Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Dragos Catalin Jianu and Version 2 by Beatrix Zheng.
Cerebral venous thrombosis (CVT) is a relatively rare disorder in the general population and is frequently misdiagnosed upon initial examination. The knowledge of wide clinical aspects and imaging signs will be essential in providing a timely diagnosis.
- cerebral veins and dural sinuses thrombosis (CVT)
- thrombophilia
- headache
- native and contrast-enhanced Head Computed Tomography (CT)
- Magnetic Resonance Imaging (MRI) of the Head
1. Epidemiology
No epidemiologic studies of cerebral venous thrombosis (CVT) own the needed criteria for a good quality epidemiologic stroke study, due to multiple factors, including the wide clinical spectrum of CVT, frequently with subacute onset [1][2][3][6,11,12].
CVT represents only less than 1% of all strokes [3][12], its prevalence is higher than previously noted, due to an increased awareness of this type of disease among clinicians, and to improved and more accessible imaging methods, including Magnetic Resonance Imaging (MRI)/MR Venography (MRV)I/MRV, for the examination of patients with unclear neurological clinical aspects, such as headache and seizures [1][2][3][4][5][6,11,12,13,14].
Annual incidence is noted to be between 0.22 to 1.57 per 100,000 citizens [2][11] and is sex-independent in children and the elderly [1][6][6,7]. CVT is more frequent in children (especially in neonates) than in adults [1][6][6,7]. In adults, CVT is observed in patients who are younger on average than those with arterial types of stroke [1][6]. Thus, in the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT) cohort, the median age was 37 years [6][7], and only 8% of the patients were older than 65 [7][15]. Compared with men, women were significantly younger (median age of 34 years, vs. 42 years for men) [4][13]. In adult cases of the ISCVT cohort, CVT presented a female predominance (3:1) [8][9], which was higher between 31 to 50 years because of augmented risk attributed to a prothrombotic condition [1][6][6,7].
2. Etiology-Risk Factors
The most frequent risk factors detected in elder people with CVT are thrombophilia, neoplasms, and hematologic disorders [7][9][15,16].
In the Canadian pediatric ischemic stroke registry, a risk factor was detected in 98% of the children. Thrombophilia was found in 41% of all cases. In infants older than four weeks of age and children head and neck diseases, especially infections and chronic systemic diseases (e.g., connective tissue diseases, hematologic disorders, or malignancy) were frequent [10][17].
Different factors can determine or predispose adults to develop CVT (in 85% of cases at least one risk factor can be found), and in about half of CVT cases, they present multiple risk factors. For this reason, the detection of a cause or a risk factor should not stop a search for others [6][7]. The most common risk factors are represented by: genetic thrombophilia, oral contraceptives (OC), pregnancy, puerperium, malignancy, and infections [3][6][7,12]. Thus, a prothrombotic condition was detected in one-third of all cases of the ISCVT cohort, and a genetic thrombophilia was reported in 22% of all cases [6][7].
3. Pathophysiology
The main two pathophysiological mechanisms implied in CVT are diminution of CSF absorption, and increase of venular and capillary pressure [11][12][13][14][3,49,50,51] (Figure 12).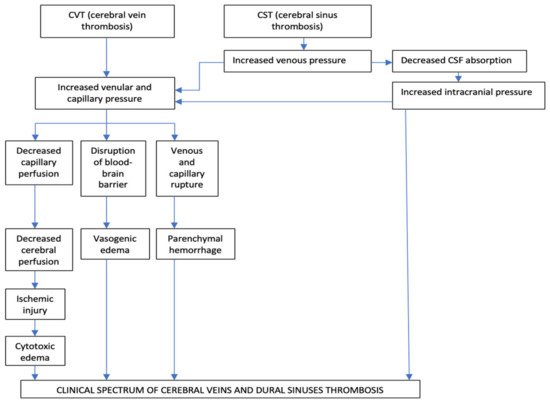
Figure 12.
Pathophysiology of cerebral veins and dural sinuses thrombosis.
