In the last few years, technological developments in the surgical field have been rapid and are continuously evolving. One of the most revolutionizing breakthroughs was the introduction of the IoT concept within the surgical practice. This systematic review of the literature aims to summarize the most important studies evaluating the IoT concept within the surgical practice, focusing on Telesurgery and Surgical Telementoring. In addition, we provide systematic overviews of the IoST use in image-guided surgery, as well as Telemonitoring of the surgical patient.
- surgical practice
- Internet of Surgical Things
- Internet of Things
- Surgery
- Telemonitoring
- Telesurgery
- Telemedicine
Introduction
Advances in surgical practice have been rapid and non-stop for the past few centuries. From the groundbreaking idea by Joseph Lister that postoperative deaths might be attributed to certain invisible pathogens that could be combated with antiseptic solutions, to the popularization of robotic surgery in many modern medical centers, progress has been continuous. Many related advances came in the form of technological milestones that changed the shape of surgical practice as we know it today. The latest in a series of breakthroughs in the smart health domain is the utilization of the Internet in everyday surgical practice, the role of which is ever-expanding.
To systematically study the technological advances in a particular sector, attributed to the utilization of the Internet, the term “Internet of Things” (IoT) was introduced. While
not strictly defined, IoT describes a network of Internet-based connected things equipped with (embedded) sensing and actuating devices, with data production, processing, and
consumption abilities. The utilization of the Internet and IoT in medical practice can take many shapes and forms. Ranging from the awe-inspiring telesurgical procedures to
complex AI machine learning applications that aid in medical decision making, to a simple email containing a preoperative CT scan, the Internet of Surgical Things (IoST) is
here to stay. A representative example of the IoST is a smart ingestible sensor (pill) that is activated after being swallowed, “travels” in the body through the colon and sends
data to outer devices such as computers and smartphones when it detects a threat for cancer. Such a device can be used instead of colonoscopy for people who cannot obtain a
colonoscopy due to psychological and physiological problems. In the broader aspect of the IoST context, IoST entities are different types of connected entities that “live” in this
smart setting, such as surgical things (e.g., a connected surgery tool), organs (e.g., a connected colon, an artificial heart), humans (e.g., a connected patient or doctor),
smart devices (e.g., a connected heartbeat monitoring device, a smart pill, an ingestible sensor), services (e.g., a connected telemonitoring service), data (e.g., a connected data steam of heart monitoring data), etc. In this extensive survey, we aim to present an overview of current uses of IoT-embedded surgical practice by focusing on Telesurgery and Surgical Telementoring. As a secondary research question, we also briefly review the latest advances in IoT-associated image guided surgery, and surgical patient telemonitoring by utilizing the IoT paradigm.
Current literature on the Internet of Medical Things (IoMT) includes a multitude of heterogenous reports of Internet-based applications within the medical/healthcare domain.
Most of the related articles present network(s) of sensor arrays and data processing stations, with or without actuating devices, interconnected via the Internet infrastructure. There
is, however, a lack of a systematic approach within the existing literature as to how the IoT concept has revolutionized the surgical world towards smarter health. To fill this
gap in current knowledge, the present systematic literature review studies the Internet of Surgical Things (IoST) domain by focusing on the three most prominent areas of application: (a) image-guided surgery, (b) telesurgery and telementoring in surgery, and (c) surgical patient monitoring [3,5]. Between these three areas of applications within the surgical discipline, the applications of Telesurgery and Surgical Telementoring are undoubtedly the most influenced by the IoMT concept. Therefore, our systematic review will be centered around studies of these applications. Additionally, we will briefly discuss the current literature on patient monitoring and IoT applications in image-guidance.
In this review, we systematically discuss a novel concept (the IoST) that is being rapidly incorporated into surgical practice. This is one of the first systematic review manuscripts
covering this area. By focusing on the three applications described above, we provide a thorough understanding of the feasibility and effectiveness of different IoST applications. In
addition, this paper also summarizes known and emerging weak points in IoST ecosystems that should be the focus of future research efforts. Finally, by incorporating data from
system development studies, we offer insight into promising future uses of the IoST that are yet to be popularized but have the potential to be groundbreaking advances.
