The clinical remount procedure, which involves remounting the dentures on an articulator with interocclusal records, can effectively reduce occlusal discrepancies. This procedure can be applied not only to new dentures but also to those already in service. Performing a clinical remount on these existing dentures would enhance the oral function of the denture wearer and would enable effective and accurate correction of the accumulated errors in the jaw relationship in a stable working environment. The clinical remount procedure should be performed if a patient has poor masticatory function or occlusion-related complaints. This procedure remains an essential skill both for fabricating quality dentures and maintaining those already in service.
- clinical remount
- complete denture
- malocclusion
1. Introduction
2. Hypothetical Model
The clinical remount procedure effectively and accurately corrects the accumulative errors of the jaw relationship.
The clinical remount procedure effectively and accurately corrects the accumulative errors of the jaw relationship.
2.1. Correction of the Accumulative Errors of Jaw Relationship
The first component of this model is ”correcting the accumulative errors of the jaw relationship.” Even when the prostheses were carefully balanced before delivery, many researchers have noted that discrepancies and malocclusion occur after the delivery of dentures. The reasons for the occlusal alterations can be classified into three categories: material factors, physiological changes and clinical practice. For the material factors, the acrylic denture base is porous, and mild distortion will occur due to absorption of water [21] (p. 159). Additionally, it is not uncommon to find worn occlusal surfaces on those dentures that had already served for a while [6][23]. For the physiological changes, factors including settling of the dentures [21] (p. 159), neuromuscular adjustment [14], edentulous ridge resorption [23][24] and denture wearing habits [24] were reported in previous studies. Last but not least, occlusal alterations will also occur due to adjustments carried out by clinicians in recall appointments. Long-term cephalometric evaluation also shows that complete dentures exhibit a counterclockwise rotation and forward movement mainly because of soft tissue seating [25] or efforts made by patients to retain poorly fitting, worn-out prostheses [26]. The clinical remount procedure should be understood as an extraoral method to establish occlusion and articulation of the prostheses at any designated position according to the bite registration; however, if the original jaw relationship is difficult to duplicate [6] or is unstable, it is safer to re-establish the articulation of the used prostheses as close to the centric relation (CR) as possible. CR is widely considered to be the