The Occlusion of the Intracranial Dural Sinuses May Determine a Diminution of CSF Absorption
The normal absorption of CSF is produced through arachnoid granulations, especially at the level of the SSS and LS. In the particular situation of dural sinuses occlusion, especially of the SSS and LS, appears a raise of the cerebral venous pressure, with subsequent diminution of CSF absorption which, consecutively, increases the intracranial pressure. This pathologic process produces a rise in venular and capillary hypertension and generates vasogenic and cytotoxic edema and cerebral hemorrhage [11][12][13][14][3,49,50,51]. The second mechanism is represented by the progressive increase of venular and capillary pressure. This mechanism is the result of the thrombosis of dural sinuses and cerebral veins [11][12][13][14][3,49,50,51]. In the initial stages of venous obstruction, a diminished but still efficient perfusion of the correspondent brain tissue might be possible, due to the collateral venous circulation, which produces a significant degree of compensation, with consecutive neutralization of the pathological pressure modifications. For this reason, the corresponding areas of the brain can be functionally and metabolically affected, but not irreversibly injured [11][12][13][14][3,49,50,51]. As loco-regional venous pressure continues to increase, in the context of an ineffective collateral venous circulation, a rise of the thrombosis within cortical venous tributaries will reduce the cerebral perfusion pressure even more. Consequently, it will appear damage to the blood-brain barrier producing vasogenic edema, local ischemic lesions, cytotoxic edema, and venous and capillary lesions with consecutively parenchymal hemorrhage and, rarely, subarachnoid hemorrhages [11][12][13][14][3,49,50,51]. The diminution of the venous drainage consecutive to CVT determines raised venous pressure, with the backup of the fluid into the brain, producing vasogenic edema. This type of edema is situated within the extracellular compartment of the encephalic white matter/inside the glial cells, under the control of the hydrostatic pressure (augmented blood pressure and local blood flow) and osmotic gradients. Usually, the vasogenic edema does not produce neuronal lesions, because the fluid in excess in the extracellular space can, frequently, be removed [11][12][13][14][3,49,50,51]. Cytotoxic edema is produced by energy failure with a displacement of ions and water across the cell membranes into neurons. The intracellular edema, caused by ischemia, determines a great volume of dead or dying brain neurons with a bad prognosis [11][12][13][14][3,49,50,51]. In cerebral venous infarcts, the vasogenic edema represents the majority in comparison with the cytotoxic edema; these pathological aspects identified by diffusion-weighted imaging (DWI) confirm that the venous infarcts differ from arterial ones and present a significantly better recovery [12][13][14][15][1,49,50,51]. Brain edema and associated augmented intracranial pressure produce headache, vomiting, and diminished consciousness, but the most severe complications are represented by the pressure differences and the potential risk for brain herniation, which can determine death due to probable pressure-related lesions to neighboring areas [15][1]. The growth of the venous and capillary pressures produces vessel lesions and erythrocytes diapedesis due to disruptions