Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Rod Moore and Version 2 by Camila Xu.
Effective communication skills, that is, accurate listening or observation and focused verbal or non-verbal response, enhances efficiency of diagnoses, ethical clinical decision making, positive clinical outcomes, promotes patient use of services, and patient–clinician satisfaction. It also helps to decrease patient anxiety and pain perception.
- active listening
- communication skills
- dental education
- empathy
1. Introduction
Effective communication skills, that is, accurate listening or observation and focused verbal or non-verbal response, enhances efficiency of diagnoses, ethical clinical decision making, positive clinical outcomes, promotes patient use of services, and patient–clinician satisfaction [1][2][3]. It also helps to decrease patient anxiety and pain perception [4]. Conversely, poor communication is the most common reason for dissatisfaction with care, promotion of distrust, including malpractice [5], and is the most common cause for termination of the relationship [6].
Effective communication skills, that is, accurate listening or observation and focused verbal or non-verbal response, enhances efficiency of diagnoses, ethical clinical decision making, positive clinical outcomes, promotes patient use of services, and patient–clinician satisfaction [1,2,3]. It also helps to decrease patient anxiety and pain perception [4]. Conversely, poor communication is the most common reason for dissatisfaction with care, promotion of distrust, including malpractice [5], and is the most common cause for termination of the relationship [6].
Most of the literature about student learning of clinical communication skills appears in allied health, especially for medical and nursing students. This literature is vast compared with similar dental educational literature [7][8]. The role of the dentist or dental student and the context of interactions with patients reveals some very special conditions, such as supine dental chair position and that the patient’s mouth is often occupied. These among others, make this role unique among health care workers. Moreover, unlike modern medical care situations, the patient role is most often passive and the relationship is dentist dominated [9][10]. For this reason, it is important not to extrapolate allied health findings and draw conclusions for dental student communication skills learning. Furthermore, given this persistent dentist-dominated relationship over time, many educators emphasize the need for dental students to increase practical learning in active listening and patient-centered skills [8][9][10][11]. Patient-centered communication has shown several advantages in the medical literature, including improved patient recall, compliance and satisfaction [11]. Research on advantages of patient-centered communication in dentistry is scant in comparison, but includes decreased patient dental anxiety [4][12], decreased perceived operative pain [4] as well as improved oral hygiene and periodontal compliance [13][14].
Most of the literature about student learning of clinical communication skills appears in allied health, especially for medical and nursing students. This literature is vast compared with similar dental educational literature [7,8]. The role of the dentist or dental student and the context of interactions with patients reveals some very special conditions, such as supine dental chair position and that the patient’s mouth is often occupied. These among others, make this role unique among health care workers. Moreover, unlike modern medical care situations, the patient role is most often passive and the relationship is dentist dominated [9,10]. For this reason, it is important not to extrapolate allied health findings and draw conclusions for dental student communication skills learning. Furthermore, given this persistent dentist-dominated relationship over time, many educators emphasize the need for dental students to increase practical learning in active listening and patient-centered skills [8,9,10,11]. Patient-centered communication has shown several advantages in the medical literature, including improved patient recall, compliance and satisfaction [11]. Research on advantages of patient-centered communication in dentistry is scant in comparison, but includes decreased patient dental anxiety [4,12], decreased perceived operative pain [4] as well as improved oral hygiene and periodontal compliance [13,14].
Finally, dental communication skills have traditionally been taught as one time didactic coursework, with little or no practical components prior to 2010 [7]. Although this has changed considerably, some dental education experts [7][15][16] have called for more longitudinal teaching that would follow students’ clinical development through the course of the dental curriculum.
Finally, dental communication skills have traditionally been taught as one time didactic coursework, with little or no practical components prior to 2010 [7]. Although this has changed considerably, some dental education experts [7,15,16] have called for more longitudinal teaching that would follow students’ clinical development through the course of the dental curriculum.
