Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Sirius Huang and Version 3 by Sirius Huang.
Nitrogen oxides (NOx) are gaseous pollutants contributing to pollution in their primary form and are also involved in reactions forming ground-level ozone and fine particulate matter. Thus, NOx is of great interest for targeted pollution reduction because of this cascade effect. To achieve a holistic understanding of the correlation between NOx and human health, both the physical and mental health implications must be accounted for. The following content is intended to be illustrative in nature, and not exhaustive of all research conducted in the field.
- air pollution
- air quality
- mental health
- nitrogen oxides
- NOx
- physical health
1. Nitrogen Oxides (NOx) as a Targeted Pollutant
NOx is a ubiquitous pollutant due to its numerous sources (mainly from stationary and mobile fossil fuel combustion but also from natural causes such as lightning), its potential to be both a primary and secondary pollutant, and its documented impacts on human health.
NOx occurs primarily in one of two forms: nitric oxide (NO) and nitrogen dioxide (NO2). NO is generally emitted as a primary pollutant, which photochemically reacts with free radicals in the atmosphere to form NO2 [1][2]. There are instances where NO2 is emitted as a primary pollutant, but more often than not, it occurs as a result of pre-existing NO [3]. The rate of secondary oxidation of NO into NO2 depends on the solar radiation intensity, humidity, concentration, availability of free radicals, and airflow in the region of concern [4]. When no information is not provided, it can be assumed that the NO2 concentration is essentially equivalent to the NOx concentration, since any NO in the atmosphere reacts quickly to form NO2 [1][2].
NO and NO2 can rapidly cycle back and forth in the atmosphere on a minute-by-minute timescale [5]. NOx is regarded as a short-lived air pollutant with an atmospheric lifetime on the order of a day [5], although this is typically shorter in the summer (<6 h [6][7]) due to higher ozone concentrations [7]. NO2 buildup in the atmosphere can be visually seen hanging over many large urban centres as a brown haze on the horizon.
In some instances, nitrous acid (HONO) is also generated [4]. Water molecules in the atmosphere are able to dissolve the ambient NO2 to form acidic compounds contributing to acid rain, putting ecosystems at risk of acidification. Additionally, NO2 can be absorbed directly by plants causing damage or death of tissue, which can impact plant growth and yield [8].
NOx, while a significant environmental pollutant on its own, also acts as a precursor for other air pollutants. NOx typically resides close to ground level in urban environments and, through a complex set of reactions, can react to form both ground-level ozone (O3) and fine particulate matter (PM2.5) in the form of secondary organic and inorganic aerosols (SOAs and SIAs, respectively). This, in turn, contributes to smog formation [9][10][11][12]. These reactions are cyclical in nature and can result in a buildup of NOx and O3 at ground level. There is typically a lag time between when the concentration of NOx increases (during morning and evening rush hours) and when the concentration of O3 increases (mid-morning and into the afternoon during peak solar intensities) [11].
2. Physical Health Impacts of NOx
The main route of NOx exposure for humans is via inhalation, during which 80–90% is absorbed into the body through the respiratory tract. Nitrogen oxides, both NO and NO2, are readily absorbed into the bloodstream through the respiratory tract. Once in the bloodstream, NO reacts quite quickly, on the order of three seconds, with O2 to generate NO2. NO2 can further react in the bloodstream, as it is a water-based environment. Highly reactive NO2 generates superoxide and alloxy radicals, and the ensuing nitrogen anion imbalance contributes to lipid peroxidation [13].
NO occurs naturally in the bloodstream and has essential physiological functions in the human body, including acting as a vasodilator and signalling molecule. Blood concentrations above what is considered normal trigger inflammatory responses [13][14][15][16][17].
Exposure to NO also directly affects the nitric oxide synthase (NOS) activity, generally found in the intercellular fluid or in membranes of blood vessels and can trigger changes to the respiratory system and cellular respiration leading to the formation of reactive oxygen species (ROS). The presence of ROS in the respiratory tract and lung parenchyma result in sensitive tissue damage, such as augmentation of pulmonary permeability, increased mucus secretion, damage to fatty bronchial epithelium, and damage of surfactant properties. Chronic exposure directly causes the inflammation of tracheal mucosa and is often expected to be observed with irritation of the conjunctiva and ulceration of the nasal cavity [13]. Moreover, within the human body, NO can act as a vasodilator of cerebral blood vessels, causing cytotoxic activities in the immune system, as well as acting as neurotransmitter. Within the brain, neurons produce NO during their function and, when the NO and NO-synthase equilibrium is imbalanced, this can disrupt the cerebral blood flow and brain activity connection [14].
Nitrosation is the primary indirect impact of enhanced NO in the bloodstream and leads to the formation of nitrosamines. These byproducts damage DNA leading to carcinogenesis processes as well as chronic inflammation. Another NO reaction byproduct is superoxide nitrates, strong oxidizers responsible for inflammation and lipid peroxidation, with subsequent damage to cells and tissues throughout the body [13][14][15][16][17].
The first signs of NOx exposure are generally nose and throat irritation. If exposure persists, these symptoms can progress to bronchoconstriction and dyspnea (difficult and laboured breathing), especially in individuals who suffer from asthma [1]. Symptoms can worsen and develop into bronchitis, reduced lung function, and increased susceptibility to other respiratory developments [18]. Continued direct exposure to NOx can lead to increased sensitivity to respiratory infections, allergic reactions, childhood asthma, lung cancer, cardiovascular and respiratory diseases, and potential reproductive impacts [1][8][19]. These impacts can lead to increased risk for hospital emergency room visits, hospital admissions, and mortality.
Table 1 summarizes the more specific health effects resulting from both acute and chronic NOx exposure, specifically for NO2, along with the risk ratio (where available) that represents the increased risk associated with a 10 μg·m−3 increase in concentrations of NO2. It is evident, based on the literature, that exposure to NO2 has numerous adverse health effects, many of which can be severe in nature if left untreated. In addition, many of these health effects are confounded by the simultaneous exposure to O3 and PM2.5, of which NOx is a precursor gas.
Table 1. Human physical health effects linked to NO2 exposure.
