Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Rita Xu and Version 3 by Rita Xu.
In recent years, there has been more and more talk of cyber health psychology and the implication that new technologies can have in the diagnosis, treatment, and rehabilitation of psychopathological issues in the field of mental health, ranging from post-traumatic stress disorder (PTSD) to addiction to substances of abuse.
- cyber health psychology
- Virtual Reality
- mHealth
- mCessation
- smartphone applications
1. Introduction
Among the most used technological tools is Virtual Reality (VR), an immersive experience of contextual simulation in which the subject wears a head-mounted display (HMD) and orients themselves in a three-dimensional space that has been virtually developed. It is also possible to actively interact with the environment through inputs transmitted with a controller or keyboard or, with the latest Virtual Reality models, through gloves with sensors or motion detection techniques [1]. Virtual Reality is used, for instance, in the treatment of head trauma [2] and Parkinson’s disorder [3]. It has also been used in psychotherapies with patients suffering from schizophrenic spectrum disorder, with promising results [1].
Moving to the side of mobile technologies, the use of Mobile Health (mHealth) is steadily increasing. mHealth is a relatively new area of healthcare; in its 2011 report, the World Health Organization defines it as “the use of mobile and wireless technologies to support the achievement of health goals; it has the potential to transform the face of healthcare provision around the world” [4]. Although mHealth does not have a standard definition, it is considered a medical and public health practice supported by mobile devices, such as cell phones, patient monitoring devices, personal digital assistants, and