Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Gregory P Conners and Version 2 by Conner Chen.
The optimal management of foreign body ingestion in children depends on an understanding of its natural history and risks of complication. The large majority of swallowed foreign bodies pass uneventfully through the gastrointestinal (GI) tract. However, complications, sometimes serious, may occur. The wide variety among patients and among the foreign bodies that they swallow makes creation of universal protocols complicated and difficult. Thus, the evaluation of a patient after potential foreign body ingestion requires a balanced approach, identifying and addressing potentially problematic ingestions without overtesting or overtreating.
- foreign body
- ingestion
- pediatric
1. Introduction
The optimal management of foreign body ingestion in children depends on an understanding of its natural history and risks of complication. The large majority of swallowed foreign bodies pass uneventfully through the gastrointestinal (GI) tract. However, complications, sometimes serious, may occur. The wide variety among patients and among the foreign bodies that they swallow makes creation of universal protocols complicated and difficult. Thus, the evaluation of a patient after potential foreign body ingestion requires a balanced approach, identifying and addressing potentially problematic ingestions without overtesting or overtreating.
2. Risk of Complication: Patient Factors
Most swallowed foreign bodies are either unrecognized or managed at home without medical intervention [1]. Children who present to an Emergency Department after foreign body ingestion are at higher risk of complications than those managed at home or exclusively by primary care physicians [2].
Complications are most common when the patient, the swallowed foreign body, or both, is associated with higher risk than usual. Abnormal GI motility due to either functional or anatomic variation, such as esophageal or duodenal stenosis or previous surgery, is an important patient risk factor [3]. Affected patients are at risk of impaction of the foreign body at the site of the abnormality. Thus, children who have, for example, undergone previous trachea-esophageal fistula repair, are at risk of esophageal impaction at the repair site, while those with Down syndrome (which carries a substantial risk of associated duodenal stenosis) are at higher risk of duodenal impaction [4][5][6][4,5,6]. A swallowed object is more likely to become impacted at the pylorus of a child who has had surgery to repair pyloric stenosis [7]. Children with previous complications of foreign body ingestion, especially esophageal impaction, are at an increased risk of recurrence [3]. Although complications are likelier in children with known GI tract abnormalities, it should be noted that many children who suffer complications of foreign body ingestion do not have previously identified risk factors. In some instances, this points to a previously unsuspected anatomic or functional GI tract diagnosis. Objects that are known to have been lodged in the esophagus for 72 h or more, or those found incidentally, are strongly associated with esophageal injury [8].
3. Risk of Complication: Foreign Body Factors
Foreign bodies that are generally considered chemically inert, such as coins, may provoke reactions in some children, such as those with nickel sensitivity [9]. Very small objects, such as small pills, may become adherent to the esophageal mucosa; some will exert a corrosive effect. Foreign bodies that are several centimeters long, such as a spoon or toothbrush, are unlikely to pass beyond the upper GI tract, and will therefore require endoscopic removal. These patients may also require behavioral health evaluation, as ingestions of long objects have been associated with the self-induced vomiting of bulimia nervosa [10]. Swallowed foreign bodies with a sharp edge, such as a razor blade, pose a risk of damage to the GI tract. Swallowed objects with a sharp point create a risk of perforation; sewing needles in particular are commonly associated with stomach and bowel perforation, while fish bones or push pins may become impaled in the esophagus [11][12][13][11,12,13]. Surgical intervention may be required.
Button batteries (also known as disk batteries) pose a substantial risk of mucosal damage when they become lodged in a moist environment, such as the esophagus, naris, external ear canal, vagina, or umbilicus; batteries that are steadily progressing through the GI tract are typically not associated with injury. Even discarded, partially depleted batteries may create electrical current sufficient to cause substantial tissue damage in an hour or less. Missed esophageal button batteries have been associated with fatal hemorrhage due to created aorto-esophageal fistula, or important injury to the upper airway. Larger, lithium batteries have been most commonly associated with rapid, substantial injury, but all button batteries carry risk of injury [14]. Early administration of honey (10 mL every ten minutes; not recommended for children in the first year of life) was recently recommended to help reduce injury in children who have potentially swallowed lithium button batteries that have lodged in the esophagus, based on cadaver and animal research [15]. Sucralfate was also effective [16]. Management of swallowed button batteries is further discussed below; the National Battery Ingestion Hotline at 800-498-8666 can also provide guidance [15].