While there is a lack of a universally accepted definition for the Internet of Things, for the purposes of this review, we considered studies looking into ecosystems of interconnected computing devices, digital screens, sensor-bearing instruments, robotic surgery systems, mobile phones, 5th generation mobile networks, and can even include people (in
our case either operators or patients. We have focused our attention on systems operating within the surgical world, connecting two or more “Things” (as defined above), via a
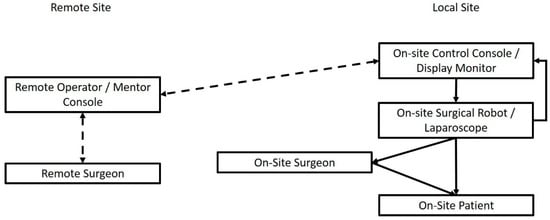
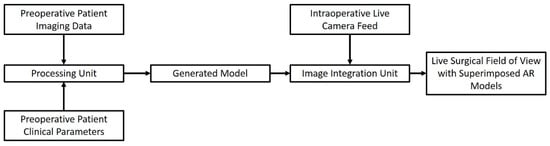
certain, defined, and dedicated network. Looking into our specified research questions, some examples of IoT applications would be, for instance, a network comprising a preoperative imaging modality (e.g., MRI scanner), a processing station, and software within a specialized robot or specialized augmented reality glasses that ultimately aim to facilitate a procedure by superimposing real-time image guidance. Telementoring/Telesurgery systems usually comprise specialized working stations connected to a user that are capable of transmitting audiovisual cues and/or controlling a surgical robot at a distant location. Finally, telemonitoring is carried out by an interconnected series of sensor-bearing devices that centripetally transmit patient data, either directly to the physician, or to a dedicated data-gathering station.
1. The Internet of Telesurgery and Surgical Telementoring
2. Image-Guided Surgery in the IoT Era
3. The Role of the IoT in Telemonitoring the Surgical Patient
Table S3). Medical telemonitoring usually consists of a specialized “smart” device that captures target parameters and transmits them through a wireless Internet connection,
either directly to the referring physician, or to a centralized repository from which they can be accessed (Figure 3). The role of the Internet here is more straightforward: instead of being the network substrate that interconnects a variety of operating stations, data repositories and data processing modalities, here, it is used as a unidirectional “data highway” that
runs towards the physician. In contrast to previous advances, telemonitoring has been widely implemented in some healthcare systems.
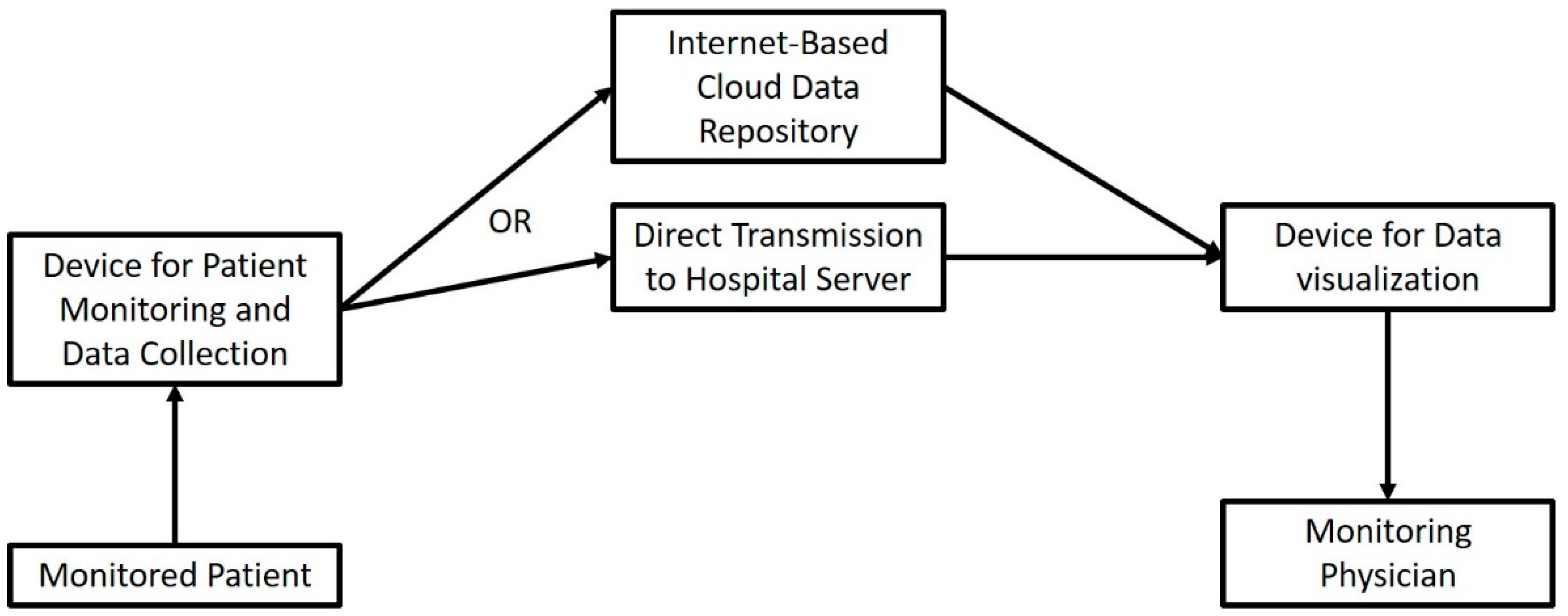
(Supplemental Table S3). Patients enrolled in an at-home monitoring program after chest wall surgery were also monitored effectively by utilizing the Internet to input certain
parameters in an online platform [65,67] Cardiac surgery patients were also studied in an IoST rehabilitation program that included wearable biomedical and motion tracking
sensors [68]. The physician was therefore able to monitor the patients’ activity levels and their performance in rehabilitation exercises. In a 2021 study by Cos et al., patients
scheduled to undergo pancreatic surgery were monitored preoperatively by using a wearable smart device that was able to record heart rate, activity status, etc., and through
an internet connection, transmit them to a central server. Not only did patients adhere to this novel concept, but the data that were automatically collected were of such quality
that the research team developed an accurate predictive model for postoperative outcomes. Biosensor-based systems are able to wirelessly transmit data on physiological
parameters of the patients in order to assist with postoperative monitoring. Authors have reported the incorporation of pulse rate, blood pressure and activity tracking sensors as
being successful in monitoring the rehabilitation process of surgical patients [69–77]. Reported advantages, include successful vital signs readings, short training period of
nurses and patients alike, less unplanned office visits, and predicting unplanned postoperative complications by indirect monitoring of vital signs [8]. Kim et al. successfully
developed a Doppler cuff that could be remotely monitored, allowing remote monitoring of the blood flow of skin flaps. This resulted in superior graft survivability rates [6]. Results such as these are indicative that we have come to a point at which smart devices with Internet connections can provide fast and accurate measurements of clinical parameters in a reproducible manner and have the potential to effectively substitute an in-office visit for routine monitoring. In addition to the universally observed accuracy of
the requested parameter measurements, distance monitoring saves time for the patient and the physician alike, prevents missed appointments and is generally preferred by patients [78–80]. When studying the response of bariatric patients postoperatively, regarding the telemonitoring process, Vilallonga et al. found that patients themselves would