other wireless devices [4]. The capillarity now achieved by radio infrastructures makes mHealth technologies functional. Mobile connection networks, in 2016, reached 84% of the world population [5]; according to Pew Research Center, 95% of Americans have a generic mobile phone, while 85% use a smartphone [6]. With regard to Italy, 100% of the Italian population is covered by mobile connection networks, both 3G and 4G bands; 92% of the population own a mobile phone [7]. mHealth techniques are frequently used, independently by the subjects or inserted in specific rehabilitation programs, for the treatment of addiction to substances of abuse, such as nicotine, or in interventions aimed at supporting individuals on smoking cessation paths; in these cases, researchers speak of mobile phone-based smoking cessation support, or mCessation interventions [8]. Moreover, mHealth programs based on smartphone applications are used in alcohol use disorder treatments [9] and, albeit to a much lesser extent, in heroin addiction treatments [10].
2. Characteristics of the Included Studies
The database search identified a total of 8891 articles. After excluding duplicates, researchers found 3556 unique records, which were initially screened, based on title and abstract data. A total of 611 full-text articles were assessed for eligibility, and 28 out of these met the inclusion criteria and were included in the review; 583 were excluded because they did not meet the inclusion criteria (flow diagram, Figure 1).
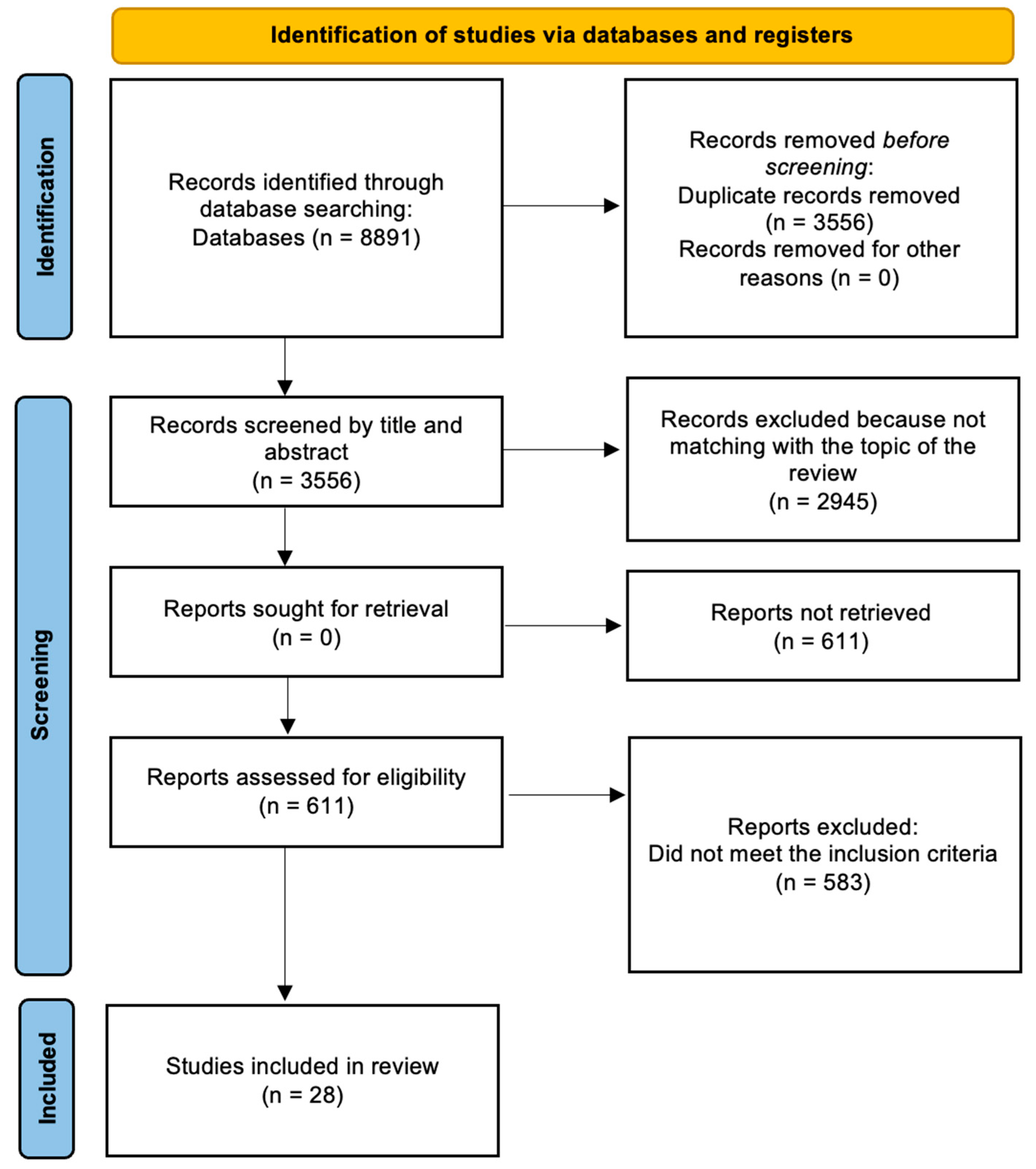
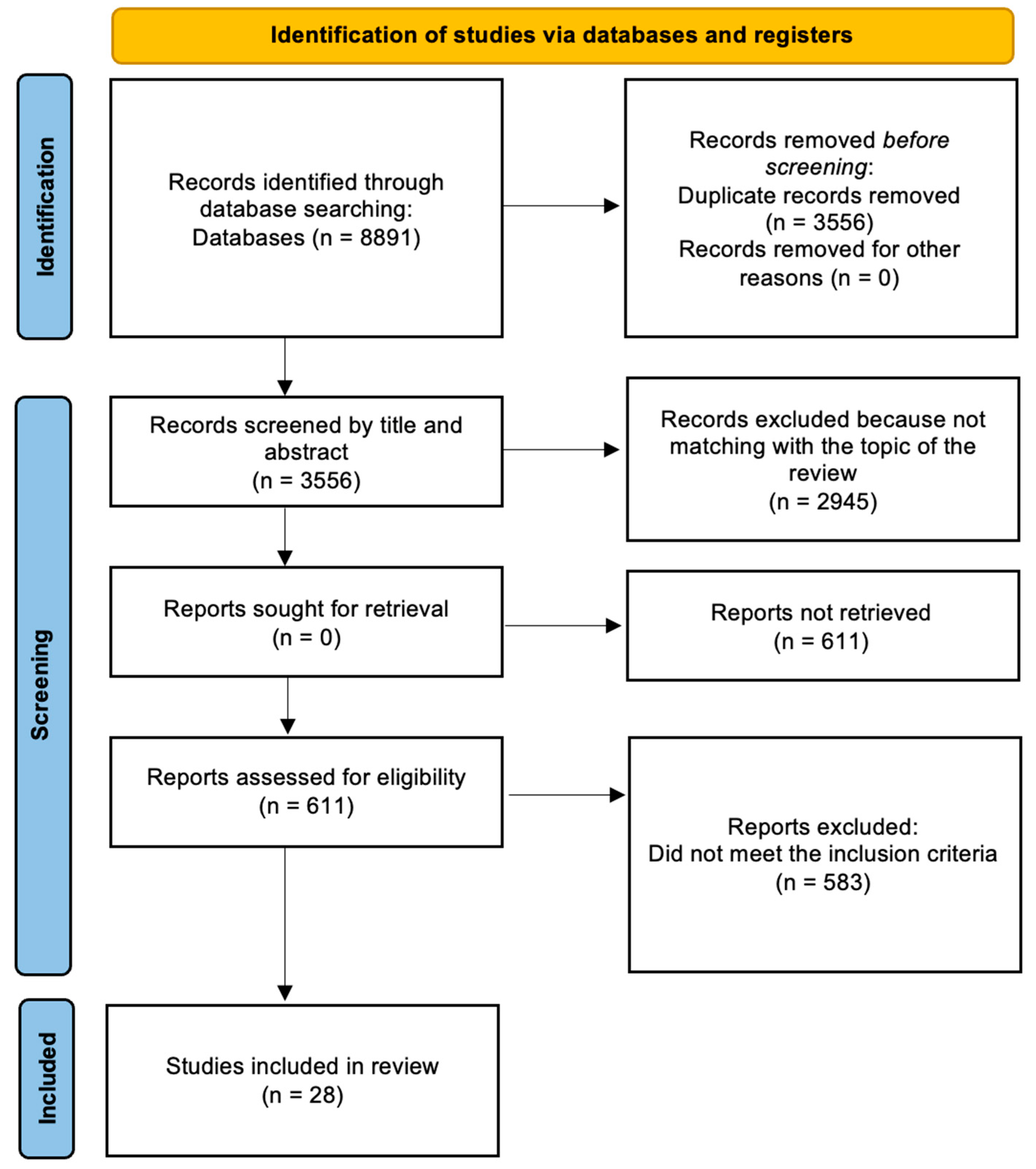
Figure 1. PRISMA (2020) flow diagram.
23. The Implementation of Virtual Reality in Psychotherapeutic Treatments
