Cardiovascular disease (CVD) is one of the greatest public health concerns and is the leading cause of morbidity and mortality in the United States and worldwide. CVD is a broad yet complex term referring to numerous heart and vascular conditions, all with varying pathologies. Macrophages are one of the key factors in the development of these conditions. Macrophages play diverse roles in the maintenance of cardiovascular homeostasis, and an imbalance of these mechanisms contributes to the development of CVD. Here we provide an overview of the diversity of macrophages, their roles in maintaining tissue homeostasis within the heart and vasculature, and potential mechanisms through which macrophages may be targeted in the treatment of CVD.
1. Introduction
Cardiovascular disease (CVD) encompasses a constellation of pathologies and diseases, including atherosclerosis, heart failure, cardiomyopathy, valvular heart disease, and arrhythmia. Despite vast research efforts and public health campaigns, CVD remains the world’s largest cause of mortality, accounting for nearly one-third of health-related deaths in the United States and other major countries
[1][2][3][1,2,3]. Lifestyle, diet, and metabolic dysfunctions are well known to be the primary risk factors of CVD, and have been found to increase the prevalence of comorbidities such as obesity, hypertension, and hyperglycemia, as well as dyslipidemia
[4][5][4,5]. Other biological factors have also been linked to an increased risk of CVD. Vascular calcification, which is often associated with chronic kidney disease (CKD), has been shown to worsen atherosclerosis and increase the risk of cardiac events, including heart attack and stroke, which has also made it a valuable predictor of CVD
[6][7][8][6,7,8]. The unifying element among all of these risk factors is the increased presence of arterial and tissue inflammation, while the increased presence of pro-inflammatory markers in circulation is often associated with CVD and decreased tissue regeneration
[9][10][9,10]. It is important to understand the body’s natural regulation of tissue inflammatory responses to gain better insight into the possible effective treatments of CVD conditions.
The inflammatory responses within tissues are now better understood to be a regulated and balanced process between the activity of macrophages in both the tissue itself as well as the blood circulation
[11][12][11,12]. Macrophages are immune system cells that are known for their defense against infectious pathogenic agents, as well as their maintenance of homeostasis in tissue that has been damaged during disease
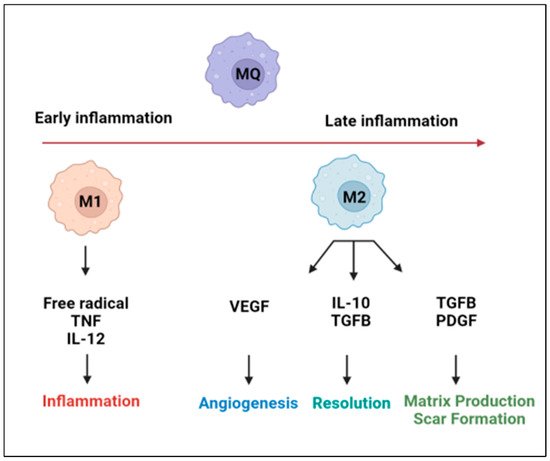
[12]. Traditionally, macrophages were defined based on their inflammatory activity, which categorized them as either M1 pro-inflammatory macrophages or M2 anti-inflammatory macrophages (
Figure 1). M1 macrophages can induce inflammatory responses in tissue through the secretion of pro-inflammatory cytokines and the recruitment of other inflammatory stimulating cells. In contrast, the M2 macrophages relieve inflammation through the signaling apoptosis of affected cells and by activating anti-inflammatory processes
[12][13][12,13]. Although this simplified classification remains true, it does not consider the varying plasticity of macrophages, which have been shown to possess a variety of phenotypic characteristics depending on the resident tissue and the disease that is present. Both past and recent studies have also relied on the usage of electron microscopy to visualize macrophages and identify specific cell surface receptors that provide insight into their function
[14][15][14,15]. It is now better understood that macrophages display specialized functions that work to maintain homeostasis in their resident tissues and to offset the effects of tissue-damaging pathologies.
Figure 1. Schematic illustrating the inflammatory signaling mechanisms and the regulation of macrophages during early and late phases of inflammation. M1 macrophages are highly phagocytic and produce large amounts of pro-inflammatory mediators, whereas M2 macrophages produce large amounts of anti-inflammatory mediators and support angiogenesis and tissue repair. Created with
BioRender.com.
2. Targeting Macrophages in the Treatment of CVD
Many of the potential macrophage-centered treatment options for CVD target pro-inflammatory cytokines that relate to macrophage-induced disease processes. The inhibition of IL-1β is a target being explored. IL-1β has been shown to promote the development of atherothrombotic plaque and macrophage adhesion
[16][135]. In a study of 10,000 patients with histories of MI, the monoclonal anti-body drug canakinumab, which blocks the pathway of IL-1β, showed a significant reduction in cardiovascular events over a median follow-up period of 3.7 years
[16][135]. The inhibition of IL-1β by canakinumab led to a reduction in heart-failure-related mortality in patients who had prior MI and active inflammation
[17][18][136,137]. Another study found that the canakinumab treatment resulted in a dose-dependent 25% reduction in hospitalizations related to HF when treated with 300 mg canakinumab every three months
[17][136]. IL-1β inhibition can offer a new approach to the treatment of HF that does not alter the blood pressure or renal function in a clinically significant way. Other therapeutic targets related to macrophage IL-1β expression include Rac-2-mediated pathways that play a role in atherosclerosis; however, no treatments have been developed for this target to date
[19][138].