| Health Effect Resulting from NOx Exposure | Exposure Duration | Risk Ratios (Per 10 μg·m−3 Increase in NO2 Exposure) | References | ||||||
|---|---|---|---|---|---|---|---|---|---|
| General | Diabetes | Chronic | 1.23 | [20] | |||||
| High Blood Pressure | Chronic | 1.01 | [20] | ||||||
| Headache | Chronic | 1.13 | [20] | ||||||
| Physical Symptoms | Chronic | 1.23 (1.02, 1.39)* for NO2 | Stroke | Chronic | 1.01 | [20] | |||
| 1.22 (1.02, 1.38)* for NO | x | ||||||||
| Self-Rated Health | Chronic | 1.15 (0.94, 1.32)* for NO2 1.13 (0.93, 1.30)* for NOx |
Nose and Throat Irritation | Acute | [1] | ||||
| Chronic | 1.07 (1.05, 1.10)* per IQR | 23.4 | [67] | Increased sensitivity and susceptibility to respiratory illness and disease | Chronic | [1][3][8][ | |||
| Chronic | 18 | ] | [19][21] | ||||||
| 0.95 (0.39, 1.31)* highest vs. lowest tertile range | 34.64 | [ | 68] | Respiratory Illness | Chronic | [17] | |||
| Psychological Distress | Chronic | Positive, statistically significant relationship with NOx | [69] | Chest Colds, Chronic Cough and Wheezing, Chest Cough | Acute and Chronic | ||||
| Mental Health Service Use | Chronic | 1.32 (1.25, 1.38) per IQR for NO2 1.31 (1.24, 1.37) per IQR for NOx | [8][15][17][22][23][24] | ||||||
| 40.2 (NO | 2 | ) | 71.1 (NOx) |
[70] | Dyspnea | Chronic | [1] | ||
| Hospital Admissions | Acute | 1.17 (1.00, 1.36) | 56.75 | [71] | Reduced Lung Function | Acute and Chronic | [8][15][18][23] | ||
| Hospital Admissions | Acute | 1.0188 (−0.40,4.16) for 1-day lag, moving average concentration | 46 | [72] | Bronchitis and Bronchitis Symptoms | Chronic | 1.021 | [1 | |
| Hospital Admissions | Chronic | 1.18 (1.05, 1.34) per IQR for NO2 1.18 (1.05, 1.34) per IQR for NOx | ][2][17][18][25][ | 40.2 (NO226) 71.1 (NOx][27][28] |
|||||
| ) | [ | 70 | ] | Allergic Reactions | Chronic | [1][8][19] | |||
| Emergency Room Visits | Chronic | 1.02 (−0.6, 4.6) | [73] | Inflammatory Responses | Chronic | [2][13][14][15][16][17][22][26] | |||
| Acute | 1.0494 (1.0203, 1.0792) per IQR | 39.8 | [74] | Potential Reproductive Impacts | Chronic | ||||
| Acute | 1.0377 (1.0278, 1.0478) | [1] | 32.79–53.23[8] | [75[19] | |||||
| ] | Cell Damage | Chronic | [2][13][14][15][16][17][22][26] | ||||||
| Cardiovascular Disease (CVD) | Chronic | 1.04–1.22 | [1][3][8][19][21][29][30][31][32][33] | ||||||
| Respiratory Disease | Chronic | [1][2][3][8][19] | |||||||
| Asthma | |||||||||
| Acute | 0.9966 (0.9873, 1.0061) per IQR | 23.57 | [76] | ||||||
| Acute | 1.0445 (1.0290, 1.0604) | 24.69 | [77] | ||||||
| Acute | 1.0794 (1.0628, 1.0962) | 30.13 | [77] | Chronic | 1.05–1.5 | [1][8] | |||
| Acute | [ | 19 | ][20][ | 1.0219 (0.0051, 1.0389)22][24][34][35][36] | |||||
| 33.35 | [ | 77 | ] | Hospital Admissions | General | Acute and Chronic | 1.01 | ||
| Psychosis Mortality | Acute | 1.0010 (0.9999, 1.0021) | 18.7 | [25] | [78[27][28][37][38] | ||||
| ] | Emergency Room | Chronic | |||||||
| Sleep | 1.1 | Low Sleep Efficiency | [3] | Chronic[39] | |||||
| 1.16 (1.07, 1.25)* | 27.82 | [ | 79 | ] | Stroke | Chronic | 1.14 | [40 | |
| Sleep Apnea | ] | ||||||||
| Chronic | 1.28 (1.03, 1.47)* | 27.82 | [ | 79] | Asthma | Acute and Chronic | 1.001–1.27 | [13][38] | |
| Sleep Disorder | Chronic | [ | 1.11 (1.02, 1.19)* per IQR40] | ||||||
| 36.78 | [ | 80 | ] | Respiratory Ailments | Chronic | 1.009–1.05 | [38][40][41][42] | ||
| Respiratory Disease | Acute | 1.018 | [ | ||||||
| Sleep Disorder | Chronic | 1.17 (0.77, 1.44)* highest vs. lowest tertile range | 34.64 | [68]25][28] | |||||
| Anxiety | Anxiety Disorder | Chronic | 1.09 (0.90, 1.25)* | 27.5 | [21] | Chronic Obstructive Pulmonary Disease (COPD) | Acute | [13] | |
| Chronic | 1.34 (0.85, 1.62)* highest vs. lowest tertile range | 34.64 | [68] | Blood Poisoning | Acute | [13] | |||
| Medication Use | Chronic | 1.21 (0.90, 1.44)* for NO2 1.13 (0.89, 1.32)* for NOx |
57.3 | [ | Cardiovascular-Circulatory System Disease | Chronic | 1.05 | [40] | |
| 81 | ] | ||||||||
| Hospital Admissions | Acute | 2.23 (1.02, 4.91) | 56.75 | [71] | Cardiovascular-Myocardial Infraction | Chronic | 1.15 | [40] | |
| Emergency Room Visits | Acute | 1.0342 (1.0210, 1.0475) | 32.79–53.23 | [75] | Cancer-Lung | Chronic | 1.2 | [40 | |
| Acute | ] | ||||||||
| 1.0506 (1.0233, 1.0786) | 24.69 | [ | 77] | Cancer-Kidney | Chronic | 1.2 | [40] | ||
| Acute | 1.0740 (1.0545, 1.0938) | 30.13 | [77] | Cancer-Other | Chronic | 1.06 | [40] | ||
| Acute | 1.0429 (1.0217, 1.0645) | 33.35 | [77] | Cancer | Lung | Chronic | |||
| Depression | 1.12 | Depressive Symptoms | Chronic | 1.50 (1.27, 1.67)* per 10 μg·m−3 increase NO2 1.38 (1.18, 1.53)* per 20 μg·m−3 increase NOx[1][8][19][34][43][ |
57.3 (NO244][45][46][47][48] | ||||
| ) | 92.8 (NO | x | ) | [81] | Brain | Chronic | [34][49] | ||
| Cervical | Chronic | [34][49] | |||||||
| Breast | Chronic | ||||||||
| Chronic | 1.33 (1.27, 1.39)* for highest quartile exposure | [82] | [34][44 | ||||||
| Acute | 1.25 (1.11, 1.36)* | 36.2 | [83] | ][49] | |||||
| Acute | 1.24 (0.99, 1.43)* per IQR | 31.4 | [84 | Prostate | Chronic | [44] | |||
| ] | |||||||||
| Chronic | 1.24 (1.06, 1.39)* | 11.7–18.8 | [85] | Premature Mortality | All-Cause | Acute | |||
| Chronic | 1.35 (1.07, 1.52)* for NO2 1.27 (0.94, 1.50)* for NOx | 1.003–1.016 | 25.9 (NO2) 39.6 (NOx) |
[86][19][28][50] | |||||
| All-Cause | Chronic | 1.003–1.06 | [2][3][25][27][28][50][51][52][53][54][55] | ||||||
| Chronic | 1.05 (0.98, 1.11)* for NO2 1.05 (0.99, 1.09)* for NOx |
[65] | Cardiovascular | Chronic | 1.004–1.03 | [31][50][51] | |||
| Medication Use | Chronic | 1.03 (1.00, 1.05)* per IQR | 23.4 | [67] | Respiratory | Chronic | 1.004–1.03 | [2][50][51][56][57][58] | |
| Lung Cancer | Chronic | 1.05 | [19][51] | ||||||
| Coronary Heart Disease | Chronic | 1.05 | [51] | ||||||
| COPD | Chronic | 1.03 | [51] | ||||||
| Pneumonia | Chronic | 1.08 | [51] | ||||||
| Diabetes | Chronic | 1.04 | [51] | ||||||
While NOx, O3, and PM2.5 have individual health impacts [59], they coexist in the ambient atmosphere; hence, it is not possible to allocate the health impacts, or portions of the impacts, to one specific pollutant outside of a controlled laboratory setting. Based on the medical evidence to date, the WHO has established annual and 24-h mean NO2 exposure limits of 10 μg·m−3 and 25 μg·m−3, respectively [60]. Prior to 2021, the annual limit was set at 40 μg·m−3. These limits are guidelines, and many countries impose their own regulations, having not yet adopted the new WHO guidelines. In Canada, for example, the current annual and 1-h NOx exposure levels are 35 μg·m−3 and 123 μg·m−3, respectively. These limits are scheduled to be reduced to 25 μg·m−3 and 86 μg·m−3, respectively, in 2025 [8].