Virtual Reality was found to be an effective tool in mental health fields. In a randomized controlled trial for social anxiety, Bouchard et al. [11] reported that conducting exposure in VR was found to be more effective post-treatment than in vivo on the primary outcome measure and one secondary measure; furthermore, improvements were maintained at the 6-month follow-up, suggesting that using VR can be advantageous over standard cognitive–behavioral therapy (CBT) as a potential solution for treatment avoidance and as an efficient, cost-effective, and practical medium of exposure.
This tool has also been used in therapies with patients suffering from schizophrenic spectrum disorder with promising results, proving to be particularly effective in the treatment of psychotic symptoms, such as delusions and hallucinations, and cognitive and social skills; there is a general agreement in the literature on the safe, tolerable, and long-term persistence of the therapeutic effects obtained by immersive VR. In addition, no serious side effects have been reported [1]. The usefulness of Virtual Reality in the treatment of psychotic disorders derives from the fact that this tool can represent social environments that trigger responses, reactions, and emotions equivalent to what the real world in a given context would create in the mind of patients [12][13]; similarly, a virtual person (avatar) will elicit reactions similar to those provoked in real life [14].
Dellazizzo et al. [15] found that treatments employing VR stress-provoking scenarios significantly decreased the frequency and intensity of anger, as well as significantly decreasing core PTSD symptoms; they also analyzed a cognitive training program with immersive VR based on a virtual classroom and electroencephalogram (EEG) biofeedback for symptoms of attention-deficit hyperactivity disorder (ADHD). The program did not show significant improvements in both the VR and non-VR group scores, although the VR group improved the most.