of the blood-brain barrier both resulting in cerebral hemorrhage. The neuronal lesions determined by the cerebral hemorrhage induced by CVT are often milder than the damages induced by arterial infarcts [11][12][13][14][3,49,50,51]. Histological exam in CVT cases notes dilated cerebral veins, brain edema with flattened gyri, diminished sulci, compressed small ventricles, and ischemic neuronal lesions. The thrombus inside the cerebral veins is similar to other venous thrombi (when it is fresh, it presents a rich content in red blood cells and fibrin and a poor content in platelets; and, when it is chronic, it is replaced by fibrous tissue, frequently with recanalization) [15][1].4. Clinical Diagnosis
The clinical spectrum and outcome of CVT are related to different factors: location and number of thrombosed sinuses and cerebral veins, as well as the presence of functional collateral pathways, absence or presence of parenchymal lesions (cytotoxic or vasogenic edema, hemorrhage), gender, age, etiology, and interval from onset to admission to hospital [1][16][4,6]. The clinical presentation of CVT can be polymorphous, and misleading. In the majority of cases (50–80% of patients), the onset is subacute [15][17][1,52].4.1. Clinical Syndromes
In the majority of adult CVT cases, four major clinical syndromes have been noted in combination or isolation: Isolated intracranial hypertension, focal neurological deficits, seizures, and encephalopathy [15][18][1,2]. A minority of adult CVT patients develop a cavernous sinus thrombosis with a distinctive clinical picture: painful ophthalmoplegia. Collet-Siquard syndrome (consisting of multiple low cranial nerves palsies) represents a clinical syndrome of IJVs, posterior fossa veins, or LS thrombosis [15][18][1,2]. Rare adult CVT cases with unusual clinical aspects were also reported: subarachnoid hemorrhage, transient ischemic attacks, or psychiatric symptoms, mimicking a postpartum psychosis [15][18][1,2]. In neonates, CVT has a nonspecific clinical presentation with seizures, tetraparesis, and encephalopathy [10][17]. In older children, the clinical spectrum is more similar to the adult clinical aspects, with headache and paresis [19][53]. In elderly patients, symptoms of encephalopathy are more common than in adults, whereas isolated intracranial hypertension is less common [15][18][1,2].Isolated Intracranial Hypertension
It is the most frequent clinical syndrome observed in CVT (40% of cases) [1][6]. It consists of headaches, associated with vomiting, papilledema, visual complaints, and sixth nerve palsy [20][54]. It is more common in patients with a chronic onset than in those cases that present acutely [21][55]. Headache is the most common symptom of CVT (about 90% of cases in the ISCVT cohort). It is usually the initial one, and can develop isolated, or can precede other symptoms or signs. Headache is more frequent in women and younger patients than in men or older patients [4][6][17][19][7,13,52,53]. The characteristics of headaches are polymorphic. It may be localized or diffused [20][54]. Frequently, headache is severe augmenting during the night and may worsen with Valsalva maneuvers or position changes (when the patient is lying down) [18][22][2,32]. However, its characteristics can be misleading, sometimes being initially diagnosed as a migraine with aura [23][56]. In a few cases, it occurs like a thunderclap headache (mimicking a subarachnoid