prefer the telemonitoring option [71].
pain. Postoperative pain and nausea were reduced in the patients treated with this system. An ostomy alert sensor was developed by the team of Rouholiman et al. [80] that was
capable of alerting nurses, patients, and physicians alike of the content status of the ostomy.
no studies for this specific cohort of patients. Systems used to monitor diseases such as heart failure, hypertension, pregnancy-related complications and more can easily be
applied to the surgical patient in the future. A recently developed smartphone application could aid in the distant monitoring of COPD patients and could be useful in the detection
of acute exacerbations and advise timely hospitalization [74]. All the above-mentioned modalities for long distance patient monitoring rely on the Internet for data transmission
and could very well see their way in surgical patient monitoring or consultation in the not-so-distant future.
with operating such systems [74–78]. Technological illiteracy is a persistent issue that seems harder to address than the technicalities of the systems. Patients of older age, of mental
burden and patients without a reliable Internet connection that is readily accessible are in danger of being left out of such technological advancements, an observation reported in the
majority of clinical studies. What is more, home-based distance monitoring relies entirely upon the adherence of the patient in data recording and the use of the instructed devices
4. Discussing Open Issues and Challenges
Telesurgery and surgical telementoring are undoubtedly the most impressive of the listed IoT applications within the surgical practice. Looking into the included particles
of the presented survey, we can safely say that long-distance surgery on real-life patients is now feasible, although it seems to be scarcely performed. Authors do not mention
any surgical safety compromises when IoT networks were utilized to perform telesurgery, which is most definitely the first hurdle that a newly emerging technique must overcome
on its way to popularization. However, the most significant drawback of these applications, is the requirement of fast, stable Internet connections that will allow minimal latency and
data loss. Paradoxically, such Internet connections may be lacking in the areas that are most in need of telesurgical and telementoring applications, such as rural and distant
institutions that are not able to provide expert surgical consultations. Popularization of 5th generation (5G) mobile Internet networks is expected to be a big step towards that
direction that will guarantee minimal latency and maximal connection stability. Particularly for telesurgical applications, there is also the issue of legal implications, as is underlined
by several authors. The lack of specific legislature regarding long-distance surgery might prove to be grounds for liability of the providers, which is not previously described or
covered by insurance. Due to the rapid implementation of such systems that is expected to follow, we must tackle such issues rapidly so that providers feel confident in partaking in
long-distance operations or consultations. Financial costs are once again a key factor in play here. Teleconsultation or telementoring might not require much more than an audiovisual connection over the Internet; however, telesurgery itself requires surgical robots in order to transfer the instrument movements as instructed by the surgeon. Once again, these are not available everywhere on the globe, and rural centers in need of distant expert consultation are not likely to have robotic surgical systems available. From the above, it can be concluded that the feasibility and reliability of a new paradigm such as the IoST in telesurgery are not guarantees for its widespread application. There are still major logistic problems to overcome before telesurgery becomes part of the everyday surgical practice. Our research team aims to set up the first surgical telementoring system in Greece that will begin by providing a real-time audiovisual connection between an expert and a novice surgeon with live intraoperative guidance. This system will be evaluated against the traditional live mentoring of more inexperienced surgeons in order to provide a proof-of-concept. Further steps within our goals also include the introduction of more surgical centers to the said system in view of establishing a network of interconnected hospitals that provide regularsurgical consultation over the Internet.