The most recent literature also states that Virtual Reality Exposure Therapy (VRET) proved to be a valid alternative to “In Vivo” therapies (iVET) for the treatment of social anxiety disorder and its various forms. Caponnetto et al. [16] found, through the analysis of various studies, that the effectiveness of these two types of treatment is comparable, stating that “the superiority of VRET over iVET should not be seen as much in the perspective of the reduction in symptoms, since they seem to be equally effective, but in the drastic reduction in the costs to carry out the therapy and in the flexibility that allows the clinician to control all the variables at stake”. The cost effectiveness of VRET may today represent the turning point for wider access to psychological care to currently excluded socioeconomic classes (Table 1).
Table 1. Characteristics of Virtual Reality concerning the effects found in psychotherapy treatments and the advantages of this tool.
| Characteristics of Virtual Reality | |
|---|---|
| Effects in Psychotherapy | More effective at post-treatment than in vivo Improvements maintained for at least 6 months Effective in the treatment of psychotic symptoms Decreases the frequency and intensity of anger Decreases core PTSD symptoms Potential benefits in impulsivity treatments |
| Medium Advantages | Efficient Cost effective Practical Safe Tolerable No serious side effects Flexible, possibility of controlling all the variables at stake |
34. The Advent of Mobile Health
Mobile Health exploits the use of mobile devices and their functionalities, and it includes simple strategies, such as the use of the short messaging service (SMS or text messages), and more complex strategies, such as using smartphone applications (Apps), telecommunication systems 3G/4G, general packet radio service (GPRS), global positioning system (GPS), and Bluetooth technologies [4]. More recently, the use of sensors to monitor and provide feedback to suppliers and patients about biological parameters is fueling new areas of both research and development. The fact that it is such a widespread tool makes the smartphone also extremely useful for clinical rehabilitation.
34.1. mHealth and Clinical Rehabilitation
Choi et al. [17] demonstrated the effectiveness of stroke rehabilitation programs using video games in Virtual Reality on smartphones. The mobile game-based VR program effectively promoted upper extremity recovery in patients with stroke; in addition, patients completed the treatment without adverse effects and were generally satisfied with the program. As stated by the authors, “this mobile game-based VR upper extremity rehabilitation program can substitute for some parts of the conventional therapy that are delivered one-on-one by an occupational therapist. This time-efficient, easy to implement, and clinically effective program would be a good candidate tool for telerehabilitation for upper extremity recovery in patients with stroke”. Researchers can see that one of the recurring positive factors of new technologies, in addition to easy applicability, is the low cost of use.
Song et al. [18] used smartphones as telemonitoring platforms for rehabilitation exercises with patients with coronary heart disease; the results of this study showed that patients in the intervention group had more significant improvement in exercise tolerance compared with those in the control group. The authors stated, however, that “it must be noted that both study arms indicated a tendency towards improvement regardless of intervention; although, the improvement was more obvious in group A”. Improvements in exercise tolerance can lead to greater consistency in exercise rehabilitation programs, producing better outcomes and increasing patients’ compliance.
Nehrujee et al. [19] worked on successfully verifying the usability of a smartphone-based gaming system for vestibular rehabilitation. Unlike all existing systems for vestibular rehabilitation, VEGAS—the smartphone-based gaming system VR HMD used in the study—is convenient, compact, portable, and suitable for training a wide range of exercises both in clinics and in patients’ homes. According to the authors, the system was reported to be highly usable by both healthy subjects and patients included in the study; furthermore, they “strongly believe that the smartphone-based HMD approach has significant potential to become an affordable, portable, and safe tool for vestibular rehabilitation”, therefore remarking how these instruments, which improve year after year, are functional and convenient from every point of view (Table 2).