starting point of mandibular movement with reproducibility. From this position, the mandible can perform lateral and anterior eccentric movements [27][28]. Articulating the prostheses as close to the CR as possible maximizes the possibility that the mandibular movement coincides with the set articulation of the prostheses. This strategy also reduces the chance of horizontal deviation because the lateral movement border of the mandible converges gradually while retruding. Thus, the prostheses are more likely to be stabilized during the masticatory cycle (Figure 1) [29][30].
Figure 1
. Diagram showing the advantage of setting the occlusion and articulation of dentures in the centric relation (CR). The original figures come from Posselt and Gibbs and Lundeen.
2.2. Selective Grinding on the Articulator
The second component of this model is “performing selective grinding on a stable platform.” Compared with the process of adjusting the occlusion in the patient’s mouth directly, the clinical remount procedure provides a solid, clean, saliva-free and easily accessible working environment. This procedure also reduces patient participation and alleviates psychological pressure [1] (p. 397). Although the thickness of the articulating paper may vary from 25 to 100 μm, the physiological displacement of the edentulous ridge has been reported to be larger than 500 μm [3][4]. Research has indicated that compared with evaluating the occlusion of dentures on an articulator, marking the occlusal contact points with articulating paper in the patient’s mouth directly creates more spurious and false marks, regardless of whether the dentures have been stabilized [5][6]. Furthermore, it is difficult to check the occlusal status of each pair of molars individually intraorally. Mpungose et al. [7] established the low accuracy and poor reliability of evaluating the occlusal status by visual inspection only. The false, unclear marks lead to unnecessary grinding of the artificial teeth, decreasing the longevity of the dentures. Additionally, edentulous patients today have different characteristics than those of earlier times, including greater mean age, more ridge resorption and increased loss of oral awareness and dexterity. These negative factors make an accurate and repeatable jaw relationship difficult to achieve. Last but not least, protracted treatment time and intimate recalls may be unfavored for the edentulous patients nowadays because of greater age and impaired general health [31][32]. Achieving the same extent of occlusal adjustment as the clinical remount procedure at the chairside directly would involve a challenging and lengthy appointment. From the patient’s perspective, the use of the clinical remount procedure means that chairside procedures can be shortened, and the repeated procedure of inserting and retrieving