3. Mental Health Impacts of NOx
The mental health impacts of NOx are not as established as the physical health effects of NOx and appear to have become a major focus of research after approximately 2015. This date coincides with the emergence of a worldwide societal focus on the mental health of the population and has been a focus over the past decade [61]. Mental health has been identified in the UN Sustainable Development Goals and focuses on promoting wellbeing among global citizens [62].
Mental health is an integral part to the overall wellness of an individual and, when not cared for properly, can also contribute to detrimental physical health impacts. A recent study at the University of Washington [63] found that the prevalence of mental health disorders increased at a rate of approximately 9,876,000 cases per annum between 2000 and 2019. This means that in 2020 there were be over 976 million people, 12.6% of the world’s population, with a mental health disorder. With the high ever-increasing prevalence of mental health disorders and with air pollution being a ubiquitous challenge significantly impacting physical health, the question becomes how does air pollution, specifically NOx, impact mental health?
The evaluation of the over thirty five longitudinal studies and reviews presented herein in Table 2 found that, in all cases, air pollution was mapped to NO2 exposure (NOx levels were sometimes also included). Any OR from studies were converted to RR, and the data converted from ORs are clearly indicated. The mental health concerns investigated included common mental disorders (CMD), sleep apnea, anxiety, depression, and suicide. Sleep apnea was included in the research because of its strong association with the occurrence of many psychopathological conditions, including psychological distress, anxiety, depression, and suicidal ideation [64]. Most commonly, researchers collected data based on emergency room visits, though other metrics were used to quantify mental health impacts including self-reported assessments, medication use, hospital admissions, and number of deaths. The work was primarily collected on adults of all sexes, over numerous years, and spanning multiple seasons.
Table 2. Human mental health effects linked to NO2 exposure.
| Category | Symptom | Exposure Duration | Risk Ratio (95% CI) per 10 μg·m−3 Increase in NO2 (Unless Otherwise Specified) *-Calculated from OR |
Mean NO2 Exposureug μg·m−3 | Reference |
|---|---|---|---|---|---|
| Common Mental Disorders (CMD) |
CMD | Chronic | 1.35 (1.26, 1.35)* for NO2 1.23 (1.19, 1.27)* for NOx |
[65] | |
| CMD | Chronic | 1.28 (1.05, 1.46)* for NO2 1.27 (1.04, 1.45)* for NOx |
35.8–39.6 (NO2) 57.0–67.4 (NOx) |
[66] | |
| Depressive Disorder | |||||
| Chronic | |||||
| 1.13 (0.95, 1.28)* | |||||
| 27.5 | |||||
| [ | |||||
| 21 | |||||
| ] | |||||
| Chronic | |||||
| 1.05 (0.86, 1.20)* per 188 μg·m | |||||
| −3 | |||||
| -30 days before indexing date | |||||
| 46 | |||||
| [ | |||||
| 87 | |||||
| ] | |||||
| Chronic | |||||
| 1.05 (0.78, 1.21)* per 188 μg·m | |||||
| −3 | |||||
| -365 days before indexing date | |||||
| 46.1 | |||||
| [ | |||||
| 87 | |||||
| ] | |||||
| Acute | 1.04 (0.99, 1.08)* per IQR | 34.78 | [88] | ||
| Chronic | 1.37 (0.99, 1.60)* highest vs. lowest tertile range | 34.64 | [68] | ||
| Major Depressive Disorder | Chronic | 1.14 (0.72, 1.41)* highest IQR for NO2 1.30 (0.96, 1.53)* highest IQR for NOx |
26.04 (NO2), 35.19 (NOx)–mean 39.85 (NO2), 59.71 (NOx)–Q4 | [89] | |
| Emergency Room Visits | Acute | 1.039 (1.013, 1.066)-Cold Season 1.066 (1.012, 1.124)-Warm Season |
41.17 | [90] | |
| Acute | 1.10 (1.066, 1.136) per 20.1 ppb NO2-All Season 1.20 (1.133, 1.272) per 20.1 ppb NO2-Warm Season 1.064 (1.021, 1.108) per 20.1 ppb NO2-Cold Season |
37.79 | [90] | ||
| Acute | 1.03 (0.98, 1.04)*-Warm Season, Male 1.03 (1.00, 1.05)*-Warm Season, Female |
22.18 | [91] | ||
| Acute | 1.0369 (1.0224, 1.052) | 32.79–53.23 | [75] | ||
| Acute | 1.08 (1.03, 1.12)* | [92] | |||
| Acute | 0.9875 (0.9704, 1.0049) per IQR | 23.57 | [76] | ||
| Acute | 1.36 (0.44, 2.28) | 48.5 | [93] | ||
| Acute | 1.0494 (1.0270, 1.0723) | 24.69 | [77] | ||
| Acute | 1.0802 (1.0623, 1.0984) | 30.13 | [77] | ||
| Hospital Admissions | Acute | 1.18 (0.55, 2.53) | 56.75 | [71] | |
| Acute | 1.0178 (1.0073, 1.0283)-1-day Lag | 34.6 | [94] | ||
| Suicide | Emergency Room Visits | Acute | 1.112 (1.006, 1.228) All Seasons, Male, 1-day Lag 1.239 (1.078, 1.424)-Cold Season, Male, 1-day Lag |
36.47 | [95] |
| Acute | 0.9990 (0.9730, 1.0258) per IQR | 23.57 | [76] | ||
| Risk of Death by Suicide | Chronic | 1.33 (1.09, 1.64) | 48.20 | [96] | |
| 1.39 (1.03, 1.87)-for individuals with pre-existing physical or mental disease | 48.20 | [96] | |||
| Acute | 1.06 (1.01, 1.12)*-All Gender, Under 30 years old, 0-day Lag 1.04 (1.00, 1.08)*-All Age, Warm Season, 0-day Lag |
68.94 | [97] | ||
| Acute | 1.019 (0.999, 1.039)-0–1 day Lag | [98] | |||
| Acute | 1.0057 (1.0023, 1.0081) | 18.7 | [78] | ||
| Completed Suicide | Acute | 1.17 (1.04, 1.29)*-all 1.26 (1.09, 1.40)*-Spring and Fall Transitions | [99] | ||
| Alzheimer’s Disease | Hospital Admissions | Chronic | 1.06 (0.96, 1.17) | 26.2 | [40] |
| Parkinson’s Disease | Parkinson’s Disease | Chronic | 1.08 (0.94, 1.24) | 26.2 | [40] |
All studies found positive relationships between NO2 exposure and mental health disorders, and all but twelve of the 66 relationships were statistically significant to at least the p < 0.05 significance level. Depending on the length of the study and the data set available, some of the studies made adjustments for the sex, season, and the lag after the exposure event. There were no distinguishable trends across the literature as to whether sex or season posed any greater risk to mental health disorders due to NO2 exposure. Studies that examined the time separation between exposure event and mental health disorder manifestation did, in general, find that there was increased risk associated with shorter time scales (i.e., a mental health disorder generally had greater risk of manifestation in a zero to one day lag from the exposure event with the risk diminishing with more time passing from the exposure event). An overall observation from the body of literature points to a positive statistically significant correlation between NO2 exposure and the mental health of the global population.