pain. By making use of serial interconnected data processing modules, researchers are able to construct IoT networks that greatly facilitate image-guidance in surgery. The
real-time integration of preoperative imaging is the main goal in this case. The tracking of the imaging-specified patient anatomy in real-time surgical operations has proved
highly significant in increasing surgical accuracy, and, in many cases, in assisting the prevention of accidental tissue damage. Despite encouraging results from proof-of-concept
studies, however, these systems seem to be lacking adequate investigation in large-scale patient cohorts. As such, it is not safe to state with confidence that image-guided surgery
incorporating the IoT paradigm today is widely accepted for clinical use. Still, we can safely conclude that IoT-based tool-tracking sensors will be proved valuable in the near future,
especially for the surgeons that require maximum precision in instrument or anatomical landmark tracking. A major advantage of these systems, as already mentioned by a large
number of authors, is the capability of IoST to account for interpersonal variability in anatomical structures in a real-time manner. Despite the lack of explicit reference in any
of the included studies, acquisition of the necessary tool-tracking sensors and software is surely expected to be a major issue for several institutions. Therefore, the scientific
community ought to aim for larger studies on surgical patients that will not only include image-guidance systems similar to those mentioned here but will randomize patients
between image-guidance systems in order to better delineate the proposed advantages over older systems.
Long-distance monitoring using IoT is also one of the most common applications in medicine and healthcare. There is a limited number of articles including telemonitoring
of the surgical patient specifically; however, such systems have proven their value in patient comfort and effective physiological parameter monitoring. The major challenge
in the widespread implementation of said systems is the technological literacy of the patient population, as well as its Internet access. While improving Internet access is an
ongoing global strife, researchers must focus on constructing adaptable and more intuitive user interfaces of such applications in order to appeal to older patients not comfortable
with the everyday use of technological applications, wearable sensors and smart devices.
adoption of IoT-based monitoring of the surgical patient.
5. Conclusions
The aim of the present literature review is to collect and analyze the available knowledge on the most prominent fields that the IoT paradigm finds application to the surgical
practice, i.e., the Internet of Surgical Things. Technological advances allow the incorporation of rendered preoperative data to the live surgical field, the valuable from-a-distance
mentorship of younger from more experienced surgeons, the realization of a surgical procedure by remotely controlled robots, and the monitoring of surgical patients without
the need for hospital visits. Despite the availability of reliable and fast Internet being arequirement for the actualization of these concepts in more areas of the world, the seamless
incorporation of “smart” functions within the surgical world with the aid of the Internet is on a steady route to becoming a reality towards smarter and more efficient health services.
This study faces certain methodological limitations which arise from the narrative structure of most of the included literature. To begin with, this is a narrative systematic review, meaning that there are no statistical deductions to be made or pre-specified comparisons between different methodological approaches. The IoST is a concept, rather than a method, and therefore tangible comparisons can only be made in very specific applications.
Current literature on IoST is lacking in comparative studies that produce results one can use to reach safe conclusions. Despite adhering to specific selection criteria, our study selection process was amenable to an unavoidable degree of bias, arising mainly from the lack of specific clinical applications in many of the screened publications. Finally, our inclusion of feasibility and animal model studies needs to be interpreted as a showcase of potential future applications, rather than everyday uses of the IoST concept. The review’s findings can be summarized, per the research question, in the following paragraphs.
Telesurgical applications are undoubtedly the primary example of IoST systems. Their validity has been repeatedly evaluated over the years and the literature reveals that telesurgical networks are routinely incorporated in many surgical centers. Within such systems, there is a wide adoption of sensorial arrays that transmit data to distant locations. Telementoring is an even more inclusive concept in surgical education. Evaluation of distant teaching in surgery has revealed that it is a viable alternative to traditional teaching, which is at times preferred over in-person assistance. Recent literature also points out the incorporation of 5th generation cellular networks that are able to effectively eradicate latency times and connectivity issues.
IoST in image-guided surgery is currently an “under development” application that has produced tangible results in only a few clinical studies. Intraoperative use of IoST
networks mainly focuses on superimposing preoperative imaging on live surgical camera feeds to assist surgeons in precision-requiring tasks. Despite being investigated mainly in
neurosurgical procedures, these networks are predominantly software-dependent, thus making it possible to also be incorporated in more procedures in the years to come.
Patient telemonitoring involves the utilization of network-connected biosensors that track physiological patient parameters that are observed by a distant physician. Such
sensorial ecosystems seem to be highly successful at detecting specified cutoff points and providing alerts to the physicians. Additionally, such systems can shorten hospital stays
and lessen routine in-office patient visits, without compromising patient safety. Lastly, telemonitoring has relatively few requirements, considering the availability of biosensors
in everyday technological products and “smart” wearable devices.