Table 2. Forms of mHealth, areas of use in clinical rehabilitation, and medium advantages.
| Characteristics of mHealth | |
|---|---|
| Forms of mHealth tools | SMS (short text messages) Smartphone applications Smartphones as telemonitors Mobile game-based VR systems |
| Areas of use in clinical rehab | Upper extremity recovery in patients with stroke Rehab exercises with patients with coronary heart disease Vestibular rehabilitation |
| Medium advantages | No adverse effects General patients’ satisfaction Low cost Time efficient Easy to implement Clinically effective Highly usable Safe |
34.2. Mobile Phone-Based Smoking Cessation Support (mCessation)
mHealth systems were also used as part of interventions aimed at supporting individuals on smoking cessation paths; in these cases, as already written in the Introduction, researchers speak of mobile phone-based smoking cessation support, or mCessation interventions [8]. According to the data, in 2019, there were over 1 billion smokers worldwide, and they consumed over 7 trillion cigarettes. The proportion of people who smoke globally has decreased since 1990, while, with population growth, the absolute number of smokers has grown in many parts of the world; moreover, also since 1990, the global prevalence of smoking among subjects aged between 15 and 24 years has decreased significantly, although the absolute number of young smokers has increased in some regions due to the growth of the population itself. In 2019 alone, tobacco smoking was held directly responsible for the deaths of 7.69 million people [20]. These and previous data have pushed toward the search for even better systems to combat the spread of tobacco and smoking addiction, identifying a useful ally first in the mobile phone and then in the smartphone.
A review conducted by Whittaker et al. [8], based on 26 studies with a total of over 33,000 participants, highlighted how the use of mCessation, in particular, the use of automated text message systems delivered to mobile phones, led to higher termination rates than the minimum standard for smoking cessation support. The authors specifically argue that there is moderate certainty of the benefit of interventions involving automated text messaging if used in addition to other smoking cessation support compared to only minimal smoking cessation support.
Deutsch et al. [21] described a similar system called Test My Quit (TMQ), also based on sending text messages on mobile phones, and highlighted its potential effectiveness. The design of this system consisted of a tailored smoking cessation intervention delivered 100% through text messaging to an intervention group in comparison with non-smoking-related text messages sent to a control group. The authors concluded the description of the design by asserting that, in addition to specificity and technicality, one of the strengths of Test My Quit is its total accessibility on the market, as it is based on text messages.
Liao et al. [22] conducted a text message-based smoking cessation intervention on the Chinese population, called Happy Quit, and found positive effects on a small number of subjects in the sample, suggesting greater efficacy on larger samples. This type of intervention was also studied with representative samples of minority populations, such as Somali nationals professing the Islamic religion by Pratt et al. [23] and pregnant women by Forinash et al. [24]; in the first case, positive prospects were recorded especially during the Ramadan period, while, in the second case, the impact of the intervention was minimal (also due to some problems that occurred during the recruitment phase and high drop-out rates).
45. Smartphone Applications Designed for Smoking Cessation
Another type of mHealth, used in support interventions for smoking cessation, concerns the use of smartphone applications specially designed for this purpose.
Regmi et al. [25] conducted a review involving eight studies of the clinical trial type or interventions, concerning smartphone applications designed for smoking cessation. From the reported results, it is clear that this is an area that is still embryonic but of certain interest and that requires constant further study; the use of such applications appears to produce an increase in cessation rates among smokers, although adherence to the internal functionalities of the application appears to influence cessation rates; “audiovisual features followed by a quit plan, progress tracking and sharing features are the most liked and used application features”, although “inconsistency in their association with abstinence or termination rate has been observed”. The authors also report a reduction in relapses attributed to debates carried out on social media among those who quit smoking. Regmi and colleagues conclude by suggesting carrying out studies with applications of this type on larger samples to measure the effectiveness of the intervention more clearly.
Pbert et al. [26] compared the effectiveness of interventions aimed at smoking cessation: two interventions based on smartphone applications specifically designed to help people quit smoking and based on mindfulness training, one called Craving to Quit (C2Q) and the other QuitSTART, while the third intervention involved the use of written material. The selected sample included 146 adolescents. The authors found that “cotinine-validated abstinence (tobacco alkaloid and nicotine metabolite) was similar between intervention conditions and tended to increase with (subject’s) greater engagement in each condition”. They go on to state that “a greater involvement of the C2Q App among heavy smokers was associated with a significantly greater decline in the number of cigarettes smoked, compared to other conditions”. The Craving to Quit App was also employed in a randomized controlled experiment conducted by Garrison et al. [27]; although the results led to the conclusion that the mindfulness training through the App “did not lead to a reduction in smoking rates compared to the control group”, useful data were found to hypothesize that this system may loosen the association between craving and smoking, which would be particularly useful in supporting cessation in long-term programs.
