higher, considering the late diagnoses. The etiology is heterogeneous. BA, which is considered in half of the causes leading to orthotopic liver transplantation, occurs in primates and non-primates. To consolidate any model, (1) more transport and cell membrane studies are needed to identify the exact mechanism of noxa-related hepatotoxicity; (2) an online platform may be key to share data from pilot projects and new techniques; and (3) the introduction of differentially expressed genes may be useful in investigating the liver metabolism to target the most intricate bilio-toxic effects of pharmaceutical drugs and toxins.
- biliary atresia
- liver
- congenital
- perinatal
- animal model
1. Introduction
2. Experimental Animal Models Conundrum
Some rodent models are well suited for studying mechanisms of various aspects of inflammation. Still, they have shown limited utility for translating genetic research data to human terms, thereby impeding therapeutic developments. There is a need to emphasize the need for standardization of preclinical animal models by showing the impact of duration of jaundice, sex, and methodologies. Recognizing and realizing the limitations and advantages of preclinical models will assist a more effective translation of experimental results to enhanced approaches to therapy for human BA. This neonatal cholangiopathy proceeds through several overlapping stages that unequivocally necessitate precise spatiotemporal control. It also needs contributions from multiple cell types that orchestrate the myriad of cellular processes that eventually result in BA. This extraordinary process is evolutionarily conserved and can be studied in numerous in vivo models, ranging from zebrafish to primates. Over the past several decades, the use of BA models has contributed to breakthroughs, advancing the knowledge and interpretation of the molecular and cellular events that contribute to this process. Despite advances in the biology of understanding BA, understanding the pathophysiology of acute and chronic inflammation in the developing liver is limited, resulting in a lack of successful therapies for the affected infants. Animal models that have been designed to investigate biology and preclinical mechanisms resulted in variations that have not been properly standardized and validated, creating a challenging situation. Several variables influence this already complex biologic process. They include age, sex, biliary development, metabolic pathways, and microbiome diversity. Consequently, reswearchers encounter a conundrum. On the one hand, researcherswe face the situation where the field is required to use animal models to perform preclinical investigations as a necessity for therapeutic development. On the other hand, researcherswe are often confronted with the limited predictive value of data obtained in preclinical examination for clinical implementation. It is critical to understand both the limitations and advantages of various models. Accurate experimental animal models may allow the understanding of pathophysiological mechanisms involved. Different animal species like the rat, lamprey, and rhesus monkey have been used, but murine models have been used more often. The reproduction of BA requires various strategies, including surgical methods (e.g., common bile duct (CBD) ligation), viral infection, grafting, and drug administration. ResearchersWe will describe the available animal models, their development, applications, and practical considerations for scientific usage.3. Non-Human Primates and Non-Primates Occurrence of BA
Spontaneously occurring BA-like findings have been reported in lambs, dogs, calves, and foals but have not been adopted for studies. The more investigated spontaneous BA models in animals are zebrafish, lamprey, and Rhesus monkey and animal models for BA can be subdivided in viral, surgical, toxin-based, and genetic (Figure 1).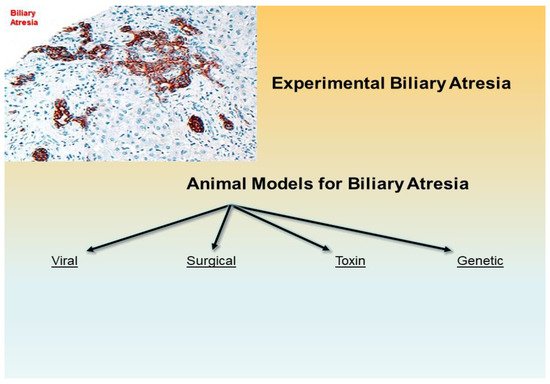