Interleukin-1 receptor blockade with anakinra preserves the LV systolic function after acute MI and attenuates systemic inflammation
[20][46]. Anakinra may have a use in both HFrEF and HFpEF
[20][46]. Anakinra demonstrated an improvement in peak aerobic exercise capacity and re-hospitalization of patients with heart failure (HF) when received for 12 weeks’ duration in comparison to treatment for 2 weeks’ duration or placebo
[21][139]. This difference was not statistically significant but has created interest in exploring the IL-1 receptor blockade as a potential treatment option
[21][139]. The left ventricular ejection fraction was also shown to increase with IL-1 blockade when compared to placebo-treated patients
[22][140].
Interleukin-6 is produced by many cells in the cardiovascular system, including macrophages. IL-6 could also prove to be a promising therapeutic target. The IL-6 inhibitor tocilizumab was able to reduce the levels of pro-B-type natriuretic peptide in patients with rheumatoid arthritis and no CVD, implying that the drug may have cardioprotective properties
[23][141]. Additionally, non-STEMI patients showed attenuated troponin T release and reduced systemic inflammation in the presence of tocilizumab, yet again demonstrating that IL-6 blockade’s effects may need to be further explored
[24][142]. The blockade of IL-6 needs to further be explored in CVD. A further exploration of macrophage-expressed CCL2/CCR2 should also be considered
[20][25][46,143]. The inhibition of CCL2/CCR2 raises concerns due to the macrophages’ role in both pro- and anti-inflammatory processes
[18][137]. It is important to find ways to selectively discourage pro-inflammatory M1 macrophages, while encouraging M2 anti-inflammatory macrophage actions in the treatment of CVD processes
[26][27][144,145].
Aside from interleukin-based strategies to target macrophages, other molecular pathways have had some success as well in various etiologies of CVD. The inhibition of protein phosphatase and tensin homolog (PTEN) with a vanadium-based compound called “VO-Ohpic” has been shown to attenuate inflammatory M1 macrophages and increase anti-inflammatory M2 macrophages, improving cardiac function in doxorubicin-induced cardiomyopathy
[27][145]. Targeting cytokine MCP-1 may be a way to attenuate the M1 macrophage response in patients with dilated and uremic cardiomyopathy
[28][146]. Baicalin, a plant-based anti-inflammatory flavonoid, has shown benefit in changing the macrophage phenotype from M1 to M2 in the treatment of CVD
[29][120]. Additionally, another anti-inflammatory agent salvianolic acid B (SalB) has been shown to increase M2 macrophages and decrease M1 macrophages at 3 days, which was followed by reduced cardiac dysfunction at 7 days in a post-myocardial infarction mouse model
[30][147].
The reduction in all macrophages was protective against myxomatous valvular disease progression in mouse models
[31][148]. Refametinib and doxycycline were shown to reduce macrophage infiltration in mouse models with latent aortic valve disease, slowing its progression
[28][146]. Evogliptin, an inhibitor of the enzyme dipeptidyl peptidase-4, was shown to attenuate aortic valve calcification through a reduction in pro-inflammatory cytokines (Il-6, IL-1, TNF-alpha) and the inhibition of macrophage infiltration in a rabbit model
[32][149]. Evogliptin has also been shown to be useful as an anti-atherosclerosis therapy via its ability to inhibit vascular inflammation
[33][150]. Studies using mouse models demonstrated that macrophage depletion by IV clodronate liposomes inhibited the development of hypertension, consequently reducing left ventricular hypertrophy, cardiac fibrosis, and cardiac remodeling
[34][151]. Future trials are needed to explore the effects of denosumab and bisphosphonates on pro-inflammatory cytokines that lead to the development of calcific aortic valve disease
[26][144].
The use of cardiosphere-derived cell (CDC) exosomes has proven to have some benefit for CVD in porcine and rat models. One study demonstrated a decrease in acute ischemic reperfusion injury and a decrease in chronic post-MI remodeling
[35][152]. A two-fold reduction in macrophages was noted and groups that were treated with CDCs had lower left ventricular diastolic pressure, decreased lung congestion, and enhanced survival
[35][152]. Clinical trials are underway testing the use of CDCs for the prevention of CVD
[35][152]. The blockade of TNF-alpha with ethanercept and infliximab in HFrEF patients has been explored, and did not show any promise due to the complicated relationship between TNF-alpha and macrophages
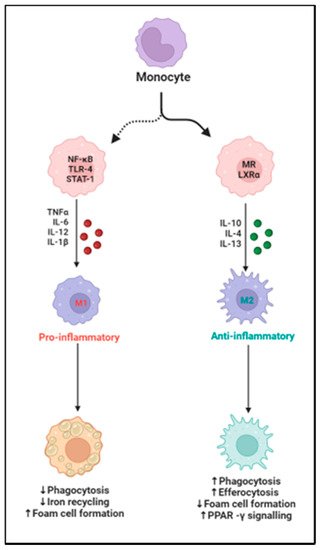
[18][20][46,137]. Macrophages and their associated pro-inflammatory cytokines are promising therapeutic targets that warrant further study in the treatment of CVD (
Figure 24).
Figure 24. Schematic illustrating macrophage polarization to proinflammatory M1 and to an anti-inflammatory M2 phenotype and the specific factors affecting the process, up arrows mean increased levels, and down arrows refer to decreased levels. Created with
BioRender.com.