2. Special Characteristics about the Dental Clinic and Communication
Sociolinguists Coleman and Burton [17] originally pointed out that there is considerable difference between dental and medical consultations in that the latter are hands-on treatment sessions only in exceptional cases. This has also been echoed recently in the dental literature [13][18][19]. The functions of the physician in a typical consultation are to investigate symptoms and patient perceptions, aid diagnosis, prescribe treatment, review progress and give information and advice. The structure as described by sociolinguist Long and others [19][20] is a sequence of phases, which closely resemble other decision-making schemes in other disciplines: (1) greeting the patient; (2) discovering the patient’s reasons for attending; (3) conducting a physical or verbal examination (or both); (4) sharing information with the patient; (5) detailing further courses of action (i.e., prescription of drugs or referral); and (6) closing the consultation. More recently, it has evolved towards patient-centered communication and is called the “six-functions model” as reviewed by King and Hoppe [11]: (1) fostering the relationship, (2) gathering information, (3) providing information, (4) making decisions, (5) responding to emotions, and (6) enabling disease- and treatment-related behavior in closure. The emphasis upon one phase or another varies from case to case, often requiring more work on building rapport in a relationship throughout the consultation. An initial consultation with the dentist also has all of these functions. On the other hand, one crucial difference is that there is actual administration of hands-on dental treatment in nearly all phases of dentist–patient interaction, including initial consultations [13][17][18][19]. Patient-centered interactions requiring response to emotions force dentists to also take into account patients’ perceived feelings of need for control during treatment in the dental chair, among other things [19]. Thus, in a dental private practice setting, only initial contact with a new patient for the first time truly resembles a medical consultation, unless there are special circumstances for follow-up consultations due to anxiety or special care needs. In a 2010 systematic review of dental communication skills training, Carey et al. [7] pointed out the necessity for communications skills learning to be extended to include intra-operative communication, rather than solely based on learning skills for initial consultations with patients. Since most communication occurs during actual treatment phases, rather than in initial consultations, it seems logical that dental students should be prepared for both. Furthermore, all dental patients are recalled for periodical check-ups and preventive treatments, unlike most medical patients. This also affects the context of dentist–patient communication compared with the context of medical consultations. In a 2019 major systematic review of communication coursework in dental education, Khalifah and Celenza [8] also point out the necessity for communication skills to be extended to include intra-operative communication, concurring with Carey et al.’s findings. They also go on to study dental communication skill categories and other essential components of dental student learning.3. Essential Components of Dental Student Learning of Communication Skills
Khalifah and Celenza [8] identified 26 communication skills that fell under four categories as listed below (see2. Special Characteristics about the Dental Clinic and Communication
Sociolinguists Coleman and Burton [18] originally pointed out that there is considerable difference between dental and medical consultations in that the latter are hands-on treatment sessions only in exceptional cases. This has also been echoed recently in the dental literature [13,19,20]. The functions of the physician in a typical consultation are to investigate symptoms and patient perceptions, aid diagnosis, prescribe treatment, review progress and give information and advice. The structure as described by sociolinguist Long and others [20,21] is a sequence of phases, which closely resemble other decision-making schemes in other disciplines: (1) greeting the patient; (2) discovering the patient’s reasons for attending; (3) conducting a physical or verbal examination (or both); (4) sharing information with the patient; (5) detailing further courses of action (i.e., prescription of drugs or referral); and (6) closing the consultation. More recently, it has evolved towards patient-centered communication and is called the “six-functions model” as reviewed by King and Hoppe [11]: (1) fostering the relationship, (2) gathering information, (3) providing information, (4) making decisions, (5) responding to emotions, and (6) enabling disease- and treatment-related behavior in closure. The emphasis upon one phase or another varies from case to case, often requiring more work on building rapport in a relationship throughout the consultation. An initial consultation with the dentist also has all of these functions.
On the other hand, one crucial difference is that there is actual administration of hands-on dental treatment in nearly all phases of dentist–patient interaction, including initial consultations [13,18,19,20]. Patient-centered interactions requiring response to emotions force dentists to also take into account patients’ perceived feelings of need for control during treatment in the dental chair, among other things [20]. Thus, in a dental private practice setting, only initial contact with a new patient for the first time truly resembles a medical consultation, unless there are special circumstances for follow-up consultations due to anxiety or special care needs. In a 2010 systematic review of dental communication skills training, Carey et al. [7] pointed out the necessity for communications skills learning to be extended to include intra-operative communication, rather than solely based on learning skills for initial consultations with patients. Since most communication occurs during actual treatment phases, rather than in initial consultations, it seems logical that dental students should be prepared for both.
Furthermore, all dental patients are recalled for periodical check-ups and preventive treatments, unlike most medical patients. This also affects the context of dentist–patient communication compared with the context of medical consultations. In a 2019 major systematic review of communication coursework in dental education, Khalifah and Celenza [8] also point out the necessity for communication skills to be extended to include intra-operative communication, concurring with Carey et al.’s findings. They also go on to study dental communication skill categories and other essential components of dental student learning.
