In percutaneous pedicle screw (PPS) fixation of the osteoporotic spine, rigid screw fixation obtaining strong stabilization is important for achieving successful treatment outcomes. However, in patients with severe osteoporosis, it is difficult to obtain PPS fixation with sufficient stability. PPS fixation has potential disadvantages with respect to maintaining secure stabilization in comparison to conventional pedicle screw fixation. In PPS fixation, bone grafting to achieve posterior spine fusion is generally not applicable and transverse connectors between the rods cannot be used to reinforce the fixation. Various augmentation methods, including additional hooks, sublaminar bands, and hydroxyapatite (HA) sticks, are available for conventional pedicle screw fixation.
- percutaneous pedicle screw
- hydroxyapatite granules
- augmentation
- osteoporosis
- spine
1. Introduction
2. Surgical Procedure of Augmentation of PPS Fixation Using HA Granules
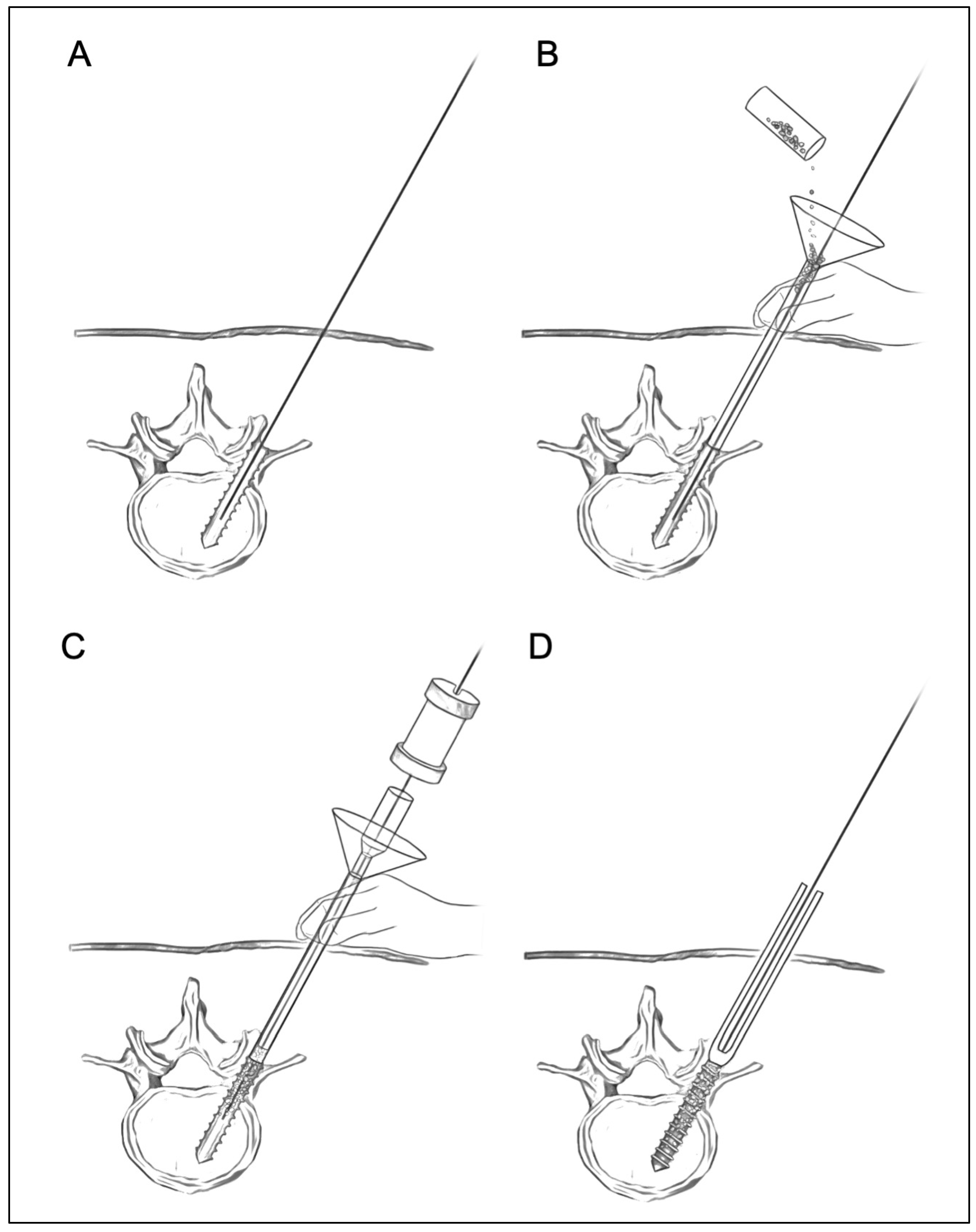
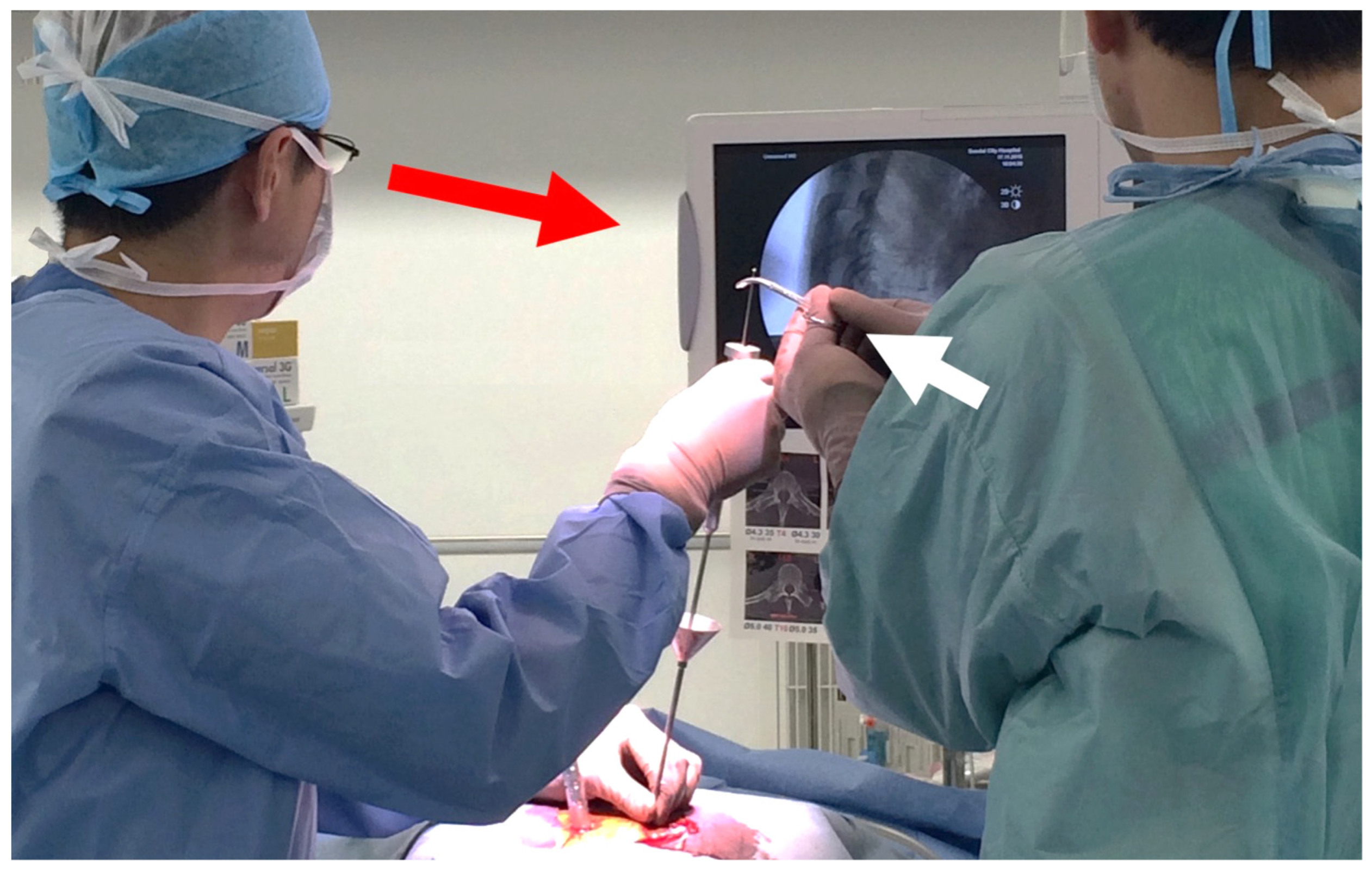
In ourthe augmentation technique for PPS fixation, HA granules can be inserted percutaneously into the screw hole along the guidewire using a dedicated inserter (Figure 1). This method has the advantage that PPS fixation can be enhanced percutaneously without