Immunotherapy research has often focused on CD8+ T cells because of their ability to eliminate tumor cells. However, CD4+ T cells have attracted attention in the field because they are not only crucial for promoting CD8+ T cell functions, preventing CD8+ T cell depletion or inducing CD8+ T cell memory, but also able to directly or indirectly kill tumor cells [50].
1. Regulatory T (Treg) Cells
In addition to effector cells, the T lymphocyte family includes an immunomodulatory subgroup called Treg cells, whose role is to negatively regulate other immune cells, prevent the overactivation of the immune response, and play a role in a wide range of diseases, such as allergies, chronic infections, and parasitic infections
[1][51]. However, the presence of Treg cells is disadvantageous to hosts with tumors because they limit an effective antitumor immune response. Kamada et al.
[2][52] reported that the proportions of effector regulatory T (eTreg) cells/CD8 T cells, Ki67 Treg cells/Ki67CD8 T cells, and Ki67 Treg cells decreased significantly in non-HPD patients after treatment with anti-PD-1 antibodies, while these proportions in HPD patients remained stable or even increased slightly. This finding suggested that if the number of CD8 T cells is insufficient to overcome Treg cells, the possibility of HPD development is greatly increased. Furthermore, Treg cells have also been shown to express immune checkpoints, such as PD-1; thus, Treg cells can also be targeted by anti-PD-1 agents
[3][53]. Researchers have observed that knocking out PD-1 in Treg cells or blocking PD-1 with monoclonal antibodies (mAbs) caused Treg cells to gain a stronger proliferative ability and a stronger immunosuppression ability, thus leading to a stronger ability to promote tumor growth. This finding suggested that PD-1 Treg cells play a key role in anti-PD-1 treatment-mediated HPD in advanced gastric cancer. In addition, Ratner et al.
[4][5][37,54] demonstrated that nivolumab led to rapid progression in patients with adult T-cell leukemia/lymphoma (ATLL). They identified a novel relationship between tumor-resident Tregs and ATLL cells and revealed the tumor suppressive effect of PD-1 in ATLL.
+++++++Furthermore, in Treg cells treated with PD-1 blockade, the expression of immune checkpoints is upregulated, and the immunosuppressive function is enhanced. Thus, the antitumor immunity of some patients after anti-PD-1 treatment is not enhanced but greatly weakened, which leads to the occurrence of HPD. Interestingly, CTLA-4 was found to be strongly expressed in Treg cells
[6][55]. Anti-CTLA-4 treatment increased the presence of Ki67 Treg cells
[2][52]. Furthermore, the combination of anti-CTLA-4 antibodies and anti-PD-1 antibodies was associated with a lower incidence of HPD than other ICI combinations, and CTLA-4, OX-40, or CCR4-targeted therapy might be a strategy for preventing HPD through Treg cell consumption
[7][56]. In addition, selective PD-1/PD-L1 inhibition may lead to tumor immune evasion and accelerate tumor growth by increasing the number of Treg cells infiltrating and circulating in the tumor
[8][57].
+2. Other Subsets of CD4 T Cells+
CD4CD28
+− T cells are a cell subpopulation with unique biological effects that frequently appear in some autoimmune diseases
[9][58]. Due to their lack of CD28, which is necessary for a cell-specific immune response and the most important costimulatory molecule on the T-cell surface, these unique cells not only have abnormal immune function but also have the characteristics of autoreactivity, massive expansion, and a long lifespan
[10][59]. Arasanz et al.
[11][60] found that CD4CD28
+− T cells in the peripheral blood of lung cancer patients with HPD were amplified after PD-1 treatment, and high tumor growth dynamics scores were associated with the presence of CD4CD28
+− T-cell subsets in patients with HPD.