3. Essential Components of Dental Student Learning of Communication Skills
Khalifah and Celenza [8] identified 26 communication skills that fell under four categories as listed below (see
Figure 1 for details).
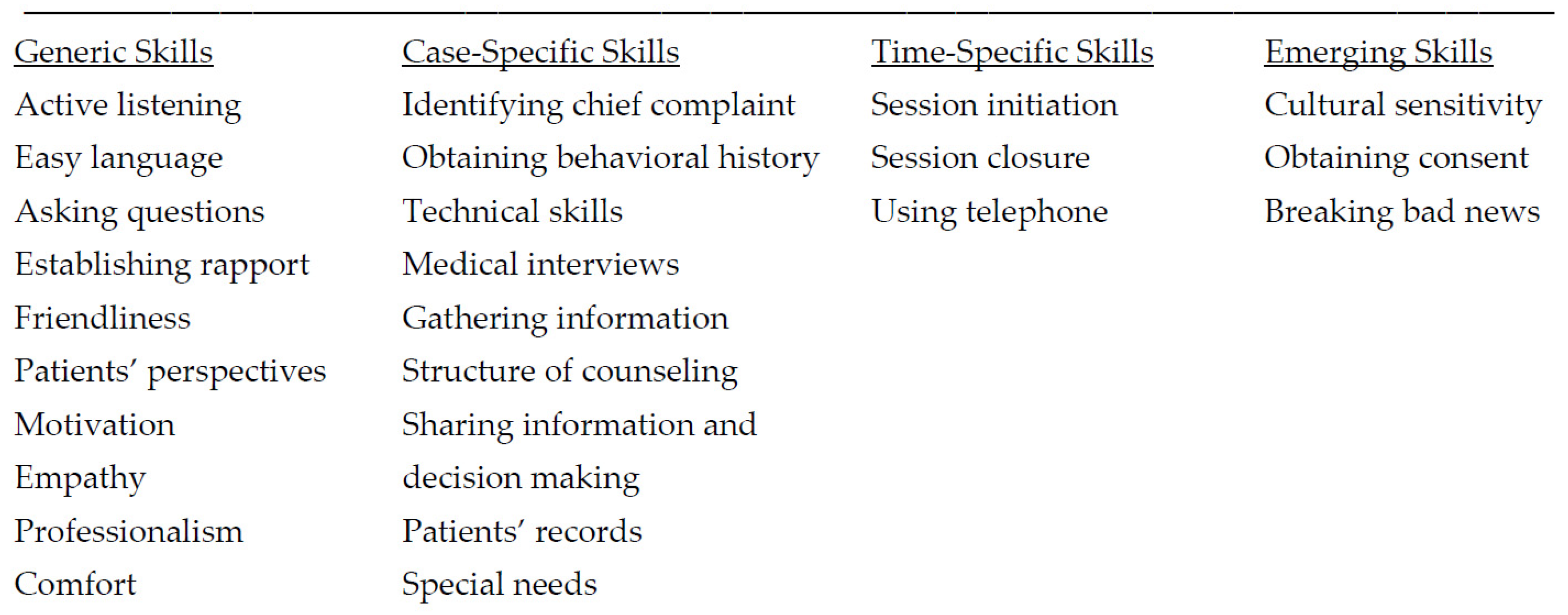
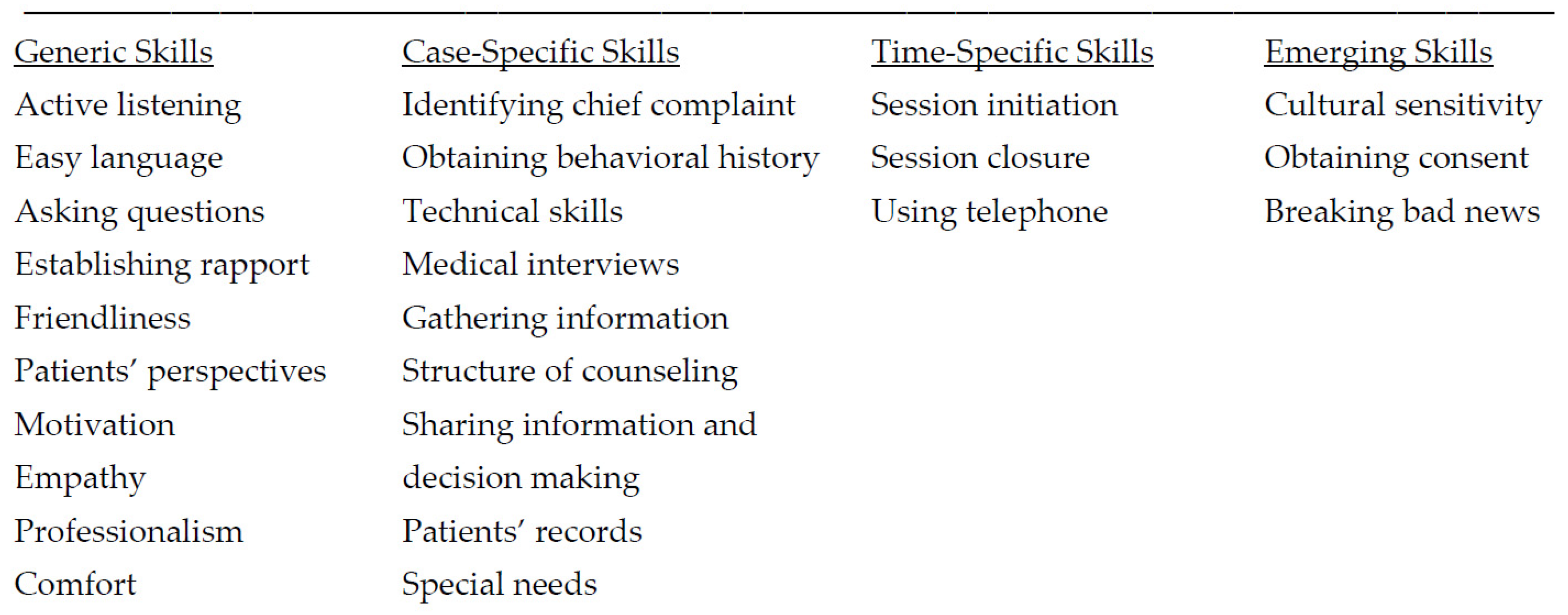
for details).
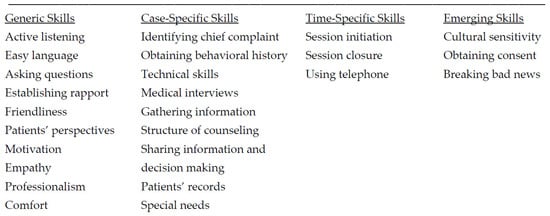
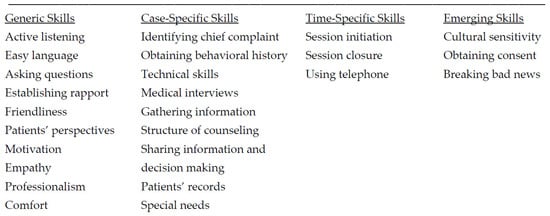
Figure 1. Twenty-six communication skills in four categories adapted from Khalifah and Celenza [8]. Generic skills are those to be used at any dental visit and must become natural habits of the dentist. Case-specific skills regard individual cases and situations and vary according to patient and case. Time-specific skills are appropriate at certain times in a consultation. Emerging skills are skills to be applied in distinctive cases with special considerations.
Khalifah and Celenza also tabled each of the 50 relevant studies for type of communication skills taught, teaching method (e.g., role-play, video supervision, lectures) and assessment method and outcomes [8]. From these, researchers obtain a picture of the specific contexts for learning communication skills in dentistry and being able to rate them according to quality. In common with most of the articles reviewed and tabled by Khalifah and Celenza, “active listening”, gathering information, establishing rapport, empathy, professionalism and motivation were predominant [8]. According to Khalifah and Celenza [8], the highest quality studies put the patient’s perspective at the center of communications, no matter how short or long the duration of consultation or needs within the context described.