4. Zebrafish
Although distant from the human condition, the tropical freshwater zebrafish (Danio rerio) may be used as a model for studying biliary defects due to the remarkable conservation of development genes. Since the 1960s, the zebrafish model has become increasingly important to scientific research. This tropical fish native to Southeast Asia has many characteristics that make it a valuable model for studying human genetics and disease. The complete genomic sequence of the zebrafish was published in 2013, and its genome reaches 1,505,581,940 base pairs in length (26,247 protein-coding genes) [36][37][38][36,37,38]. The notch pathway, which is essential in mammalian biliary development, also regulates the specification of liver progenitor cells towards a biliary cell fate in zebrafish [39]. In the zebrafish model of BA, the inhibition of DNA methylation leads to biliary defects and activation of interferon gamma (IFN-γ) genes. Activating the IFN-γ pathway is sufficient to cause developmental defects. Subsequently, there is a decrease in cholangiocyte proliferation and expression of vhnf1 (hnf1b, tcf2) [40][41][42][40,41,42]. In addition, BA patients show, in the cholangiocytes, a reduction of the levels of apical glypican-1 (GPC1) [43][44][45][46][47][48][49][43,44,45,46,47,48,49], a heparan sulfate proteoglycan involved in regulating hedgehog signaling. Knockdown of gpc1 in zebrafish leads to biliary defects, which can be partially reversed with cyclopamine, a hedgehog antagonist. Most recently, HNF6, ARF6, Sox17, ILF2, DNMT1 genes have been confirmed to have effects on the development of bile ducts in zebrafish [46][50][51][52][53][54][55][56][57][58][46,50,51,52,53,54,55,56,57,58]. In particular, the deletion of ilf2 determined a reduction of bile flow and defect in the biliary anatomy, which has been interpreted as a phenocopy of BA in humans. It is imperative to investigate the embryonic biliary development in Zebrafish in more detail and compare BA development as induced by virus (RRV) or toxins (biliatresone) in heterozygous/homozygous ilf2 knockout rodents to further illuminate the roles of ILF2 in the human embryonic biliary development and BA [50]. In Table 1 are detailed the most paramount animal models of biliary atresia.5. Lamprey
The Sea Lamprey (Petromyzon marinus) is a primitive, eel-like fish native to the northern Atlantic Ocean and freshwater of the Great Lakes [59][60][61][62][63][59,60,61,62,63]. The sea lamprey metamorphosis is a genetically pre-programmed animal model for BA [64][65][66][67][68][69][70][71][72][73][64,65,66,67,68,69,70,71,72,73]. The larva has a fully formed biliary system with the gallbladder, lost during the transition to the adult stage. The epithelium of the extrahepatic ducts in lamprey larvae transforms and expands into a caudal portion of the pancreas of the adult. Regression of the biliary structures is accompanied by periductular fibrosis. Although Youson initially noted these morphological similarities in 1978 [66][74][66,74], the lamprey was not adapted as an experimental BA model until recently in this century [59][64][65][67][68][69][70][71][72][73][75][59,64,65,67,68,69,70,71,72,73,75]. In human BA, the most severe injury seems to occur early in the extrahepatic tract, and the intrahepatic ducts show ductular proliferation. In the lamprey, the degenerative process is asynchronous. The more rapid decline occurs in small peripheral components, and post-metamorphosis lampreys usually grow to adult size without developing any sort of progressive disease, despite having no bile ducts. Yeh et al. reported that the sea lamprey adapts by de novo synthesis and secretion of bile salts in the intestine and reduction of bile salt synthesis in the liver [71]. According to Cai et al. [70], adult sea lamprey tolerates BA by transforming its bile salt composition from toxic C24 bile acids (petromyzonol sulfate) to less harmful C27 bile acids (3-keto-petromyzonol sulfate). It accelerates renal excretion through urine, supported by marked upregulation for organic anion and bile acid transporters. Further studies may be necessary to explore, validate, and leverage this BA model.6. Rhesus Monkey