A comparison between the RR for each mental health disorder and for NO2 exposure level is presented in Figure 1. For reference, the WHO 24-h and annual mean exposure guidelines for NO2 are included on the plot. All studies had NO2 exposure concentrations that surpassed the 2021 WHO annual mean exposure guideline for NO2, and all but four exceeded the 24-h guideline. Data points are grouped based on the type of mental health disorder, and the metric used to quantify the disorder (i.e., emergency room visits, medication use, etc.) is not distinguished. The scattered nature of both data sets does not lead to any significant correlation for linking mean exposure to the level of risk of the presence of a mental health disorder. Linear trend lines were fit to the entire data set (mental health) (Equation (1)), as well subcategories with five or more data points (Equations (2)–(5)):
with RR being the risk ratio for all types of mental health disorders due to NO2 exposure, and C is the NO2 concentration (µg·m−3).
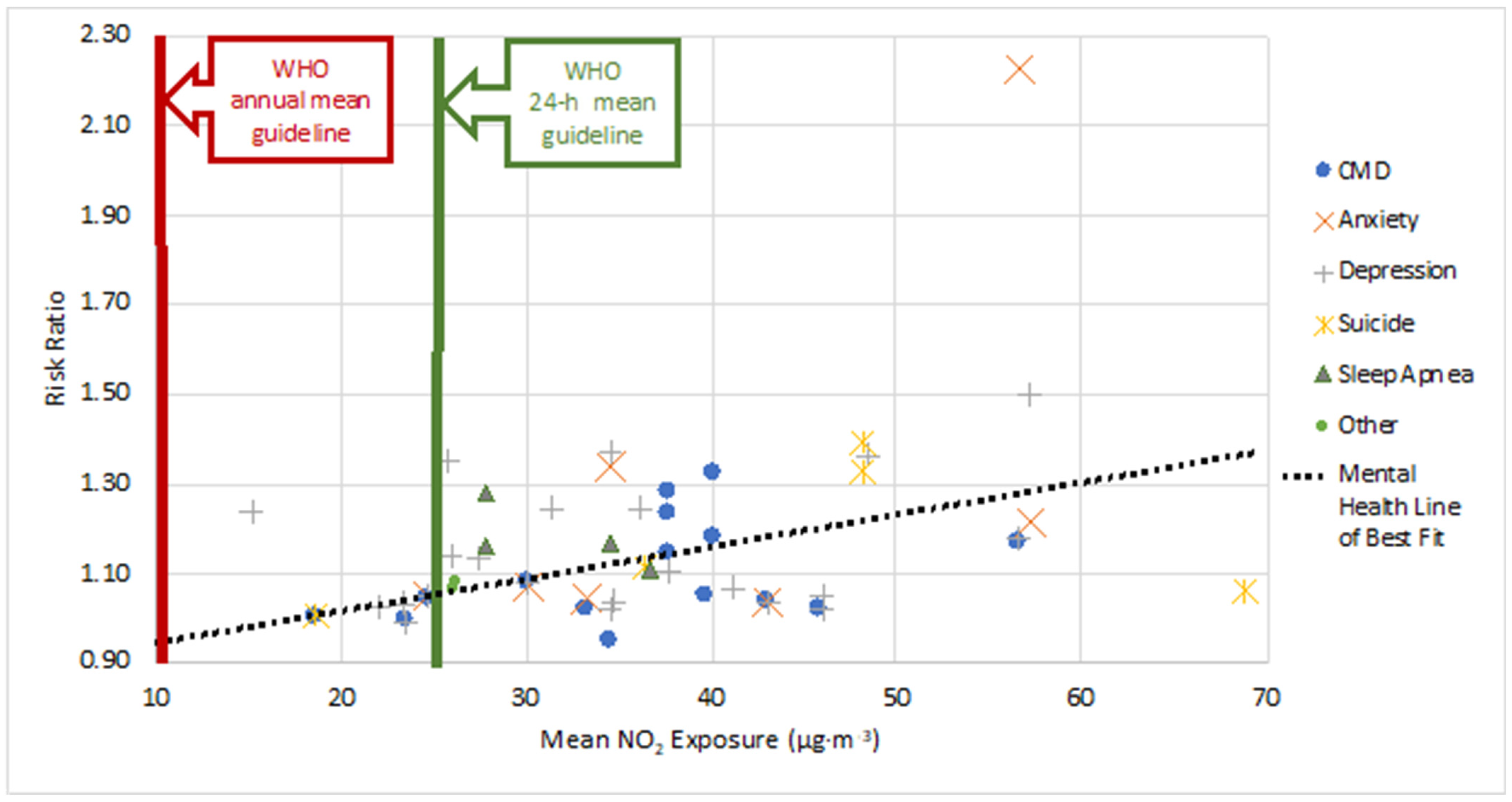
Figure 1. Risk Ratio (RR) vs. Mean NO2 exposure (µg·m−3) for different mental health disorders. This figure provides a comparison for RR and mean exposure, when both values were provided in a study. Data are plotted from each study under the broad mental health category and the actual metric used to quantify the disorder (e.g., emergency room visit, medication use, etc.) is not distinguished. Additionally, this comparison is meant to illustrate the breadth of mental health correlations, and so both acute and chronic exposure risks are grouped together under the respective mental health category. A rough linear trend line was fit to the data set, and the equation for the line of best fit leads to the observation of a positive, though weak, association between increased NO2 exposure and increased RR.
In all instances, there were positive correlations between NO2 exposure and mental health disorders, though with low correlation coefficients. Based on the trend line slopes, anxiety carries the most risk with increased NO2 exposure levels. The subcategory of ‘sleep’ only had four data points, and ‘other’ included only Alzheimer’s and Parkinson’s diseases; thus, no trend lines were generated given the limited data. Additionally, the correlation coefficients for all the linear trend lines were very low ranging from a minimum of R2 = 0.0793 to a maximum of R2 = 0.3888. One primary reason for the large degree of scatter in the plot is that the exposure duration and concentration for each study was varied. The length of exposure and fluctuations of NO2 about the mean were not well communicated in the research and, thus, not accounted for. This makes it difficult to definitively correlate the risk ratio back to a single NO2 concentration value. While the scatter of the data may not lead to a strong fit, there is a distinct trend that increasing concentration enhances the risk of an individual manifesting a mental health disorder. This positive association, coupled with the fact all studies examined exceed the WHO annual mean NO2 guideline, leads to the observation that NO2 levels in urban areas must be reduced in order to help protect the mental health of global citizens.