Swallowed small, toy magnets have led to multiple reports of intestinal damage [17][18][17,18]. When multiple magnets pass separately through the GI tract, they can powerfully attract each other, eroding tissues between them, leading to gastrointestinal perforation or creation of an entero-enteric fistula [19]. Swallowed small magnets and other metallic objects may cause similar injury. A dangerous variation is the co-ingestion of a small magnet and a button battery; the combination of physical tissue erosion due to the strong magnetic attraction with the damage due to local electrical currents may lead to substantial injury [20].
Coins are, by far, the swallowed foreign bodies most commonly brought to medical attention [8]. Thus, there has been substantial literature on coin ingestion. In the United States, children swallow far more pennies than other coins [21]. While the majority pass through the GI tract without complication, it is not uncommon for a previously healthy child to have a swallowed coin lodge in the esophagus. About 70% of coins (and similarly-shaped objects) lodge at the upper esophagus, corresponding to the area between the clavicles on frontal radiographs (Figure 1) [21]. The remainder are found lodged with about equal frequency in the mid-esophagus (Figure 2) or at the lower esophageal sphincter (Figure 3). While one-third to one-half of coins in the mid-esophagus or at the lower esophageal sphincter will pass into the stomach spontaneously in minutes to hours, especially in conjunction with oral intake, it is less common for upper esophageal coins to progress spontaneously [21]. Coins that lodge in the esophagus may partially or completely obstruct the esophagus, causing inability to swallow, or cause complications due to local pressure necrosis on the esophageal mucosa. While coins may remain in the esophagus for long periods, even years, with minimal symptoms, some migrate into the mediastinum or structures of the chest, including the aorta, with important morbidity, such as mediastinitis or creation of an aorto-esophageal fistula [8]. Occasionally, a radiograph performed in evaluation of cough, fever, dysphagia, failure to thrive, or other complaint will reveal an unexpected esophageal coin. It is often difficult to determine how long the coins have been in place. These coins may be associated with esophageal scarring, and/or have migrated into other chest structures [8]. Management will require subspecialty consultation, and likely endoscopic or surgical removal.

Figure 1. Chest radiograph showing a coin lodged in upper esophagus. Details suggesting it is a United States dime are visible on close inspection (photo courtesy of Timothy Johnson, DO, MMM).

Figure 2.
Chest radiograph showing swallowed hardware (washer) lodged in the mid-esophagus.
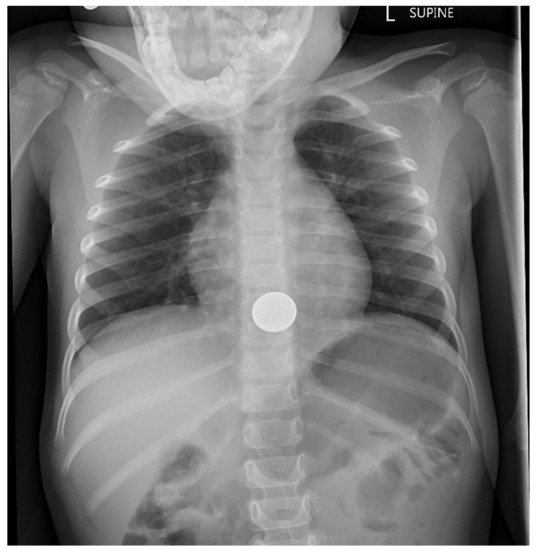
Figure 3. Chest radiograph showing coin lodged at lower esophageal sphincter.
Chest radiograph showing coin lodged at lower esophageal sphincter (photo courtesy of Marcus Rivera, MD).