compromising the minimally invasive procedure. WResearchers use commercially available HA granules (porosity, 50%; particle size, 1.0–2.0 mm; Apaceram, HOYA Technosurgical Corp., Tokyo, Japan) for the augmentation (Figure 1A) [22,23][22][23]. Based on the results of biomechanical analyses in ourthe previous studies [22[22][23],23], at least 0.25 g of HA granules are used for the augmentation for each PPS. WThey created a dedicated device to insert the HA granules percutaneously into the screw hole in order to achieve the augmentation (Figure 1B) [14].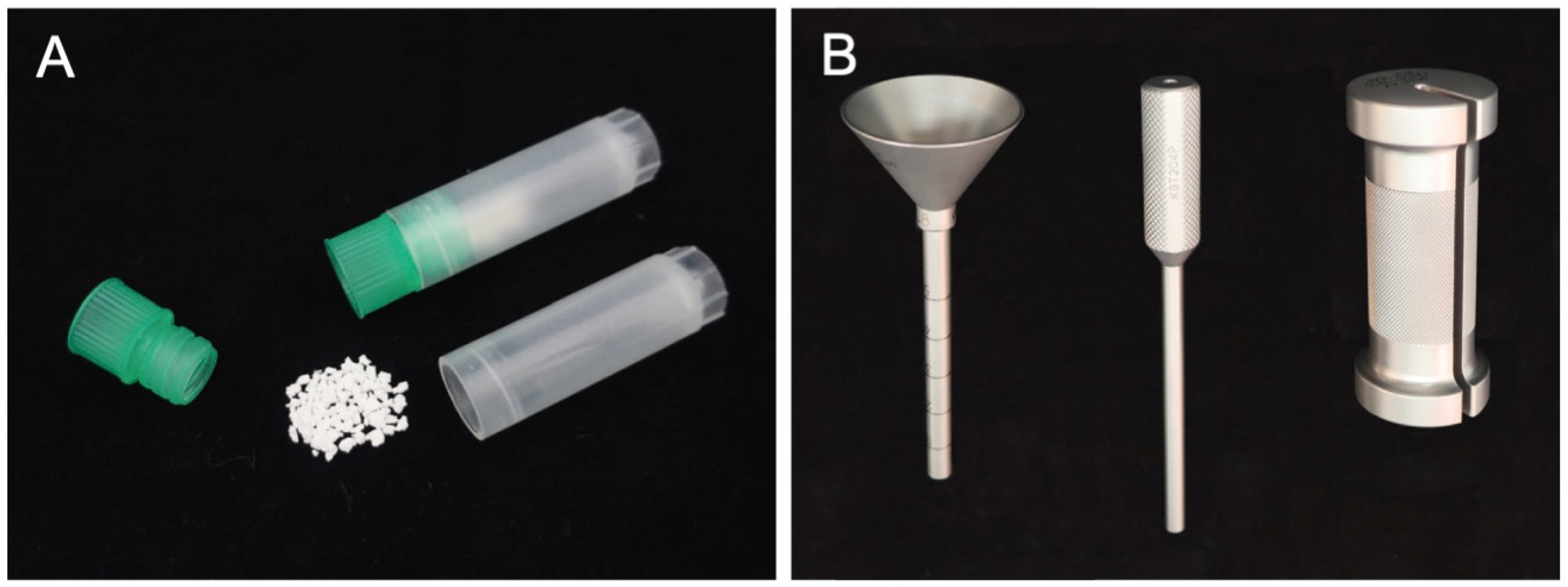
3. Biomechanical Analysis of Augmentation of PPS Fixation Using HA Granules
Previous studies indicated that the placement of substances into the tapped screw hole increases the bone–metal interface friction force and enhances the mechanical strength of screw fixation [16,26,27,28,29,30,31][16][26][27][28][29][30][31]. WResearchers previously performed a biomechanical analysis to evaluate the strength and stiffness of PPS fixation augmented with HA granules using a synthetic bone model [22]. The results of that study demonstrated the biomechanical advantages of augmentation with HA granules for PPS fixation in the osteoporotic bone model. The study showed that the maximal insertion torque and the maximal pullout strength were significantly increased in screws with augmentation in comparison to without augmentation. Furthermore, the mechanical strength against cyclic loading was significantly greater in screws with augmentation in comparison to those without augmentation. In another study, wresearchers performed a cadaveric biomechanical analysis of PPS fixation augmented with HA granules [23]. The biomechanical performance in augmenting PPS fixation was evaluated using osteoporotic lumbar vertebrae obtained from cadavers. OurThe results demonstrated that the augmentation using HA granules significantly increased the maximal pullout strength and maximal insertion torque of the screws placed in the osteoporotic lumbar spine. Moreover, a cyclic loading test revealed that the augmented screws achieved significantly higher mechanical strength. These findings suggest that PPS fixation can be enhanced by augmentation with HA granules in the osteoporotic lumbar spine. PPS fixation augmented with HA granules may be helpful for decreasing the incidence of screw loosening and implant failure in patients with osteoporotic spine.References
- Mobbs, R.J.; Park, A.; Maharaj, M.; Phan, K. Outcomes of percutaneous pedicle screw fixation for spinal trauma and tumours. J. Clin. Neurosci. 2016, 23, 88–94.