Figure 2 provides a geographical representation for where the studies on mental health have been conducted, in regard to NO2 exposure, on a world map by highlighting countries in blue. There is significant representation in North America, North and Western Europe, and some in Asia (mainly from China). Study gaps exist for Australia, South America, Africa, most of Asia, and Eastern Europe. Many of these regions are known to be heavy emitters of anthropogenic air pollution and are also highly populated. For example, ambient air quality in India (home to 1.4 billion people) can be extremely poor, with the capital city, Delhi, having the worst air quality in the world in 2020 [100]. Without mental health study data in these regions, any regional nuances and ramifications of NO2 exposure on mental health cannot be ascertained.
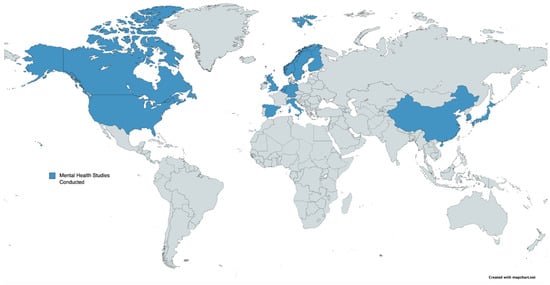
Figure 2. World map indicating (in blue) where mental health studies in relation to NO2 exposure have been conducted. There is a significant information gap in South America, Africa, Australia, Eastern Europe, and most of Asia. Many of these regions without mental health studies are high emitters of anthropogenic air pollution and are highly populated.
References
- Kampa, M.; Castanas, E. Human health effects of air pollution. Environ. Pollut. 2008, 151, 362–367.
- César, A.C.; Carvalho, J.A.; Nascimento, L.F. Association between NOx exposure and deaths caused by respiratory diseases in a medium-sized Brazilian city. Braz. J. Med. Biol. Res. 2015, 48, 1130–1135.
- Chaloulakou, A.; Mavroidis, I.; Gavriil, I. Compliance with the annual NO2 air quality standard in Athens. Required NOx levels and expected health implications. Atmos. Environ. 2008, 42, 454–465.
- Zouzelka, R.; Rathousky, J. Photocatalytic abatement of NOx pollutants in the air using commercial functional coating with porous morphology. Appl. Catal. B-Environ. 2017, 217, 466–476.
- Jacob, D.J. Introduction to Atmospheric Chemistry; Chapter 11: Oxidizing Power of the Atmosphere; Princeton University Press: Princeton, NJ, USA, 1999; pp. 199–219.
- Liu, F.; Beirle, S.; Zhang, Q.; Dörner, S.; He, K.; Wagner, T. NOx lifetimes and emissions of cities and power plants in polluted background estimated by satellite observations. Atmos. Chem. Phys. 2016, 16, 5283–5298.
- Shah, V.; Jacob, D.; Li, K.; Silvern, R.; Zhai, S.; Liu, M.; Lin, J.; Zhang, Q. Effect of changing NOx; lifetime on the seasonality and long-term trends of satellite-observed tropospheric NO2; columns over China. Atmos. Chem. Phys. Discuss. 2019, 670, 1–23.
- Canadian Council of Ministers of the Environment. 2017 Air Quality, Canadian Ambient Air Quality Standards (CAAQS). Available online: http://airquality-qualitedelair.ccme.ca/en/ (accessed on 20 January 2021).
- Bélanger, D.; Berry, P. Human Health in a Changing Climate: A Canadian Assessment of Vulnerabilities and Adaptive Capacity; Health Canada: Ottawa, ON, Canada, 2008.
- Boubel, R.W.; Fox, D.L.; Turner, D.B.; Stern, A.C. Fundamentals of Air Pollution, 3rd ed.; Chapter 7 Effects on Health and Human Welfare and Chapter 12 Atmospheric Chemistry; Academic Press: Cambridge, MA, USA, 1994; pp. 99–109,165–177.
- Muilwijk, C.; Schrijvers, P.J.; Wuerz, S.; Kenjereš, S. Simulations of photochemical smog formation in complex urban areas. Atmos. Environ. 2016, 147, 470–484.
- Seinfield, J.H.; Pandis, S.N. Atmospheric Chemistry and Physics, 3rd ed.; Chapter 2.7: Particulate Matter (Aerosols); John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2006; pp. 48–54.
- Krzeszowiak, J.; Stefanow, D.; Pawlas, K. The impact of particulate matter (PM) and nitric oxides (NOx) on human health and an analysis of selected sources accounting for their emission. Med. Sr.—Environ. Med. 2016, 19, 3–15.
- Anyanwu, E. Complex interconvertibility of nitrogen oxides (NOx): Impact on occupational and environmental health. Rev. Environ. Health 1999, 14, 169–185.
- Mohsenin, V. Human exposure to oxides of nitrogen at ambient and supra-ambient concentrations. Toxicology 1994, 89, 301–312.
- Munawer, M.E. Human health and environmental impacts of coal combustion and post-combustion wastes. J. Sustain. Min. 2018, 17, 87–96.
- Skouloudis, A.N.; Kassomenos, P. Combining environment and health information systems for the assessment of atmospheric pollution on human health. Sci. Total Environ. 2014, 488–489, 362–368.
- Vasev, N. Governing energy while neglecting health—The case of Poland. Health Policy 2017, 121, 1147–1153.
- Lu, X.; Yao, T.; Li, Y.; Fung, J.C.; Lau, A.K. Source apportionment and health effect of NOx over the Pearl River Delta region in southern China. Environ. Pollut. 2016, 212, 135–146.
- Zock, J.P.; Verheij, R.; Helbich, M.; Volker, B.; Spreeuwenberg, P.; Strak, M.; Janssen, N.A.H.; Dijst, M.; Groenewegen, P. The impact of social capital, land use, air pollution and noise on individual morbidity in Dutch neighbourhoods. Environ. Int. 2018, 121, 453–460.
- Palmgren, F.; Berkowicz, R.; Hertel, O.; Vignati, E. Effects of reduction of NOx on the NO2 levels in urban streets. Sci. Total Environ. 1996, 189–190, 409–415.
- Patelarou, E.; Tzanakis, N.; Kelly, F.J. Exposure to indoor pollutants and wheeze and asthma development during early childhood. Int. J. Environ. Res. Public Health 2015, 12, 3993–4017.
- Brunekreef, B.; Holgate, S.T. Air pollution and health. Lancet 2002, 360, 1233–1242.
- Mi, Y.H.; Norbäck, D.; Tao, J.; Mi, Y.L.; Ferm, M. Current asthma and respiratory symptoms among pupils in Shanghai, China: Influence of building ventilation, nitrogen dioxide, ozone, and formaldehyde in classrooms. Indoor Air 2006, 16, 454–464.
- Anderson, H.R.; Atkinson, R.W.; Bremmer, S.A.; Carrington, J.; Peacock, P. Quantitative Systematic Review of Short Term Associations between Ambient Air Pollution (Particulate Matter, Ozone, Nitrogen Dioxide, Sulphur Dioxide and Carbon Monoxide), and Mortality and Morbidity; Division of Community Health Sciences St George’s—University of London: London, UK, 2007. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/215975/dh_121202.pdf (accessed on 26 November 2021).