References
- Agrawal, R.; Mishra, S.K.; Mishra, A.; Chand, G.; Agarwal, G.; Agarwal, A.; Verma, A.K. Role of Telemedicine Technology in Endocrine Surgery Knowledge Sharing. Telemed. J. E-Health 2014, 20, 868–874.
- Andersen, D.; Popescu, V.; Cabrera, M.E.; Shanghavi, A.; Mullis, B.; Marley, S.; Gomez, G.; Wachs, J.P. An Augmented Reality-Based Approach for Surgical Telementoring in Austere Environments. Mil. Med. 2017, 182, 310–315.
- Anderson, S.M.; Kapp, B.B.; Angell, J.M.; Abd, T.T.; Thompson, N.J.; Ritenour, C.W.M.; Issa, M.M. Remote Monitoring and Supervision of Urology Residents Utilizing Integrated Endourology Suites—A Prospective Study of Patients’ Opinions. J. Endourol. 2013, 27, 96–100.
- Andersen, D.; Popescu, V.; Cabrera, M.E.; Shanghavi, A.; Gomez, G.; Marley, S.; Mullis, B.; Wachs, J.P. Medical Telementoring Using an Augmented Reality Transparent Display. Surgery 2016, 159, 1646–1653.
- Artsen, A.M.; Burkett, L.S.; Duvvuri, U.; Bonidie, M. Surgeon Satisfaction and Outcomes of Tele-Proctoring for Robotic Gynecologic Surgery. J. Robot. Surg. 2022, 16, 563–568.
- Prince, S.W.; Kang, C.; Simonelli, J.; Lee, Y.H.; Gerber, M.J.; Lim, C.; Chu, K.; Dutson, E.P.; Tsao, T.C. A Robotic System for Telementoring and Training in Laparoscopic Surgery. Int. J. Med. Robot. 2020, 16, e2040.
- Patel, E.; Mascarenhas, A.; Subuhee, A.; Stirt, D.; Brady, I.; Perera, R.; Noël, J. Evaluating the Ability of Students to Learn and Utilize a Novel Telepresence Platform, Proximie. J. Robot. Surg. 2021, 2021, 1–7.
- Rojas-Muñoz, E.; Cabrera, M.E.; Lin, C.; Andersen, D.; Popescu, V.; Anderson, K.; Zarzaur, B.L.; Mullis, B.; Wachs, J.P. The System for Telementoring with Augmented Reality (STAR): A Head-Mounted Display to Improve Surgical Coaching and Confidence in Remote Areas. Surgery 2020, 167, 724–731.
- Rojas-Muñoz, E.; Cabrera, M.E.; Andersen, D.; Popescu, V.; Marley, S.; Mullis, B.; Zarzaur, B.; Wachs, J. Surgical Telementoring without Encumbrance: A Comparative Study of See-through Augmented Reality-Based Approaches. Ann. Surg. 2019, 270, 384–389.
- Rojas-Munõz, E.; Cabrera, M.E.; Lin, C.; Sánchez-Tamayo, N.; Andersen, D.; Popescu, V.; Anderson, K.; Zarzaur, B.; Mullis, B.; Wachs, J.P. Telementoring in Leg Fasciotomies via Mixed-Reality: Clinical Evaluation of the STAR Platform. Mil. Med. 2020, 185, 513–520.
- Rojas-Muñoz, E.; Lin, C.; Sanchez-Tamayo, N.; Cabrera, M.E.; Andersen, D.; Popescu, V.; Barragan, J.A.; Zarzaur, B.; Murphy, P.; Anderson, K.; et al. Evaluation of an Augmented Reality Platform for Austere Surgical Telementoring: A Randomized Controlled Crossover Study in Cricothyroidotomies. NPJ Digit. Med. 2020, 3, 75.
- Safir, I.J.; Shrewsberry, A.B.; Issa, I.M.; Ogan, K.; Ritenour, C.W.M.; Sullivan, J.; Issa, M.M. Impact of Remote Monitoring and Supervision on Resident Training Using New ACGME Milestone Criteria. Can. J. Urol. 2015, 22, 7959–7964.
- Schlachta, C.M.; Lefebvre, K.L.; Sorsdahl, A.K.; Jayaraman, S. Mentoring and Telementoring Leads to Effective Incorporation of Laparoscopic Colon Surgery. Surg. Endosc. 2010, 24, 841–844.
- Talbot, M.; Harvey, E.J.; Berry, G.K.; Reindl, R.; Tien, H.; Stinner, D.J.; Slobogean, G. A Pilot Study of Surgical Telementoring for Leg Fasciotomy. BMJ Mil. Health 2018, 164, 83–86.