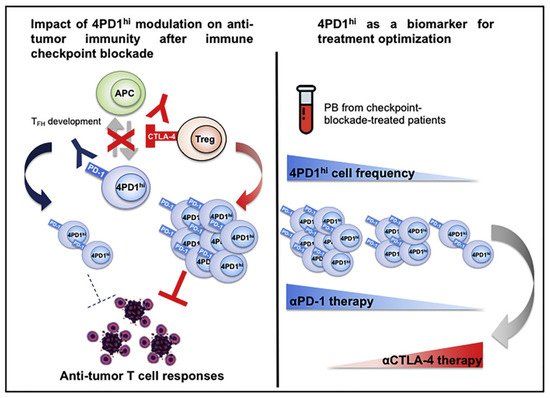
In addition, Zappasodi et al.
[12][61] observed in melanoma mice that a subset of CD4Foxp3
+−PD-1
high T cells can perform immunosuppressive functions similar to those of Treg cells, but their RNA expression levels may be more similar to those of follicular helper T (Tfh) cells. Interestingly, while anti-PD-1 treatment reduced the numbers of these cells, anti-CTLA4 treatment increased their intratumoral abundance. This result suggests that this cell subpopulation could also respond to ICB, proliferate under anti-CTLA-4 treatment, and acquire negative regulatory immune properties, which might contribute to the development of HPD
(Figure 1).
Figure 1. Zappasodi et al. illustrated the function of 4PD1hi cells (PD-1+CD4+Foxp3- T cells) and observed that these cells accumulate within the tumor as a function of the tumor burden. Reprinted with permission from Ref. [61]. 2018, Elsevier.
3. Exhausted CD4+ T Cells
Another potential mechanism of HPD is the correlation between exhausted CD4+ T cells and anti-PD-1 treatment. The current understanding of CD4+ T cell exhaustion is obviously insufficient. However, the negative effects of CD4+ T cell exhaustion on proliferation, cytokine production, B-cell help, and CD8+ effector functions have been reported. Furthermore, exhausted CD4+ T cells upregulate immune-regulatory proteins, such as TIM3 and PD-1, paralleling phenotypes observed in exhausted CD8+ T cells [13][62]. Unlike non-HPD patients, HPD patients showed abnormal dilation of peripheral exhausted memory CD4+ T cells after the initial administration of anti-PD-1/PD-L1 antibodies [14][60]. Arasanz et al. [14][60] monitored peripheral blood mononuclear cells (PBMCs) in NSCLC patients treated with anti-PD-1/PD-L1 antibodies, and peripheral exhausted CD4+ T-cell proliferation was observed in patients with HPD. They proposed that the rapid expansion of peripheral CD28-CD4+ T cells is an early distinguishing feature of ICIs-induced HPD in NSCLC. Although the role of exhausted CD4+ T cells is not fully understood, these studies provide important evidence that these cells might also contribute to the progression of HPD.
4. IFN-γ
While IFN-γ is considered to be a key factor in antitumor immunity [15][16][63,64], Xiao et al. [17][65] demonstrated that IFN-γ could promote immune escape and papilloma development by enhancing a Th17-associated inflammatory reaction. Thus, IFN-γ can promote either antitumor immunity or immune escape according to the pathological background and the level of selective stress [18][66]. Sakai et al. [19][67] reported that in a mouse model of Mycobacterium tuberculosis infection, PD-1- led to the extensive penetration of CD4+ T cells into the lung parenchyma and the production of large amounts of IFN-γ, causing rapid disease progression, compared with that observed in wild-type mice. In addition, mutations in genes encoding IFN-γ signaling pathway components, such as IFN-γ receptor and JAK1/2, have been identified as potential mechanisms of resistance against anti-PD-1/PD-L1 and anti-CTLA-4 antibodies [16][20][64,68]. Champiat et al. [21][40] noted that T-cell behavior in the TME under ICB may be affected by mutations that affect the IFN-γ signaling pathway, particularly mutations in JAK1/2. JAK1/2 mutations have been proven to be associated with primary resistance to ICIs [22][69]. In addition, it has been reported that IFN-γ-induced interferon regulatory factor 8 (IRF-8) binds to its promoter and induces MDM2 overexpression [23][24][70,71]. MDM2 is a protein involved in p53 degradation and inhibition, and its amplification is often observed in HPD patients [23][70].