- Kirsch, M.; Korth, H.G.; Sustmann, R.; de Groot, H. The pathobiochemistry of nitrogen dioxide. Biol. Chem. 2002, 383, 389–399.
- McConnell, R.; Berhane, K.; Gilliland, F.; Molitor, J.; Thomas, D.; Lurmann, F.; Avol, E.; Gauderman, W.J.; Peters, J.M. Prospective study of air pollution and bronchitic symptoms in children with asthma. Am. J. Respir. Crit. Care 2003, 168, 790–797.
- Rivas, E.; Santiago, J.L.; Lechón, Y.; Martín, F.; Ariño, A.; Pons, J.J.; Santamaría, J.M. CFD modelling of air quality in Pamplona City (Spain): Assessment, stations spatial representativeness and health impacts valuation. Sci. Total Environ. 2019, 649, 1362–1380.
- Alexeeff, S.E.; Roy, A.; Shan, J.; Liu, X.; Messier, K.; Apte, J.S.; Portier, C.; Sidney, S.; Van Den Eeden, S.K. High-resolution mapping of traffic related air pollution with Google street view cars and incidence of cardiovascular events within neighborhoods in Oakland, CA. Environ. Health-Glob. 2018, 17, 1–13.
- Beelen, R.; Hoek, G.; van den Brandt, P.A.; Goldbohm, R.A.; Fischer, P.; Schouten, L.J. Long-term effects of traffic-related air pollution on mortality in a Dutch cohort (NLCS-AIR study). Environ. Health Perspect. 2008, 116, 196–202.
- Chen, H.; Goldberg, M.S.; Burnett, R.T.; Jerrett, M.; Wheeler, A.J.; Villeneuve, P.J. Long-term exposure to traffic-related air pollution and cardiovascular mortality. Epidemiology 2013, 24, 35–43.
- Gan, W.Q.; Koehoorn, M.; Davies, H.W.; Demers, P.A.; Tamburic, L.; Brauer, M. Long-term exposure to traffic-related air pollution and the risk of coronary heart disease hospitalization and mortality. Environ. Health Perspect. 2011, 119, 501–507.
- Jerrett, M.; Burnett, R.T.; Beckerman, B.S.; Turner, M.C.; Krewski, D.; Thurston, G.; Martin, R.V.; van Donkelaar, A.; Hughes, E.; Shi, Y. Spatial analysis of air pollution and mortality in California. Am. J. Respir. Crit. Care 2013, 188, 593–599.
- Raaschou-Nielsen, O.; Hermansen, M.N.; Loland, L.; Buchvald, F.; Pipper, C.B.; Sørensen, M.; Loft, S.; Bisgaard, H. Long-term exposure to indoor air pollution and wheezing symptoms in infants. Indoor Air 2010, 20, 159–167.
- Rijnders, E.; Janssen, N.A.; van Vliet, P.H.; Brunekreef, B. Personal and outdoor nitrogen dioxide concentrations in relation to degree of urbanization and traffic density. Environ. Health Perspect. 2001, 109, 411–417.
- Weinmayr, G.; Romeo, E.; de Sario, M.; Weiland, S.K.; Forastiere, F. Short-Term effects of PM10 and NO2 on respiratory health among children with asthma or asthma-like symptoms: A systematic review and Meta-Analysis. Environ. Health Perspect. 2010, 118, 449–457.
- Dastoorpoor, M.; Sekhavatpour, Z.; Masoumi, K.; Mohammadi, M.J.; Aghababaeian, H.; Khanjani, N.; Hashemzadeh, B.; Vahedian, M. Air pollution and hospital admissions for cardiovascular diseases in Ahvaz, Iran. Sci. Total Environ. 2019, 652, 1318–1330.
- Janke, K. Air pollution, avoidance behaviour and children’s respiratory health: Evidence from England. J. Health Econ. 2014, 38, 23–42.
- Szyszkowicz, M. Air pollution and emergency department visits for depression in Edmonton, Canada. Int. J. Occup. Med. Environ. 2007, 20, 241–245.
- Gandini, M.; Scarinzi, C.; Bande, S.; Berti, G.; Carnà, P.; Ciancarella, L.; Costa, G.; Demaria, M.; Ghigo, S.; Piersanti, A.; et al. Long term effect of air pollution on incident hospital admissions: Results from the Italian Longitudinal Study within LIFE MED HISS project. Environ. Int. 2018, 121, 1087–1097.
- Mason, T.G.; Schooling, C.M.; Chan, K.P.; Tian, L. An evaluation of the air quality health index program on respiratory diseases in Hong Kong: An interrupted time series analysis. Atmos. Environ. 2019, 211, 151–158.
- Fusco, D.; Forastiere, F.; Michelozzi, P.; Spadea, T.; Ostro, B.; Arcà, M.; Perucci, C.A. Air pollution and hospital admissions for respiratory conditions in Rome, Italy. Eur. Respir. J. 2001, 17, 1143–1150.
- Johansson, C.; Lövenheim, B.; Schantz, P.; Wahlgren, L.; Almström, P.; Markstedt, A.; Strömgren, M.; Forsberg, B.; Sommar, J.N. Impacts on air pollution and health by changing commuting from car to bicycle. Sci. Total Environ. 2017, 584–585, 56–63.
- Al-Ahmadi, K.; Al-Zahrani, A. NO2 and cancer incidence in Saudi Arabia. Int. J. Environ. Res. Public Health 2013, 10, 5844–5862.
- Hystad, P.; Demers, P.A.; Johnson, K.C.; Carpiano, R.M.; Brauer, M. Long-term residential exposure to air pollution and lung cancer risk. Epidemiology 2013, 24, 762–772.
- Nafstad, P.; Håheim, L.L.; Oftedal, B.; Gram, F.; Holme, I.; Hjermann, I.; Leren, P. Lung cancer and air pollution: A 27 year follow up of 16 209 Norwegian men. Thorax 2003, 58, 1071–1076.
- Vineis, P.; Hoek, G.; Krzyzanowski, M.; Vigna-Taglianti, F.; Veglia, F.; Airoldi, L.; Autrup, H.; Dunning, A.; Garte, S.; Hainaut, P.; et al. Air pollution and risk of lung cancer in a prospective study in Europe. Int. J. Cancer 2006, 119, 169–174.
- Yorifuji, T.; Kashima, S.; Tsuda, T.; Ishikawa-Takata, K.; Ohta, T.; Tsuruta, K.I.; Doi, H. Long-term exposure to traffic-related air pollution and the risk of death from hemorrhagic stroke and lung cancer in Shizuoka, Japan. Sci. Total Environ. 2013, 443, 397–402.
- Crouse, D.L.; Goldberg, M.S.; Ross, N.A.; Chen, H.; Labrèche, F. Postmenopausal breast cancer is associated with exposure to traffic-related air pollution in Montreal, Canada: A case-control study. Environ. Health Perspect. 2010, 118, 1578–1583.
- Samoli, E.; Aga, E.; Touloumi, G.; Nisiotis, K.; Forsberg, B.; Lefranc, A.; Pekkanen, J.; Wojtyniak, B.; Schindler, C.; Niciu, E.; et al. Short-term effects of nitrogen dioxide on mortality: An analysis within the APHEA project. Eur. Respir. J. 2006, 27, 1129–1138.