hemorrhage) [24][57]. Some of the risk factors associated with CVT (such as meningitis, epidural or brain abscesses, meningiomas, dural arteriovenous fistulas, and different vasculitis) also clinically manifest as a headache. CVT must be suspected as a possible explanation of persisting headache after lumbar puncture because this maneuver can rarely precipitate a CVT [15][1]. Headache is noted more frequently in patients with CVT than in cases with cerebral arterial infarcts [1][15][1,6]. Papilledema is observed on funduscopy in 25–40% of CVT cases, especially in those with chronic onset or delayed clinical presentation. It can produce transient loss of vision (associated with intense headache), and if prolonged, optic atrophy and consecutive peripheral blindness [1][3][6,12].Focal Neurological Deficits
They are noted in 37–50% of CVT patients and appear at onset in 15% of cases [6][15][1,7]. Paresis, sometimes bilateral, is the most frequent focal neurological deficit associated with CVT (in the ISCVT cohort was noted in 37% of cases) [6][15][1,7]. Other signs are less common: fluent aphasia (which is observed in left transverse sinus thrombosis associated with a posterior left temporal lesion), central sensory deficits, hemianopia, and ataxia (usually observed in posterior dural sinuses occlusion) [6][7]. Mixed transcortical aphasia is noted in left thalamus lesions due to deep cerebral vein thrombosis [25][58].Seizures
Focal or generalized seizures, even status epilepticus, are more frequently noted during the evolution of CVT (in the ICSVT cohort in 40% of cases) [6][7] than in arterial strokes [26][27][28][59,60,61]. Seizures appear during the onset of CVT in about 12–15% of cases [26][27][59,60]. A higher incidence has been observed in peripartum (76%) [27][60] and neonates (44%) [28][61]. Early seizures are noted more frequently in cases with supratentorial parenchymal brain lesions (especially disposed anterior to the sulcus of Rolando), thrombosis of the SSS and cortical veins and in those patients who present motor deficits [26][27][28][59,60,61].Encephalopathy
Subacute/chronic encephalopathy, presenting altered mental status with cognitive dysfunction (including delirium, apathy, and dysexecutive syndrome), and diminished level of consciousness (between drowsiness and deep coma) is frequently associated with multifocal neurological deficits and is observed especially in elderly patients or neonates with CVT [7][29][15,62]. Usually, the diminution of the level of consciousness is reversible; however, coma at onset represents the main predictor of a poor outcome [15][18][1,2].4.2. Topographic Clinical Diagnosis
Due to frequent concomitant multiple cerebral veins and dural sinuses thrombosis (more than two-thirds of cases), the existence of multiple anatomic variants of some cerebral veins and dural sinuses, and action of venous collateral circulation, the topographic clinical diagnosis of CVT is not so well-defined like in arterial occlusion and frequent is misleading [6][15][30][1,7,63]. However, isolated thrombosis of the different dural sinuses and cerebral veins produces the following clinical aspects (Figure 21).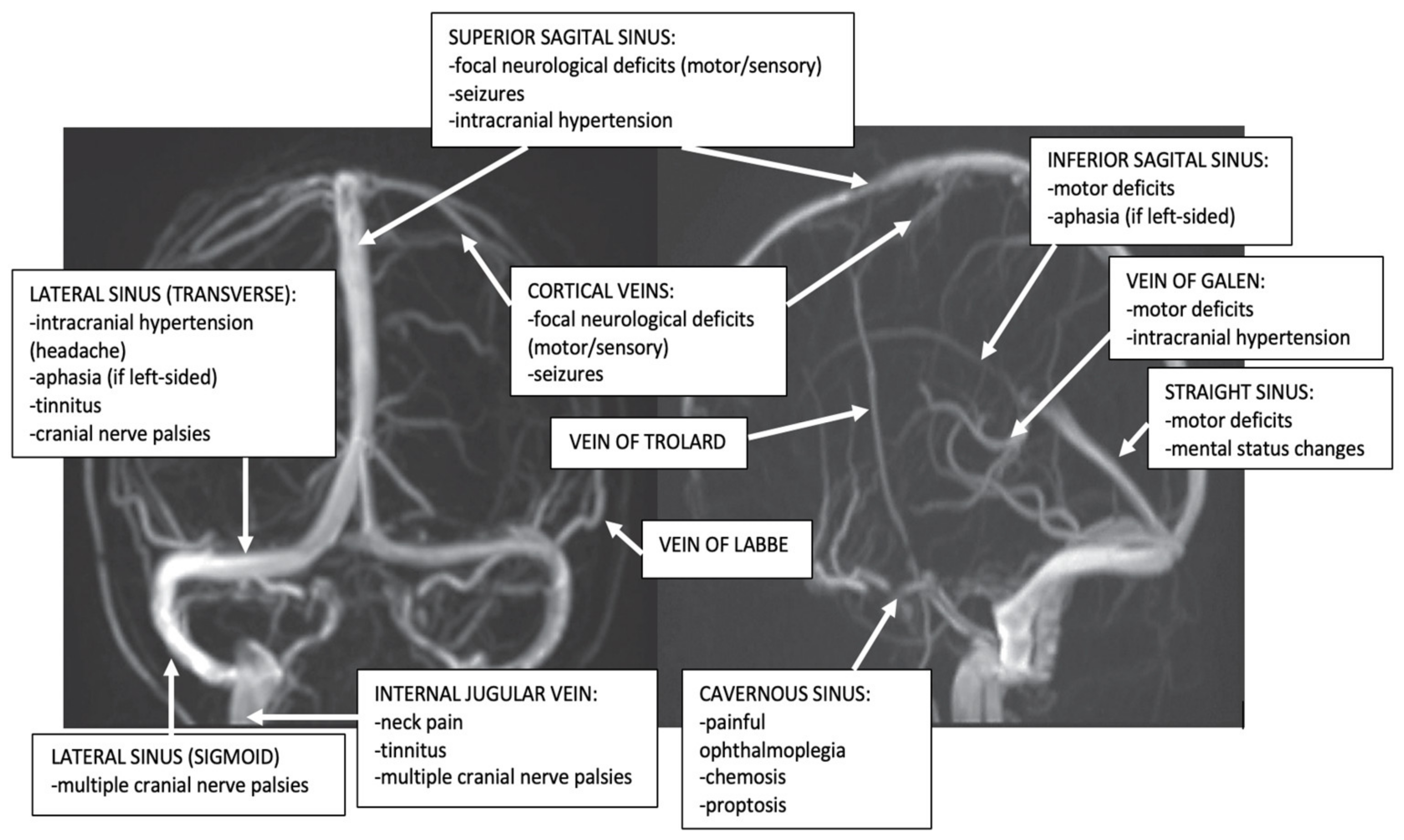
Figure 2. Dural sinuses and cerebral veins anatomy and major clinical syndromes according to the topography of CVT (archive of the First Department of Neurology, Clinical Emergency County Hospital, Timisoara, Romania).