- Trujillo Loli, Y.; D’Carlo Trejo Huamán, M.; Campos Medina, S. Telementoring of In-Home Real-Time Laparoscopy Using Whatsapp Messenger: An Innovative Teaching Tool during the COVID-19 Pandemic. A Cohort Study. Ann. Med. Surg. 2021, 62, 481–484.
- Andersen, D.S.; Cabrera, M.E.; Rojas-Muñoz, E.J.; Popescu, V.S.; Gonzalez, G.T.; Mullis, B.; Marley, S.; Zarzaur, B.L.; Wachs, J.P. Augmented Reality Future Step Visualization for Robust Surgical Telementoring. Simul. Healthc. 2019, 14, 59–66.
- Dawe, P.; Kirkpatrick, A.; Talbot, M.; Beckett, A.; Garraway, N.; Wong, H.; Hameed, S.M. Telementored Damage-Control and Emergency Trauma Surgery: A Feasibility Study Using Live-Tissue Models. Am. J. Surg. 2018, 215, 927–929.
- DeKastle, R. Telesurgery: Providing Remote Surgical Observations for Students. AORN J. 2009, 90, 93–101.
- Din, N.; Chan, C.C.; Cohen, E.; Iovieno, A.; Dahan, A.; Rootman, D.S.; Litvin, G. Remote Surgeon Virtual Presence: A Novel Telementoring Method for Live Surgical Training. Cornea 2022, 41, 385–389.
- Hinata, N.; Miyake, H.; Kurahashi, T.; Ando, M.; Furukawa, J.; Ishimura, T.; Tanaka, K.; Fujisawa, M. Novel Telementoring System for Robot-Assisted Radical Prostatectomy: Impact on the Learning Curve. Urology 2014, 83, 1088–1092.
- Altieri, M.S.; Carmichael, H.; Jones, E.; Robinson, T.; Pryor, A.; Madani, A. Educational Value of Telementoring for a Simulation-Based Fundamental Use of Surgical EnergyTM (FUSE) Curriculum: A Randomized Controlled Trial in Surgical Trainees. Surg. Endosc. 2020, 34, 3650–3655.
- Glenn, I.C.; Bruns, N.E.; Hayek, D.; Hughes, T.; Ponsky, T.A. Rural Surgeons Would Embrace Surgical Telementoring for Help with Difficult Cases and Acquisition of New Skills. Surg. Endosc. 2017, 31, 1264–1268.
- Lenihan, J.; Brower, M. Web-Connected Surgery: Using the Internet for Teaching and Proctoring of Live Robotic Surgeries. J. Robot. Surg. 2012, 6, 47–52.
- Moore, A.M.; Carter, N.H.; Wagner, J.P.; Filipi, C.J.; Chen, D.C. Web-Based Video Assessments of Operative Performance for Remote Telementoring. Surg. Technol. Int. 2017, 25, 25–30.
- Tel, A.; Bortuzzo, F.; Pascolo, P.; Costa, F.; Sembronio, S.; Bresadola, V.; Baldi, D.; Robiony, M. Maxillofacial Surgery 5.0: A New Paradigm in Telemedicine for Distance Surgery, Remote Assistance, and Webinars. Minerva Stomatol. 2020, 69, 191–202.
- Shin, D.H.; Dalag, L.; Azhar, R.A.; Santomauro, M.; Satkunasivam, R.; Metcalfe, C.; Dunn, M.; Berger, A.; Djaladat, H.; Nguyen, M.; et al. A Novel Interface for the Telementoring of Robotic Surgery. BJU Int. 2015, 116, 302–308.
- Kirkpatrick, A.W.; McKee, J.L.; Netzer, I.; McBeth, P.B.; D’Amours, S.; Kock, V.; Dobron, A.; Ball, C.G.; Glassberg, E. Transoceanic Telementoring of Tube Thoracostomy Insertion: A Randomized Controlled Trial of Telementored Versus Unmentored Insertion of Tube Thoracostomy by Military Medical Technicians. Telemed. E-Health 2019, 25, 730–739.
- Liu, P.; Li, C.; Xiao, C.; Zhang, Z.; Ma, J.; Gao, J.; Shao, P.; Valerio, I.; Pawlik, T.M.; Ding, C.; et al. A Wearable Augmented Reality Navigation System for Surgical Telementoring Based on Microsoft HoloLens. Ann. Biomed. Eng. 2021, 49, 287–298.
- Lacy, A.M.; Bravo, R.; Otero-Piñeiro, A.M.; Pena, R.; De Lacy, F.B.; Menchaca, R.; Balibrea, J.M. 5G-Assisted Telementored Surgery. Br. J. Surg. 2019, 106, 1576–1579.