- Atkinson, R.W.; Butland, B.K.; Anderson, H.R.; Maynard, R.L. Long-term concentrations of nitrogen dioxide and mortality: A meta-analysis of cohort studies. Epidemiology 2018, 29, 460–472.
- Ancona, C.; Badaloni, C.; Mataloni, F.; Bolignano, A.; Bucci, S.; Cesaroni, G.; Sozzi, R.; Davoli, M.; Forastiere, F. Mortality and morbidity in a population exposed to multiple sources of air pollution: A retrospective cohort study using air dispersion models. Environ. Res. 2015, 137, 467–474.
- de Marco, A.; Proietti, C.; Anav, A.; Ciancarella, L.; D’Elia, I.; Fares, S.; Fornasier, M.F.; Fusaro, L.; Gualtieri, M.; Manes, F.; et al. Impacts of air pollution on human and ecosystem health, and implications for the National Emission Ceilings Directive: Insights from Italy. Environ. Int. 2019, 125, 320–333.
- Faustini, A.; Rapp, R.; Forastiere, F. Nitrogen dioxide and mortality: Review and meta-analysis of long-term studies. Eur. Respir. J. 2014, 44, 744–753.
- Hoek, G.; Krishnan, R.M.; Beelen, R.; Peters, A.; Ostro, B.; Brunekreef, B.; Kaufman, J.D. Long-term air pollution exposure and cardio-respiratory mortality: A review. Environ. Health-Glob. 2013, 12, 1–15.
- Chen, R.; Samoli, E.; Wong, C.M.; Huang, W.; Wang, Z.; Chen, B.; Kan, H. Associations between short-term exposure to nitrogen dioxide and mortality in 17 Chinese cities: The China Air Pollution and Health Effects Study (CAPES). Environ. Int. 2012, 45, 32–38.
- Shang, Y.; Sun, Z.; Cao, J.; Wang, X.; Zhong, L.; Bi, X.; Li, H.; Liu, W.; Zhu, T.; Huang, W. Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ. Int. 2013, 54, 100–111.
- Tao, Y.; Huang, W.; Huang, X.; Zhong, L.; Lu, S.E.; Li, Y.; Dai, L.; Zhang, Y.; Zhu, T. Estimated acute effects of ambient ozone and nitrogen dioxide on mortality in the Pearl River Delta of southern China. Environ. Health Perspect. 2012, 120, 393–398.
- Malik, A.; Tauler, R. Exploring the interaction between O3 and NOx pollution patterns in the atmosphere of Barcelona, Spain using the MCR-ALS method. Sci. Total Environ. 2015, 517, 151–161.
- World Health Organization. Ambient (Outdoor) Air Pollution. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 21 October 2021).
- Rehm, J.; Shield, K.D. Global Burden of Disease and the Impact of Mental and Addictive Disorders. Curr. Psychiatry Rep. 2019, 21, 10.
- United Nations Department of Economic and Social Affairs. Sustainable Development Goal 3: Ensure Healthy Lives and Promote Well-Being for all at all Ages. 2021. Available online: https://sdgs.un.org/goals/goal3 (accessed on 31 September 2021).
- University of Washington Institute for Health Metrics and Evaluation. Global Burden of Disease Study 2019 (GBD 2019) Data Resources. 2021. Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 30 September 2021).
- Kaufmann, C.N.; Susukida, R.; Depp, C.A. Sleep apnea, psychopathology, and mental health care. Sleep Health 2017, 3, 244–249.
- Kanner, J.; Pollack, A.Z.; Ranasinghe, S.; Stevens, D.R.; Nobles, C.; Rohn, M.C.; Sherman, S.; Mendola, P. Chronic exposure to air pollution and risk of mental health disorders complicating pregnancy. Environ. Res. 2021, 196, 110937.
- Bakolis, I.; Hammoud, R.; Stewart, R.; Beevers, S.; Dajnak, D.; MacCrimmon, S.; Broadbent, M.; Pritchard, M.; Shiode, N.; Fecht, D.; et al. Mental health consequences of urban air pollution: Prospective population-based longitudinal survey. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 1587–1599.
- Klompmaker, J.O.; Hoek, G.; Bloemsma, L.D.; Wijga, A.H.; van den Brink, C.; Brunekreef, B.; Lebret, E.; Gehring, U.; Janssen, N.A.H. Associations of combined exposures to surrounding green, air pollution and traffic noise on mental health. Environ. Int. 2019, 129, 525–537.
- Pelgrims, I.; Devleesschauwer, B.; Guyot, M.; Keune, H.; Nawrot, T.S.; Remmen, R.; Saenen, N.D.; Trabelsi, S.; Thomas, I.; Aerts, R.; et al. Association between urban environment and mental health in Brussels, Belgium. BMC Public Health 2021, 21, 635.
- Gu, H.; Yan, W.; Elahi, E.; Cao, Y. Air pollution risks human mental health: An implication of two-stages least squares estimation of interaction effects. Environ. Sci. Pollut. R 2020, 27, 2036–2043.
- Newbury, J.B.; Stewart, R.; Fisher, H.L.; Beevers, S.; Dajnak, D.; Broadbent, M.; Pritchard, M.; Shiode, N.; Heslin, M.; Hammoud, R.; et al. Association between air pollution exposure and mental health service use among individuals with first presentations of psychotic and mood disorders: Retrospective cohort study. Br. J. Psychiatry 2021, 219, 678–685.
- Chan, E.Y.; Lam, H.C.; So, S.H.; Goggins, W.B.; Ho, J.Y.; Liu, S.; Chung, P.P. Association between ambient temperatures and mental disorder hospitalizations in a subtropical city: A time-series study of Hong Kong special administrative region. Int. J. Environ. Res. Public Health 2018, 15, 754.
- Chen, C.; Liu, C.; Chen, R.; Wang, W.; Li, W.; Kan, H.; Fu, C. Ambient air pollution and daily hospital admissions for mental disorders in Shanghai, China. Sci. Total Environ. 2018, 613–614, 324–330.
- Oudin, A.; Åström, D.O.; Asplund, P.; Steingrimsson, S.; Szabo, Z.; Carlsen, H.K. The association between daily concentrations of air pollution and visits to a psychiatric emergency unit: A case-crossover study. Environ. Health-Glob. 2018, 17, 4.
- Wei, F.; Wu, M.; Qian, S.; Li, D.; Jin, M.; Wang, J.; Shui, L.; Lin, H.; Tang, M.; Chen, K. Association between short-term exposure to ambient air pollution and hospital visits for depression in China. Sci. Total Environ. 2020, 724, 138207.
- Lu, P.; Zhang, Y.; Xia, G.; Zhang, W.; Xu, R.; Wang, C.; Guo, Y.; Li, S. Attributable risks associated with hospital outpatient visits for mental disorders due to air pollution: A multi-city study in China. Environ. Int. 2020, 143, 105906.
- Thilakaratne, R.A.; Malig, B.J.; Basu, R. Examining the relationship between ambient carbon monoxide, nitrogen dioxide, and mental health-related emergency department visits in California, USA. Sci. Total Environ. 2020, 746, 140915.