- Zhang, W.; Li, H.; Zhou, Y.; Wang, J.; Chu, T.; Zheng, W.; Chen, B.; Li, C. Minimally Invasive Posterior Decompression Combined with Percutaneous Pedicle Screw Fixation for the Treatment of Thoracolumbar Fractures with Neurological Deficits. Spine 2016, 41, B23–B29.
- Regev, G.J.; Lee, Y.P.; Taylor, W.R.; Garfin, S.R.; Kim, C.W. Nerve injury to the posterior rami medial branch during the insertion of pedicle screws: Comparison of mini-open versus percutaneous pedicle screw insertion techniques. Spine 2009, 34, 1239–1242.
- Gu, G.; Zhang, H.; He, S.; Cai, X.; Gu, X.; Jia, J.; Fu, Q.; Zhou, X. Percutaneous Pedicle Screw Placement in the Lumbar Spine: A Comparison Study between the Novel Guidance System and the Conventional Fluoroscopy Method. J. Spinal Disord. Tech. 2015, 28, E522–E527.
- Burge, R.; Dawson-Hughes, B.; Solomon, D.H.; Wong, J.B.; King, A.; Tosteson, A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J. Bone Miner Res. 2007, 22, 465–475.
- Melton, L.J. Epidemiology of spinal osteoporosis. Spine 1997, 22, 2S–11S.
- Okuyama, K.; Abe, E.; Suzuki, T.; Tamura, Y.; Chiba, M.; Sato, K. Can insertional torque predict screw loosening and related failures? An in vivo study of pedicle screw fixation augmenting posterior lumbar interbody fusion. Spine 2000, 25, 858–864.
- Okuyama, K.; Abe, E.; Suzuki, T.; Tamura, Y.; Chiba, M.; Sato, K. Influence of bone mineral density on pedicle screw fixation: A study of pedicle screw fixation augmenting posterior lumbar interbody fusion in elderly patients. Spine J. 2001, 1, 402–407.
- Murakami, H.; Tsai, K.-J.; Attallah-Wasif, E.S.; Yamazaki, K.; Shimamura, T.; Hutton, W.C. A biomechanical assessment of infra-laminar hooks as an alternative to supra-laminar hooks in thoracolumbar fixation. Spine 2006, 31, 967–971.
- Hongo, M.; Gay, R.E.; Zhao, K.D.; Ilharreborde, B.; Huddleston, P.M.; Berglund, L.J.; An, K.-N.; Zhao, C. Junction kinematics between proximal mobile and distal fused lumbar segments: Biomechanical analysis of pedicle and hook constructs. Spine J. 2009, 9, 846–853.
- Hasegawa, K.; Takahashi, H.E.; Uchiyama, S.; Hirano, T.; Hara, T.; Washio, T.; Sugiura, T.; Youkaichiya, M.; Ikeda, M. An experimental study of a combination method using a pedicle screw and laminar hook for the osteoporotic spine. Spine 1997, 22, 958–963.
- Hamasaki, T.; Tanaka, N.; Kim, J.; Okada, M.; Ochi, M.; Hutton, W.C. Pedicle screw augmentation with polyethylene tape: A biomechanical study in the osteoporotic thoracolumbar spine. J. Spinal Disord. Tech. 2010, 23, 127–132.
- Hongo, M.; Ilharreborde, B.; Gay, R.E.; Zhao, C.; Zhao, K.D.; Berglund, L.J.; Zobitz, M.; An, K.-N. Biomechanical evaluation of a new fixation device for the thoracic spine. Eur. Spine J. 2009, 18, 1213–1219.
- Burval, D.J.; McLain, R.F.; Milks, R.; İnceoğlu, S. Primary Pedicle Screw Augmentation in Osteoporotic Lumbar Vertebrae. Spine 2007, 32, 1077–1083.