- Netzer, I.; Kirkpatrick, A.W.; Nissan, M.; McKee, J.L.; McBeth, P.; Dobron, A.; Glassberg, E. Rubrum Coelis: The Contribution of Real-Time Telementoring in Acute Trauma Scenarios-A Randomized Controlled Trial. Telemed. E-Health 2019, 25, 1108–1114.
- Greenberg, J.A.; Schwarz, E.; Paige, J.; Dort, J.; Bachman, S. At-Home Hands-on Surgical Training during COVID19: Proof of Concept Using a Virtual Telementoring Platform. Surg. Endosc. 2021, 35, 1963–1969.
- Forgione, A.; Kislov, V.; Guraya, S.Y.; Kasakevich, E.; Pugliese, R. Safe Introduction of Laparoscopic Colorectal Surgery Even in Remote Areas of the World: The Value of a Comprehensive Telementoring Training Program. J. Laparoendosc. Adv. Surg. Tech. 2015, 25, 37–42.
- Chu, G.; Yang, X.; Luo, L.; Feng, W.; Jiao, W.; Zhang, X.; Wang, Y.; Yang, Z.; Wang, B.; Li, J.; et al. Improved Robot-Assisted Laparoscopic Telesurgery: Feasibility of Network Converged Communication. Br. J. Surg. 2021, 108, e377–e379.
- Wirz, R.; Torres, L.G.; Swaney, P.J.; Gilbert, H.; Alterovitz, R.; Webster, R.J.; Weaver, K.D.; Russell, P.T. An Experimental Feasibility Study on Robotic Endonasal Telesurgery. Neurosurgery 2015, 76, 479–484.
- Zheng, J.; Wang, Y.; Zhang, J.; Guo, W.; Yang, X.; Luo, L.; Jiao, W.; Hu, X.; Yu, Z.; Wang, C.; et al. 5G Ultra-Remote Robot-Assisted Laparoscopic Surgery in China. Surg. Endosc. 2020, 34, 5172–5180.
- Park, J.W.; Lee, D.H.; Kim, Y.W.; Lee, B.H.; Jo, Y.H. Lapabot: A Compact Telesurgical Robot System for Minimally Invasive Surgery: Part II. Telesurgery Evaluation. Minim. Invasive Ther. Allied Technol. 2012, 21, 195–200.
- Acemoglu, A.; Peretti, G.; Trimarchi, M.; Hysenbelli, J.; Krieglstein, J.; Geraldes, A.; Deshpande, N.; Ceysens, P.M.V.; Caldwell, D.G.; Delsanto, M.; et al. Operating From a Distance: Robotic Vocal Cord 5G Telesurgery on a Cadaver. Ann. Intern. Med. 2020, 173, 940–941.
- Tian, W.; Fan, M.; Zeng, C.; Liu, Y.; He, D.; Zhang, Q. Telerobotic Spinal Surgery Based on 5G Network: The First 12 Cases. Neurospine 2020, 17, 114–120.
- Morohashi, H.; Hakamada, K.; Kanno, T.; Kawashima, K.; Akasaka, H.; Ebihara, Y.; Oki, E.; Hirano, S.; Mori, M. Social Implementation of a Remote Surgery System in Japan: A Field Experiment Using a Newly Developed Surgical Robot via a Commercial Network. Surg. Today 2021, 52, 705–714.
- Huang, E.Y.; Knight, S.; Guetter, C.R.; Davis, C.H.; Moller, M.; Slama, E.; Crandall, M. Telemedicine and telementoring in the surgical specialties: A narrative review. Am. J. Surg. 2019, 218, 760–766.
- Fuertes-Guiró, F.; Vitali-Erion, E.; Rodriguez-Franco, A. A Program of Telementoring in Laparoscopic Bariatric Surgery. Minim. Invasive Ther. Allied Technol. 2016, 25, 8–14.
- Sachdeva, N.; Klopukh, M.; Clair, R.S.; Hahn, W.E. Using conditional generative adversarial networks to reduce the effects of latency in robotic telesurgery. J. Robot. Surg. 2021, 11, 635–641.
- Shabir, D.; Abdurahiman, N.; Padhan, J.; Trinh, M.; Balakrishnan, S.; Kurer, M.; Ali, O.; Al-Ansari, A.; Yaacoub, E.; Deng, Z.; et al. Towards Development of a Telementoring Framework for Minimally Invasive Surgeries. Int. J. Med. Robot. 2021, 17, e2305.
- Nguyen, N.T.; Okrainec, A.; Anvari, M.; Smith, B.; Meireles, O.; Gee, D.; Moran-Atkin, E.; Baram-Clothier, E.; Camacho, D.R. Sleeve gastrectomy telementoring: A SAGES multi-institutional quality improvement initiative. Surg. Endosc. 2018, 32, 682–687.
- Snyderman, C.H.; Gardner, P.A.; Lanisnik, B.; Ravnik, J. Surgical telementoring: A new model for surgical training. Laryngoscope 2016, 126, 1334–1338.