Patient-Centered Care—Active Listening and Empathy
People tend to overestimate their listening comprehension, suggesting that they may not perceive listening as a skill requiring development in the same way that speaking, reading, writing or manual techniques are skills acquired through instruction, effort and time [21]. Active listening is the major skill promoted in patient-centered communication [8][22][23][24][25][26]. Active listening was initially promoted among others, by psychologist Carl Rogers [26][27]. Rogers argued that active listening was the most effective way to explore and understand a patient’s problems and help them as well. A normal first reaction of most people in thinking about listening as a possible therapy for dealing with human problems is that listening is thought of as passive and insufficient. They think that listening does not communicate anything to the speaker. However, by consistently listening and verifying what one hears with a speaker, the listener is conveying the idea: “I’m interested in you and I think that what you have to say is important. I respect your thoughts, and (even if I may not agree with them), I know that they are valid for you. I’m not trying to change you or evaluate you. I just want to understand you.” Active listening promotes empathy with the speaker, which promotes positive outcomes [11][23]. Active listening involves learning to work with both non-verbal as well as verbal communication in order to “mirror” for a patient, that is, to verify meaning by summarizing and reformulating statements for clearer mutual understanding. Active listening is a “healthy combination” of critical listening, reflective listening and passive listening. Active listeners are critical in trying to interpret a message and evaluate the speaker’s emotions and non-verbal cues; reflective listening helps the speaker to “feel heard”; and silence and pauses in passive listening signals to the speaker that there is uninterrupted time for them to communicate their message [28]. Active listening is used both in initial consultations and during communications in active dental treatment. Adapting active listening as a central element in a communication skills curriculum is not only essential to optimizing one-on-one communication between the student dentist and patients, but it also signals a philosophical change from doctor-centered to patient-centered consultations and treatment [11][15]. Patient-centered care (PCC) has grown out of observations that active listening and empathy maximize clinical communication and health outcomes and was first officially espoused by the Institute of Medicine in 2001 [11]. King and Hoppe’s 2013 extensive review of patient-centered care indicated a consensus about what constitutes ‘‘best practice’’ for communication in clinical encounters, the so-called “six-functions model” described above, which basically pervades all consultation models and styles that will be described below. King and Hoppe [11] surmised that there was abundant evidence in the medical literature supporting the importance of patient-centered communication skills as a dimension of physician competence. They cited evidence of positive outcomes about patient recall, understanding, satisfaction and adherence to therapy [11]. King and Hoppe stated that “efforts to enhance teaching of communication skills to medical trainees would likely require significant changes in instruction at undergraduate and graduate levels, as well as changes in assessing the developing communication skills of physicians.” An added critical dimension is faculty understanding of the importance of communication skills, and their commitment to helping trainees develop those skills [11]. In a systematic review of PCC in dentistry, Scambler et al., [10] concluded it is about delivering humane care involving good communication and shared decision-making. However, they noted there was no evidence in the dental literature suggesting that the concept is either clearly understood or empirically and systematically assessed in dental settings. They presented a model of four levels of information and choice provision and/or agreement between dentist and patient. Level 1 is one-way information from the dentist. Level 2 is when patient makes informed choice among informed treatment options. Level 3 is when patients are given tools to make the choice themselves, under advisement. Finally, Level 4 is when the patient is in full control of their care and capable of making informed choices they wish or do not wish to achieve. The model does not assume that all patients would want, or be happy with a Level 4 approach, that is, may not be their hierarchical endpoint. Another systematic review by Mills et al. [9] revealed a lack of understanding of PCC in dentistry, and in particular, general dental practice. Mills et al. [10] pointed to a poor evidence base and no support for the use of then current patient reported outcome measures as indicators of patient-centeredness. However, Mills et al. did find that special dentistry qualitative research about treatment of phobic and economically disadvantaged patients provided some evidence of good outcomes using patient-centered communication for these vulnerable populations. In summary, unlike the medical literature, the dental literature on patient-centered care and communication is scant. This possibly reflects values of dental education and of the profession as a whole in the reluctance to adopt what has proven to be in the medical profession and in society in general, a developmental paradigm shift. Twenty-six communication skills in four categories adapted from Khalifah and Celenza [8]. Generic skills are those to be used at any dental visit and must become natural habits of the dentist. Case-specific skills regard individual cases and situations and vary according to patient and case. Time-specific skills are appropriate at certain times in a consultation. Emerging skills are skills to be applied in distinctive cases with special considerations.
Khalifah and Celenza also tabled each of the 50 relevant studies for type of communication skills taught, teaching method (e.g., role-play, video supervision, lectures) and assessment method and outcomes [8]. From these, we obtain a picture of the specific contexts for learning communication skills in dentistry and being able to rate them according to quality. In common with most of the articles reviewed and tabled by Khalifah and Celenza, “active listening”, gathering information, establishing rapport, empathy, professionalism and motivation were predominant [8]. According to Khalifah and Celenza [8], the highest quality studies put the patient’s perspective at the center of communications, no matter how short or long the duration of consultation or needs within the context described.