dentures between each grinding can be avoided. The reduction in patient participation also grants the clinical remount procedure more versatility. Some researchers have raised doubts about the necessity of the clinical remount procedure, particularly those focused on simplifying the fabrication of new complete dentures [32][33][34][35][36][37]. With carefully determined vertical and horizontal jaw relationships, newly fabricated complete dentures seem to serve patients well even without the clinical remount procedure. Nevertheless, as previously discussed, an accumulation of errors in the jaw relationship seems inevitable. Because of the unknown extent of errors in the jaw relationship of dentures already in use, the scholars believe that the clinical remount procedure should be undertaken to re-establish the occlusion and articulation if indicated. Other researchers may doubt that an articulator can exactly duplicate mandibular movement. Discrepancies cannot be denied, and minor refinements may be needed even if the remounting procedure is carefully performed. However, as mentioned previously, the use of articulators reduces the number of chairside adjustments required [38]. Additionally, the scholars believe that the repeatable eccentric movements of an articulator and the solid working environment make it easier to establish a credible broad zone of bilateral balanced articulation [27]. As Heartwell and Rahn claimed, the remaining discrepancies are so negligible that the resilience of the supporting tissues accommodates for the error [1] (p. 399). The resilience of the supporting tissue in conventional complete denture treatment is a double-edged sword. Although the resilience of tissues hinders accurate adjustments from being carried out intraorally, this property also helps patients cope with the minor occlusal interferences of their dentures. One of the goals of clinical remounting is to minimize occlusal discrepancies and make those discrepancies minor enough for the supporting tissue to compensate.3. Indications and Contraindications
3.1. Indications
The first indication is that the complaint is caused by occlusal discrepancies. Dentures with good retention but ones that become loose after conversation or chewing are likely to have faulty occlusion and articulation. Patients seldom complain precisely about the occlusion of their dentures, but they may complain about food being trapped between the ridge and the denture or uncertain sore spots without ulceration. As Heartwell and Rahn stated, one must assume that there are occlusal faults in all complete dentures until proven otherwise [1] (p. 394). The second indication is poor masticatory function. Some patients have no complaints about their dentures because they have already given up chewing with their dentures. Patients may change