Another application studied was Quit2Heal, in comparison with the QuitGuide of the US National Cancer Institute, by Bricker et al. [28]. In this case, the sample was composed exclusively of cancer patients, and the application showed “promising acceptability and efficacy in helping cancer patients to quit smoking”.
References
- Bisso, E.; Signorelli, M.S.; Milazzo, M.; Maglia, M.; Polosa, R.; Aguglia, E.; Caponnetto, P. Immersive Virtual Reality Applications in Schizophrenia Spectrum Therapy: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 6111.
- Aida, J.; Chau, B.; Dunn, J. Immersive virtual reality in traumatic brain injury rehabilitation: A literature review. Neurorehabilit 2018, 42, 441–448.
- Dockx, K.; Bekkers, E.M.; Van den Bergh, V.; Ginis, P.; Rochester, L.; Hausdorff, J.M.; Mirelman, A.; Nieuwboer, A. Virtual reality for rehabilitation in Parkinson’s disease. Cochrane. Database. Syst. Rev. 2016, 12.
- Ryu, S. Book Review: mHealth: New Horizons for Health through Mobile Technologies: Based on the Findings of the Second Global Survey on eHealth (Global Observatory for eHealth Series, Volume 3). Healthc. Inform. Res. 2012, 18, 231.
- International Telecommunication Union. ICT Facts & Figures 2016. Available online: https://www.itu.int/en/ITU-D/Statistics/Documents/facts/ICTFactsFigures2016.pdf (accessed on 21 January 2022).
- Pew Research Center, author. Pewinternet. Mobile Fact Sheet Internet. Available online: http://www.pewinternet.org/fact-sheet/mobile/ (accessed on 21 January 2022).
- International Telecommunication Union. Digital Development 2016. 2020. Available online: https://www.itu.int/en/ITU-D/Statistics/Dashboards/Pages/Digital-Development.aspx (accessed on 19 January 2022).
- Whittaker, R.; McRobbie, H.; Bullen, C.; Rodgers, A.; Gu, Y.; Dobson, R. Mobile phone text messaging and app-based interventions for smoking cessation. Cochrane. Database. Syst. Rev 2019, 10.
- Gonzalez, V.M.; Dulin, P.L. Comparison of a smartphone app for alcohol use disorders with an Internet-based intervention plus bibliotherapy: A pilot study. J. Consult. Clin. Psychol. 2015, 83, 335–345.
- Schulte, M.; Liang, D.; Wu, F.; Lan, Y.C.; Tsay, W.; Du, J.; Zhao, M.; Li, X.; Hser, Y.I. A Smartphone Application Supporting Recovery from Heroin Addiction: Perspectives of Patients and Providers in Taiwan, China, and the USA. J. Neuroimmune. Pharmacol. 2016, 11, 511–522.
- Bouchard, S.; Dumoulin, S.; Robillard, G.; Guitard, T.; Klinger, É.; Forget, H.; Loranger, C.; Roucaut, F.X. Virtual reality compared with in vivo exposure in the treatment of social anxiety disorder: A three-arm randomised controlled trial. Br. J. Psychiatry 2017, 210, 276–283.
- Freeman, D. Studying and treating schizophrenia using virtual reality: A new paradigm. Schizophr. Bull. 2007, 34, 605–610.
- Freeman, D.; Bradley, J.; Antley, A.; Bourke, E.; DeWeever, N.; Evans, N.; Cernis, E.; Sheaves, B.; Waite, F.; Dunn, G.; et al. Virtual reality in the treatment of persecutory delusions: Randomised controlled experimental study testing how to reduce delusional conviction. Br. J. Psychiatry 2016, 209, 62–67.
- Meehan, M.; Insko, B.; Whitton, M.; Brooks, F.P., Jr. Physiological measures of presence in stressful virtual environments. ACM Trans. Graph. 2002, 21, 645–652.