Rhesus monkey represents a vital compromise to have an animal model that is close to humans and more feasible for surgical manipulation [76]. The only pure extrahepatic biliary atresia known in a nonhuman primate is identified in the rhesus monkey (Macaca mulatta) neonates. In 1983, Rosenberg et al. showed clinical and pathologic similarities to BA in a six-week-old female monkey [77]. Jaundice and conjugated hyperbilirubinemia at the age of six days persisted throughout life with the portal proliferation of biliary structures. The autopsy revealed biliary cirrhosis with ductular proliferation at ten months. High reovirus 3 titers in rhesus neonates’ serum were also found in human infants with BA [23][78][23,78]. In 1974, Landing first hypothesized that hepatotropic viruses play an etiologic role in BA, but numerous studies have substantially annihilated the viral hypothesis. It is important to keep in mind that no detailed studies have been performed on the rhesus neonate animal model due to the costs and difficulty in obtaining Ethics Committee approval.7. Transplantation Model
8. Virus-based Models
| Viral | Surgical | Toxin, Prenatal 1 | Toxin, Postnatal 2 | Genetic |
|---|---|---|---|---|
| gpCMV (Guinea pig): Infection-based => MNI, PC, Ch, F, BDP (Wang et al., 2011 [80][94]) |
Post natal BDL (Rabbit, lamb, rat, pig, monkey): Surgery-based => MNI, PC, Ch, F, ~ BDP (temp.) (Cameron & Oakley 1932 [81][79]) (Holder & Ashcraft 1966 [82][80]) (Morgan et al., 1966) (Spitz 1980 [83][81]) |
Phalloidin (Wistar rat): IP Administration => Canalicular Ch, ↑ Vol. peri-canalicular actin filaments (Hosoda et al., 1997 [84][101]) 1,4-phenylene-diisothio- cyanate (Wistar rat) Oral Administration => EHBDD, F, BDP (Ogawa et al., 1983 [85][112]) Monohydroxy bile acids (NZ white rabbit): IV Administration => BDO (in some offspring) (Jenner 1978 [86][102]) Biliatresone (BALB/c mouse): IP Administration => EHBD-A, MNI, F, BDP (Yang et al., 2020 [87][105]) |
Phorbol myristate acetate (Golden hamsters): GB infusion => Peribiliary PMN, F (Schmeling et al., 1991 [88][103]) |
inv mouse (OVE210 heterozygous invmutant mouse) IHBD-A (periportal), BDP, CBD patent (Shimadera et al., 2007 [89][106]) |
| RRV/HCR-3/WI-78 (BALB/c mouse): Infection -based => MNI, PC, Ch, ± F, -Atresia (Riepenhoff-Talty et al., 1993 [90][95]) |
Obliterative micro-Sx (Wistar rat): Microsurgery -based => F, BDP (zones 1 & 2) (Aller et al., 2004 [91][92][113,114]) |
Sox17 haploinsufficiency based mouse (C57BL/6 mouse) => Injury of the epithelial cells of the EHBDS, GB hypoplasia, BD stenosis/atresia (Uemura et al., 2013 [93][110]; Uemura et al., 2020 [54])) |
||
| Reo Virus 3 (mice): Infection-based => MNI, PC, Ch (Phillips et al., 1969 [94][115]) |
Transplantation (C57BL/6 and B1O.A mice): Graft-based (Fetal/perinatal renal subcapsular allografts in adult congenic mice) => Fibrosclerosis (Schreiber et al., 1992 [79][89]) |
Pkhd1-Nonobese diabetic (NOD) mouse (NOD.Abd3) => MNI, BDP (Huang et al., 2018 [95][111]) |
||
| Rotavirus Reassortant–Induced Model (RRRV: TR(VP2,VP4)) (Mouse): Infection-based => F, BDP (Mohanty et al., 2020 [96][98]) | Organ Culture (Embryonal liver culture) Cell culture-based (BD Induction in embryonic liver) (Petersen et al., 2001 [97][100]) |