their diet or swallow larger boluses of food to cope with decreased masticatory function [39][40][41]. Functional impairment may also not be recognized by patients. Masticatory function was previously evaluated with a reliable test food, such as carrots or peanuts, with the sieve method [37]. However, the complicated procedure of the sieve method is difficult to carry out in daily practice. Recently, a simplified but similar gummy testing kit has become commercially available in Japan and has been formally adopted as a diagnostic tool for oral hypofunction by the Japan Univeral Health Insurance Coverage System (JUHICS) [42]. Verifying masticatory function with the gummy testing kit or other standardized foods, such as a certain brand of cookie, may help clinicians gather objective information about masticatory function. If a patient is diagnosed with poor masticatory function, performing the clinical remount procedure on the existing dentures may serve as a good starting point for the rehabilitation of oral function.3.2. Contraindications
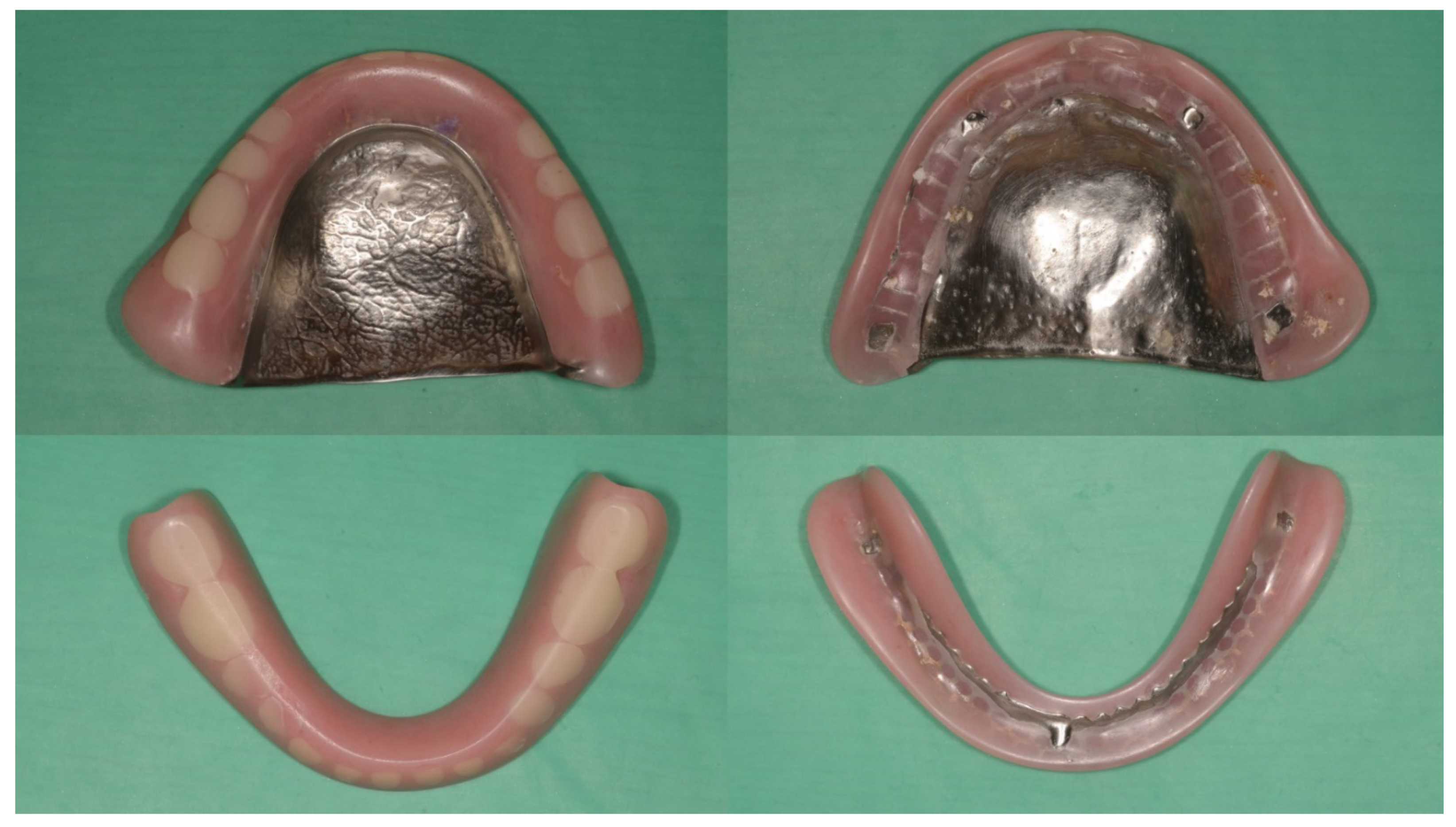
The treatment efficiency of the clinical remount procedure may be limited if either of two following clinical findings is noted: an extreme anterior–posterior discrepancy between the maximal intercuspal position (MIP) and the centric relation (CR) or an extremely low vertical dimension. An extreme amount of anterior–posterior discrepancy between MIP and CR will hinder the treatment efficiency of the clinical remount procedure. If the occlusion of the denture is re-established in CR, as previously described, the overlapping area of the maxillary and mandibular arches will be heavily restricted owing to the anatomical shape of the human dental arches. Adequate posterior support may be difficult to acquire in such a confined area; thus, the adjusted dentures cannot be well stabilized (Figure 2).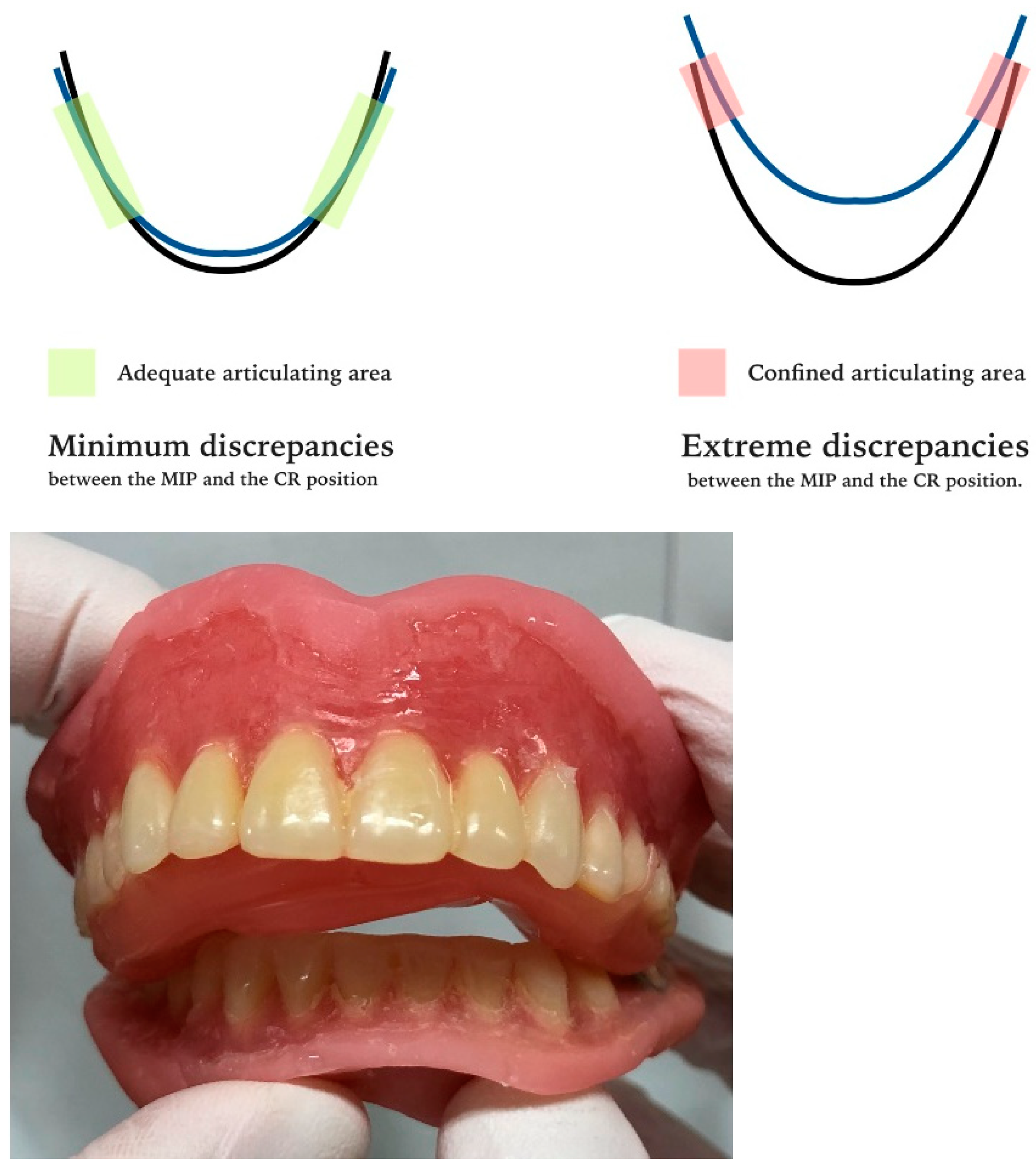
4. Conclusions
This hypothetical model portrays a possible mechanism for performing the clinical remount procedure on existing complete dentures. The accumulated errors of the jaw relationship can be corrected effectively and accurately in a stable working environment. The clinical remount procedure is suitable for correcting the occlusion of existing dentures and should be performed if a patient has poor masticatory function or occlusion-related complaints.
This hypothetical model portrays a possible mechanism for performing the clinical remount procedure on existing complete dentures. The accumulated errors of the jaw relationship can be corrected effectively and accurately in a stable working environment. The clinical remount procedure is suitable for correcting the occlusion of existing dentures and should be performed if a patient has poor masticatory function or occlusion-related complaints.