- Dellazizzo, L.; Potvin, S.; Bahig, S.; Dumais, A. Comprehensive review on virtual reality for the treatment of violence: Implications for youth with schizophrenia. Npj Schizofrenia 2019, 11.
- Caponnetto, P.; Triscari, S.; Maglia, M.; Quattropani, M.C. The Simulation Game—Virtual Reality Therapy for the Treatment of Social Anxiety Disorder: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 13209.
- Choi, Y.H.; Paik, N.J. Mobile Game-based Virtual Reality Program for Upper Extremity Stroke Rehabilitation. J. Vis. Exp. JoVE 2018, 133, 56241.
- Song, Y.; Ren, C.; Liu, P.; Tao, L.; Zhao, W.; Gao, W. Effect of Smartphone-Based Telemonitored Exercise Rehabilitation among Patients with Coronary Heart Disease. J. Cardiovasc. Transl. Res. 2020, 13, 659–667.
- Nehrujee, A.; Vasanthan, L.; Lepcha, A.; Balasubramanian, S. A Smartphone-based gaming system for vestibular rehabilitation: A usability study. J. Vestib. Res Equilib. Orientat. 2019, 29, 147–160.
- GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: A systematic analysis from the Global Burden of Disease Study 2019. Lancet 2021, 397, 2337–2360.
- Deutsch, C.; Bock, B.C.; Lantini, R.; Walaska, K.; Rosen, R.K.; Fava, J.L.; Jennings, E.G.; Foster, R.; Flanagan, W. A text message delivered smoking cessation intervention: Design and rationale of the Text My Quit Study. Contemp. Clin. Trials. 2019, 81, 19–27.
- Liao, Y.; Wu, Q.; Kelly, B.C.; Zhang, F.; Tang, Y.Y.; Wang, Q.; Ren, H.; Hao, Y.; Yang, M.; Cohen, J.; et al. Effectiveness of a text-messaging-based smoking cessation intervention (“Happy Quit”) for smoking cessation in China: A randomized controlled trial. PLoS Med. 2018, 15, e1002713.
- Pratt, R.; Ojo-Fati, O.; Adam, A.; Sharif, H.; Kahin, A.; Mahamud, A.; Dubois, D.; Mohamed, S.; Okuyemi, K.; Graham, A.L.; et al. Text Message Support for Smoking Cessation During Ramadan: A Focus Group Study with Somali Immigrant Muslim Men. Nicotine. Tob. Res. Off. J. Soc. Res. Nicotine. Tob. 2020, 22, 1636–1639.
- Forinash, A.B.; Yancey, A.; Chamness, D.; Koerner, J.; Inteso, C.; Miller, C.; Gross, G.; Mathews, K. Smoking Cessation Following Text Message Intervention in Pregnant Women. Ann. Pharmacother. 2018, 52, 1109–1116.
- Regmi, K.; Kassim, N.; Ahmad, N.; Tuah, N.A. Effectiveness of Mobile Apps for Smoking Cessation: A Review. Tob. Prev. Cessat. 2017, 3, 12.
- Pbert, L.; Druker, S.; Crawford, S.; Frisard, C.; Trivedi, M.; Osganian, S.K.; Brewer, J. Feasibility of a Smartphone App with Mindfulness Training for Adolescent Smoking Cessation: Craving to Quit (C2Q)-Teen. Mindfulness 2020, 11, 720–733.
- Garrison, K.A.; Pal, P.; O’Malley, S.S.; Pittman, B.P.; Gueorguieva, R.; Rojiani, R.; Scheinost, D.; Dallery, J.; Brewer, J.A. Craving to Quit: A Randomized Controlled Trial of Smartphone App-Based Mindfulness Training for Smoking Cessation. Nicotine. Tob. Res. Off. J. Soc. Res. Nicotine. Tob. 2020, 22, 324–331.
- Bricker, J.B.; Watson, N.L.; Heffner, J.L.; Sullivan, B.; Mull, K.; Kwon, D.; Westmaas, J.L.; Ostroff, J. A Smartphone App Designed to Help Cancer Patients Stop Smoking: Results from a Pilot Randomized Trial on Feasibility, Acceptability, and Effectiveness. JMIR Form. Res. 2020, 4, e16652.
More