- Kirkpatrick, A.W.; Tien, H.; LaPorta, A.T.; Lavell, K.; Keillor, J.; Beatty, H.E.W.L.; McKee, J.L.; Brien, S.; Robert, D.J.; Wong, J.; et al. The marriage of surgical simulation and telementoring for damage-control surgical training of operational first responders: A pilot study. J. Trauma Acute Care Surg. 2015, 79, 741–747.
- Li, G.; Su, H.; Cole, G.A.; Shang, W.; Harrington, K.; Camilo, A.; Pilitsis, J.G.; Fischer, G.S. Robotic System for MRI-Guided Stereotactic Neurosurgery. IEEE Trans. Biomed. Eng. 2015, 62, 1077–1088.
- Louis, R.G.; Steinberg, G.K.; Duma, C.; Britz, G.; Mehta, V.; Pace, J.; Selman, W.; Jean, W.C. Early Experience with Virtual and Synchronized Augmented Reality Platform for Preoperative Planning and Intraoperative Navigation: A Case Series. Oper. Neurosurg. 2021, 21, 189–196.
- Ivan, M.E.; Eichberg, D.G.; Di, L.; Shah, A.H.; Luther, E.M.; Lu, V.M.; Komotar, R.J.; Urakov, T.M. Augmented Reality Head-Mounted Display–Based Incision Planning in Cranial Neurosurgery: A Prospective Pilot Study. Neurosurg. Focus 2021, 51, E3.
- De Momi, E.; Ferrigno, G.; Bosoni, G.; Bassanini, P.; Blasi, P.; Casaceli, G.; Fuschillo, D.; Castana, L.; Cossu, M.; Lo Russo, G.; et al. A Method for the Assessment of Time-Varying Brain Shift during Navigated Epilepsy Surgery. Int. J. Comput. Assist. Radiol. Surg. 2016, 11, 473–481.
- Kiarostami, P.; Dennler, C.; Roner, S.; Sutter, R.; Fürnstahl, P.; Farshad, M.; Rahm, S.; Zingg, P.O. Augmented Reality-Guided Periacetabular Osteotomy—Proof of Concept. J. Orthop. Surg. Res. 2020, 15, 540.
- Padilla, J.B.; Arango, R.; García, H.F.; Cardona, H.D.V.; Orozco, Á.A.; Álvarez, M.A.; Guijarro, E. NEURONAV: A Tool for Image-Guided Surgery—Application to Parkinson’s Disease. In International Symposium on Visual Computing; Springer: Cham, Switzerland, 2015; Volume 9474, pp. 349–358.
- Watanabe, E.; Satoh, M.; Konno, T.; Hirai, M.; Yamaguchi, T. The Trans-Visible Navigator: A See-Through Neuronavigation System Using Augmented Reality. World Neurosurg. 2016, 87, 399–405.
- Yoon, J.W.; Chen, R.E.; ReFaey, K.; Diaz, R.J.; Reimer, R.; Komotar, R.J.; Quinones-Hinojosa, A.; Brown, B.L.; Wharen, R.E. Technical Feasibility and Safety of Image-Guided Parieto-Occipital Ventricular Catheter Placement with the Assistance of a Wearable Head-up Display. Int. J. Med. Robot. Comput. Assist. Surg. 2017, 13, e1836.
- Fan, X.; Roberts, D.W.; Schaewe, T.J.; Ji, S.; Holton, L.H.; Simon, D.A.; Paulsen, K.D. Intraoperative Image Updating for Brain Shift Following Dural Opening. J. Neurosurg. 2017, 126, 1924–1933.
- Eftekhar, B. A Smartphone App to Assist Scalp Localization of Superficial Supratentorial Lesions--Technical Note. World Neurosurg. 2016, 85, 359–363.
- Hu, L.; Wang, M.; Song, Z. A Convenient Method of Video See-through Augmented Reality Based on Image-Guided Surgery System. In Proceedings of the 2013 Seventh International Conference on Internet Computing for Engineering and Science, Shanghai, China, 20–22 September 2013; Volume 2013, pp. 100–103.
- Guo, Z.; Dong, Z.; Lee, K.H.; Cheung, C.L.; Fu, H.C.; Ho, J.D.L.; He, H.; Poon, W.S.; Chan, D.T.M.; Kwok, K.W. Compact Design of a Hydraulic Driving Robot for Intraoperative MRI-Guided Bilateral Stereotactic Neurosurgery. IEEE Robot. Autom. Lett. 2018, 3, 2515–2522.
- Ushimaru, Y.; Takahashi, T.; Souma, Y.; Yanagimoto, Y.; Nagase, H.; Tanaka, K.; Miyazaki, Y.; Makino, T.; Kurokawa, Y.; Yamasaki, M.; et al. Innovation in Surgery/Operating Room Driven by Internet of Things on Medical Devices. Surg. Endosc. 2019, 33, 3469–3477.