References
- Heartwell, C.M., Jr.; Rahn, A.O. Denture insertion. In Syllabus of Complete Denture, 4th ed.; Lea & Febiger: Philadelphia, PA, USA, 1986; pp. 391–406.
- Fenlon, M.R.; Sherriff, M. An investigation of factors influencing patients’ satisfaction with new complete dentures using structural equation modeling. J. Dent. 2008, 36, 427–434.
- Compagnoni, M.A.; de Souza, R.F. Kinesiographic study of complete denture movement related to mucosa displacement in edentulous patients. Pesqui. Odontol. Bras. 2003, 17, 356–361.
- Maeda, Y.; Okada, M.; Makishi, A.; Nokubi, T.; Okuno, Y.; Aoki, T. Using mandibular kinesiograph for measuring complete denture movements a preliminary report. J. Osaka Univ. Dent. Sch. 1984, 24, 123–129.
- Atashrazm, P.; Ansari, L.H.; Khorsand, M. An evaluation of occlusal contacts of remounted complete denture before final occlusal adjustment. Shiraz Univ. Dent. J. 2009, 9, 1–5.
- Wilson, J.; Rees, J.S. Comparison of interocclusal contacts registered intraorally and after a remount procedure in complete denture patients. Eur. J. Prosthodont. Restor. Dent. 2006, 14, 146–150.
- Mpungose, S.K.; Geerts, G.A. Analyzing Complete Denture Occlusal Contacts: Accuracy and Reliability. Int. J. Prosthodont. 2016, 29, 50–52.
- Murphy, W.M.; Bates, J.F.; Huggett, R. Complete denture construction in general dental practice. A survey. Br. Dent. J. 1971, 130, 514–521.
- Harrison, A.; Huggett, R.; Murphy, W.M. Complete denture construction in general dental practice: An update of the 1970 survey. Br. Dent. J. 1990, 169, 159–163.
- Hickey, J.C.; Boucher, C.O.; Woelfel, J.B. Responsibility of the dentist in complete dentures. J. Prosthet. Dent. 1962, 12, 637–653.
- Holt, J.E. Research on remounting procedures. J. Prosthet. Dent. 1977, 38, 338–341.
- Firtell, D.N.; Finzen, F.C.; Holmes, J.B. The effect of clinical remount procedures on the comfort and success of complete dentures. J. Prosthet. Dent. 1987, 57, 53–57.
- Gutowski, A.; Dent, M. Remounting and occlusal adjustment of complete dentures. J. Gnathol. 1990, 9, 9–22.
- Utz, K.H. Studies of changes in occlusion after the insertion of complete dentures. Part I. J. Oral Rehabil. 1996, 23, 321–329.
- Badel, T.; Ćelić, R.; Kraljević, S.; Pandurić, J.; Dulčić, N. Complete denture remounting. Acta Stomat. Croat. 2001, 35, 381–387.
- Al Quran, F. A clinical evaluation of the clinical remount procedure. J. Contemp. Dent. Pract. 2005, 6, 48–55.
- Shigli, K.; Angadi, G.S.; Hegde, P. The effect of remount procedures on patient comfort for complete denture treatment. J. Prosthet. Dent. 2008, 99, 66–72.
- Mostafa, M.M.M.; Ezzat, A. Effect of clinical remount procedures on masticatory muscle activity and comfort of complete denture wearers. Curr. Sci. Int. 2019, 8, 25–41.
- Verhaeghe, T.V.; Linke, B.A.; Cable, C.E.; Mostafa, N. Clinical remounting of complete dentures: A systematic review. J. Prosthet. Dent. 2019, 121, 604–610.
- Neil, E. Delivering the case. In Full Denture Practice; Marshall & Bruce Co.: Nashville, TN, USA, 1932; pp. 110–113.
- Lauritzen, A.G. Technique for functional analysis and balancing of occlusion in full denture prostheses. In Atlas of Occlusal Analysis; HAH Publications: Colorado Springs, CO, USA, 1974; pp. 159–228.
- Felton, D.; Cooper, L.; Duqum, I.; Minsley, G.; Guckes, A.; Haug, S.; Meredith, P.; Solie, C.; Avery, D.; Chandler, N.D. Evidence-Based Guidelines for the care and maintenance of complete dentures: A publication of the American College of Prosthodontists. J. Prosthodont. 2011, 20, S1–S12.