- Becker, S.; Chavanne, A.; Spitaler, R.; Kropik, K.; Aigner, N.; Ogon, M.; Redl, H. Assessment of different screw augmentation techniques and screw designs in osteoporotic spines. Eur. Spine J. 2008, 17, 1462–1469.
- Matsuzaki, H.; Tokuhashi, Y.; Wakabayashi, K.; Okawa, A.; Hagiwara, H.; Iwahashi, M. Effects of hydroxyapatite solid granule (HA Stick) on pedicle screwing for osteoporotic patients. Clin. Orthop. Surg. 2001, 36, 529–534. (In Japanese)
- Shin, S.J.; Lee, J.H.; Lee, J.H. Influence of Hydroxyapatite Stick on Pedicle Screw Fixation in Degenerative Lumbar Spine: Biomechanical and Radiologic Study. Clin. Spine Surg. 2017, 30, E819–E826.
- Foley, K.T.; Holly, L.T.; Schwender, J.D. Minimally invasive lumbar fusion. Spine 2003, 28, S26–S35.
- Foley, K.T.; Gupta, S.K.; Justis, J.R.; Sherman, M.C. Percutaneous pedicle screw fixation of the lumbar spine. Neurosurg. Focus 2001, 10, E10.
- Kuklo, T.R.; Dmitriev, A.E.; Cardoso, M.J.; Lehman, R.A.; Erickson, M.; Gill, N.W. Biomechanical contribution of transverse connectors to segmental stability following long segment instrumentation with thoracic pedicle screws. Spine 2008, 33, E482–E487.
- Chutkan, N.B.; Zhou, H.; Akins, J.P.; Wenger, K.H. Effects of facetectomy and crosslink augmentation on motion segment flexibility in posterior lumbar interbody fusion. Spine 2008, 33, E828–E835.
- Kanno, H.; Aizawa, T.; Hashimoto, K.; Itoi, E. Enhancing percutaneous pedicle screw fixation with hydroxyapatite granules: A biomechanical study using an osteoporotic bone model. PLoS ONE 2019, 14, e0223106.
- Kanno, H.; Aizawa, T.; Hashimoto, K.; Itoi, E. Novel augmentation technique of percutaneous pedicle screw fixation using hydroxyapatite granules in the osteoporotic lumbar spine: A cadaveric biomechanical analysis. Eur. Spine J. 2021, 30, 71–78.
- Kanno, H. Augmentation of percutaneous pedicle screw fixation: Novel method using hydroxyapatite granules and effectiveness of teriparatide. J. MIOS 2018, 87, 81–88.
- Kanno, H.; Murotani, M.; Aizawa, T.; Ozawa, H. Reinforcement of percutaneous pedicle screw fixation using hydroxyapatite granules: Prevention of postoperative screw loosening. In Proceedings of the 11th Annual Meeting of Society for Minimally Invasive Spinal Treatment, Tokyo, Japan, 29–30 October 2021; p. 87.
- Yi, S.; Rim, D.C.; Park, S.W.; Murovic, J.A.; Lim, J.; Park, J. Biomechanical Comparisons of Pull out Strengths after Pedicle Screw Augmentation with Hydroxyapatite, Calcium Phosphate, or Polymethylmethacrylate in the Cadaveric Spine. World Neurosurg. 2015, 83, 976–981.
- Spivak, J.M.; Neuwirth, M.G.; Labiak, J.J.; Kummer, F.J.; Ricci, J.L. Hydroxyapatite enhancement of posterior spinal instrumentation fixation. Spine 1994, 19, 955–964.
- Hasegawa, K.; Yamamura, S.; Dohmae, Y. Enhancing screw stability in osteosynthesis with hydroxyapatite granules. Arch. Orthop. Trauma Surg. 1998, 117, 175–176.
- Yerby, S.A.; Toh, E.; McLain, R.F. Revision of failed pedicle screws using hydroxyapatite cement. A biomechanical analysis. Spine 1998, 23, 1657–1661.
- Lotz, J.C.; Hu, S.S.; Chiu, D.F.; Yu, M.; Colliou, O.; Poser, R.D. Carbonated apatite cement augmentation of pedicle screw fixation in the lumbar spine. Spine 1997, 22, 2716–2723.
- Spivak, J.M.; Hasharoni, A. Use of hydroxyapatite in spine surgery. Eur. Spine J. 2001, 10 (Suppl. 2), S197–S204.