- Li, H.; Zhang, S.; Qian, Z.; Xie, X.H.; Luo, Y.; Han, R.; Hou, J.; Wang, C.; McMillin, S.E.; Wu, S.; et al. Short-term effects of air pollution on cause-specific mental disorders in three subtropical Chinese cities. Environ. Res. 2020, 191, 110214.
- Tong, L.; Li, K.; Zhou, Q. Season, sex and age as modifiers in the association of psychosis morbidity with air pollutants: A rising problem in a Chinese metropolis. Sci. Total Environ. 2016, 541, 928–933.
- Billings, M.E.; Gold, D.; Szpiro, A.; Aaron, C.P.; Jorgensen, N.; Gassett, A.; Leary, P.L.; Kaufman, J.D.; Redline, S.R. The association of ambient air pollution with sleep apnea: The multi-ethnic study of atherosclerosis. Ann. Am. Thorac. Soc. 2019, 16, 363–370.
- Lawrence, W.R.; Yang, M.; Zhang, C.; Liu, R.Q.; Lin, S.; Wang, S.Q.; Liu, Y.; Ma, H.; Chen, D.H.; Zeng, X.W.; et al. Association between long-term exposure to air pollution and sleep disorder in Chinese children: The Seven Northeastern Cities study. Sleep 2018, 41, 1–10.
- Vert, C.; Sánchez-Benavides, G.; Martínez, D.; Gotsens, X.; Gramunt, N.; Cirach, M.; Molinuevo, J.L.; Sunyer, J.; Nieuwenhuijsen, M.J.; Crous-Bou, M.; et al. Effect of long-term exposure to air pollution on anxiety and depression in adults: A cross-sectional study. Int. J. Hyg. Environ. Health 2017, 220, 1074–1080.
- Shin, J.; Park, J.Y.; Choi, J. Long-term exposure to ambient air pollutants and mental health status: A nationwide population-based cross-sectional study. PLoS ONE 2018, 13, e0195607.
- Lim, Y.H.; Kim, H.; Kim, J.H.; Bae, S.; Park, H.Y.; Hong, Y.C. Air Pollution and Symptoms of Depression in Elderly Adults. Environ. Health Perspect. 2012, 120, 1023–1028.
- Wang, Y.; Eliot, M.N.; Koutrakis, P.; Gryparis, A.; Schwartz, J.D.; Coull, B.A.; Mittleman, M.A.; Milberg, W.P.; Lipsitz, L.A.; Wellenius, G.A. Ambient air pollution and depressive symptoms in older adults: Results from the MOBILIZE Boston study. Environ. Health Perspect. 2014, 122, 553–558.
- Zijlema, W.L.; Wolf, K.; Emeny, R.; Ladwig, K.H.; Peters, A.; Kongsgård, H.; Hveem, K.; Kvaløy, K.; Yli-Tuomi, T.; Partonen, T.; et al. The association of air pollution and depressed mood in 70,928 individuals from four European cohorts. Int. J. Hyg. Environ. Health 2016, 219, 212–219.
- Altuğ, H.; Fuks, K.B.; Hüls, A.; Mayer, A.K.; Tham, R.; Krutmann, J.; Schikowski, T. Air pollution is associated with depressive symptoms in elderly women with cognitive impairment. Environ. Int. 2020, 136, 105448.
- Kim, S.Y.; Bang, M.; Wee, J.H.; Min, C.; Yoo, D.M.; Han, S.M.; Kim, S.; Choi, H.G. Short- and long-term exposure to air pollution and lack of sunlight are associated with an increased risk of depression: A nested case-control study using meteorological data and national sample cohort data. Sci. Total Environ. 2021, 757, 143960.
- Lo, K.; Chiang, L.L.; Hsu, S.M.; Tsai, C.Y.; Wu, D.; Chou, C.J.; Chuang, H.C.; Liu, W.T. Association of short-term exposure to air pollution with depression in patients with sleep-related breathing disorders. Sci. Total Environ. 2021, 786, 147291.
- Latham, R.M.; Kieling, C.; Arseneault, L.; Botter-Maio Rocha, T.; Beddows, A.; Beevers, S.; Danese, A.; De Oliveira, K.; Kohrt, B.A.; Moffitt, T.E.; et al. Childhood exposure to ambient air pollution and predicting individual risk of depression onset in UK adolescents. J. Psychiatry Res. 2021, 138, 60–67.
- Szyszkowicz, M.; Rowe, B.; Colman, I. Air pollution and daily emergency department visits for depression. Int. J. Occup. Med. Environ. 2009, 22, 355–362.
- Szyszkowicz, M.; Kousha, T.; Kingsbury, M.; Colman, I. Air Pollution and Emergency Department Visits for Depression: A Multicity Case-Crossover Study. Environ. Health Insights 2016, 10, 155–161.
- Cho, J.; Choi, Y.J.; Suh, M.; Sohn, J.; Kim, H.; Cho, S.K.; Ha, K.H.; Kim, C.; Shin, D.C. Air pollution as a risk factor for depressive episode in patients with cardiovascular disease, diabetes mellitus, or asthma. J. Affect. Disord. 2014, 157, 45–51.
- Zhou, Y.M.; An, S.J.; Tang, E.J.; Xu, C.; Cao, Y.; Liu, X.L.; Yao, C.Y.; Xiao, H.; Zhang, Q.; Liu, F.; et al. Association between short-term ambient air pollution exposure and depression outpatient visits in cold seasons: A time-series analysis in northwestern China. J. Toxicol. Environ. Health A 2021, 84, 389–398.
- Gu, X.; Guo, T.; Si, Y.; Wang, J.; Zhang, W.; Deng, F.; Chen, L.; Wei, C.; Lin, S.; Guo, X.; et al. Association between ambient air pollution and daily hospital admissions for depression in 75 Chinese cities. Am. J. Psychiatry 2020, 177, 735–743.
- Szyszkowicz, M.; Willey, J.B.; Grafstein, E.; Rowe, B.H.; Colman, I. Air Pollution and Emergency Department Visits for Suicide Attempts in Vancouver, Canada. Environ. Health Insights 2010, 4, 79–86.
- Min, J.; Kim, H.J.; Min, K. Long-term exposure to air pollution and the risk of suicide death: A population-based cohort study. Sci. Total Environ. 2018, 628–629, 573–579.
- Ng, C.F.; Stickley, A.; Konishi, S.; Watanabe, C. Ambient air pollution and suicide in Tokyo, 2001–2011. J. Affect. Disord. 2016, 201, 194–202.
- Kim, Y.; Ng, C.F.; Chung, Y.; Kim, H.; Honda, Y.; Guo, Y.L.; Lim, Y.H.; Chen, B.Y.; Page, L.A.; Hashizume, M. Air pollution and suicide in 10 cities in Northeast Asia: A time-stratified case-crossover analysis. Environ. Health Perspect. 2018, 126, 037002.
- Bakian, A.; Huber, R.S.; Coon, H.; Gray, D.; Wilson, P.; McMahon, W.M.; Renshaw, P.F. Acute air pollution exposure and risk of suicide completion. Am. J. Epidemiol. 2015, 181, 295–303.
- IQAir. 2020 World Air Quality Report: Region & City PM2.5 Ranking. Available online: https://www.iqair.com/ca/world-most-polluted-countries (accessed on 10 December 2021).
More