- Utz, K.H. Studies of changes in occlusion after the insertion of complete dentures (Part II). J. Oral Rehabil. 1997, 24, 376–384.
- Schierano, G.; Arduino, E.; Bosio, E.; Preti, G. The influence of selective grinding on the thickness discrimination threshold of patients wearing complete dentures. J. Oral Rehabil. 2002, 29, 184–187.
- Tuncay, O.C.; Thomson, S.; Abadi, B.; Ellinger, C. Cephalometric evaluation of the changes in patients wearing complete dentures. A ten-year longitudinal study. J. Prosthet. Dent. 1984, 51, 169–180.
- Ciftçi, Y.; Kocadereli, I.; Canay, S.; Senyilmaz, P. Cephalometric evaluation of maxillomandibular relationships in patients wearing complete dentures: A pilot study. Angle Orthod. 2005, 75, 821–825.
- The Glossary of Prosthodontic Terms: Ninth Edition. J. Prosthet. Dent. 2017, 117, e1–e105.
- Wiens, J.P.; Goldstein, G.R.; Andrawis, M.; Choi, M.; Priebe, J.W. Defining centric relation. J. Prosthet. Dent. 2018, 120, 114–122.
- Posselt, U. Movement areas of the mandible. J. Prosthet. Dent. 1957, 7, 375–385.
- Gibbs, C.H.; Lundeen, H.C. Jaw movements and forces during chewing and swallowing and their clinical significance. In Advances in Occlusion; John Wright-PSG Inc.: Boston, MA, USA, 1982; pp. 2–32.
- Ivanhoe, J.R.; Cibirka, R.M. Treating the modern complete denture patient: A review of the literature. J. Prosthet. Dent. 2002, 88, 631–635.
- Ye, Y.; Sun, J. Simplified Complete Denture: A Systematic Review of the Literature. J. Prosthodont. 2017, 26, 267–274.
- Kawai, Y.; Murakami, H. Do traditional techniques produce better conventional complete dentures than simplified techniques? J. Dent. 2005, 33, 659–668.
- Kawai, Y.; Muarakami, H.; Feine, J.S. Do traditional techniques produce better conventional complete dentures than simplified techniques? A 10-year follow-up of a randomized clinical trial. J. Dent. 2018, 74, 30–36.
- Hickey, J.C.; Henderson, D.; Straus, R. Patient response to variations in denture technique. I. Design of a study. J. Prosthet. Dent. 1969, 22, 158–170.
- Ellinger, C.W.; Somes, G.W.; Nicol, B.R.; Unger, J.W.; Wesley, R.C. Patient response to variations in denture technique. Part III: Five-year subjective evaluation. J. Prosthet. Dent. 1979, 42, 127–130.
- Wesley, R.C.; Ellinger, C.W.; Somes, G.W. Patient response to variations in denture techniques. Part VI: Mastication of peanuts and carrots. J. Prosthet. Dent. 1984, 51, 467–469.
- Koyano, K.; Tsukiyama, Y. Rehabilitation of occlusion—Science or art? J. Oral Rehabil. 2012, 39, 513–521.
- Banerjee, R.; Chahande, J.; Banerjee, S.; Radke, U. Evaluation of relationship between nutritional status and oral health related quality of life in complete denture wearers. Indian J. Dent. Res. 2018, 29, 562–567.
- Su, Y.; Yuki, M.; Hirayama, K.; Sato, M.; Han, T. Denture Wearing and Malnutrition Risk Among Community-Dwelling Older Adults. Nutrients 2020, 12, 151.
- Ettinger, R.L. Changing dietary patterns with changing dentition: How do people cope? Spec. Care Dent. 1998, 18, 33–39.
- Minakuchi, S.; Tsuga, K.; Ikebe, K.; Ueda, T.; Tamura, F.; Nagao, K.; Furuya, J.; Matsuo, K.; Yamamoto, K.; Kanazawa, M.; et al. Oral hypofunction in the older population: Position paper of the Japanese Society of Gerodontology in 2016. Gerodontology 2018, 35, 317–324.