Patient-Centered Care—Active Listening and Empathy
People tend to overestimate their listening comprehension, suggesting that they may not perceive listening as a skill requiring development in the same way that speaking, reading, writing or manual techniques are skills acquired through instruction, effort and time [22]. Active listening is the major skill promoted in patient-centered communication [8,23,24,25,26,27]. Active listening was initially promoted among others, by psychologist Carl Rogers [27,28]. Rogers argued that active listening was the most effective way to explore and understand a patient’s problems and help them as well. A normal first reaction of most people in thinking about listening as a possible therapy for dealing with human problems is that listening is thought of as passive and insufficient. They think that listening does not communicate anything to the speaker. However, by consistently listening and verifying what one hears with a speaker, the listener is conveying the idea: “I’m interested in you and I think that what you have to say is important. I respect your thoughts, and (even if I may not agree with them), I know that they are valid for you. I’m not trying to change you or evaluate you. I just want to understand you.” Active listening promotes empathy with the speaker, which promotes positive outcomes [11,24]. Active listening involves learning to work with both non-verbal as well as verbal communication in order to “mirror” for a patient, that is, to verify meaning by summarizing and reformulating statements for clearer mutual understanding. Active listening is a “healthy combination” of critical listening, reflective listening and passive listening. Active listeners are critical in trying to interpret a message and evaluate the speaker’s emotions and non-verbal cues; reflective listening helps the speaker to “feel heard”; and silence and pauses in passive listening signals to the speaker that there is uninterrupted time for them to communicate their message [29]. Active listening is used both in initial consultations and during communications in active dental treatment. Adapting active listening as a central element in a communication skills curriculum is not only essential to optimizing one-on-one communication between the student dentist and patients, but it also signals a philosophical change from doctor-centered to patient-centered consultations and treatment [11,15].
Patient-centered care (PCC) has grown out of observations that active listening and empathy maximize clinical communication and health outcomes and was first officially espoused by the Institute of Medicine in 2001 [11]. King and Hoppe’s 2013 extensive review of patient-centered care indicated a consensus about what constitutes ‘‘best practice’’ for communication in clinical encounters, the so-called “six-functions model” described above, which basically pervades all consultation models and styles that will be described below. King and Hoppe [11] surmised that there was abundant evidence in the medical literature supporting the importance of patient-centered communication skills as a dimension of physician competence. They cited evidence of positive outcomes about patient recall, understanding, satisfaction and adherence to therapy [11]. King and Hoppe stated that “efforts to enhance teaching of communication skills to medical trainees would likely require significant changes in instruction at undergraduate and graduate levels, as well as changes in assessing the developing communication skills of physicians.” An added critical dimension is faculty understanding of the importance of communication skills, and their commitment to helping trainees develop those skills [11].
In a systematic review of PCC in dentistry, Scambler et al., [10] concluded it is about delivering humane care involving good communication and shared decision-making. However, they noted there was no evidence in the dental literature suggesting that the concept is either clearly understood or empirically and systematically assessed in dental settings. They presented a model of four levels of information and choice provision and/or agreement between dentist and patient. Level 1 is one-way information from the dentist. Level 2 is when patient makes informed choice among informed treatment options. Level 3 is when patients are given tools to make the choice themselves, under advisement. Finally, Level 4 is when the patient is in full control of their care and capable of making informed choices they wish or do not wish to achieve.
The model does not assume that all patients would want, or be happy with a Level 4 approach, that is, may not be their hierarchical endpoint.
Another systematic review by Mills et al. [9] revealed a lack of understanding of PCC in dentistry, and in particular, general dental practice. Mills et al. [10] pointed to a poor evidence base and no support for the use of then current patient reported outcome measures as indicators of patient-centeredness. However, Mills et al. did find that special dentistry qualitative research about treatment of phobic and economically disadvantaged patients provided some evidence of good outcomes using patient-centered communication for these vulnerable populations.
In summary, unlike the medical literature, the dental literature on patient-centered care and communication is scant. This possibly reflects values of dental education and of the profession as a whole in the reluctance to adopt what has proven to be in the medical profession and in society in general, a developmental paradigm shift.
