Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Bruce Ren and Version 1 by Dmitry Tretiakow.
Medicine is a rapidly-evolving discipline, with progress picking up pace with each passing decade. This constant evolution results in the introduction of new tools and methods, which in turn occasionally leads to paradigm shifts across the affected medical fields. The following review attempts to showcase how 3D printing has begun to reshape and improve processes across various medical specialties and where it has the potential to make a significant impact.
- 3D printing
- three-dimensional printing
- additive manufacturing
- cardiology
- surgery
- cardiac surgery
- urology
- obstetrics
- gynecology
- oncology
- radiotherapy
- orthopedics
- trauma
- otolaryngology
- head and neck surgery
- mandible reconstruction
- training
- simulation
- outcom
1. Introduction
Three-dimensional printing (3D printing, 3DP), also known as rapid prototyping or additive manufacturing, is not new in the tech industry. In fact, the first patents and prototypes in this field date back to the 1970s, with early additive manufacturing equipment and materials following in the subsequent decade. Various manufacturing methods have been developed, such as fused deposition modeling (FDM), selective laser sintering (SLS), stereolithography (SLA), to name a few. However, a major breakthrough in the broad-scale implementation of this technology happens after 2010, following the expiration of many relevant patents. This enabled the development of affordable desktop 3D printers, which further democratized 3DP technology and made it more accessible to the public [1]. This shift, in turn, led to the exploration of various medical implementations. While there were singular mentions of 3DP technology in PubMed prior to the year 2000, the subsequent two decades have shown exponential growth in the number of publications (Figure 1), a trend suggestive of a disruptive potential of 3DP technology.
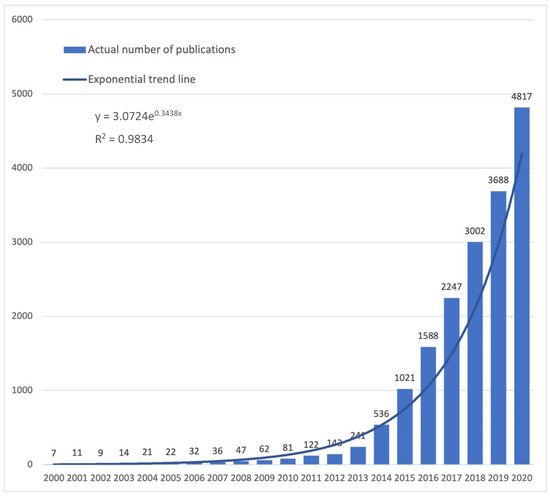
Figure 1. The number of PubMed indexed publications since 2000 (total 19,562) and fitting exponential trend line. Search query: 3D printing or additive manufacturing.
2. Three-Dimensional Printing Technique Overview
Patient-specific 3D models of anatomical structures can be generated from various medical imaging modalities in a multi-step process wthe researchers have detailed previously [2]. Most commonly, computed tomography (CT) and magnetic resonance imaging (MRI) volumetric datasets are used (Figure 2A). Transesophageal echocardiography (TEE) rotational angiography can also provide high-quality source image data. Irrespective of the modality employed, superb image fidelity is essential for quality 3D printing, as imaging faults and artifacts will complicate pre-print processing and, in the worst-case scenario, may be carried over to the final print [2,3,4][2][3][4]. On special occasions, multimodality imaging is employed to leverage the strengths of more than one imaging modality (Figure 3).
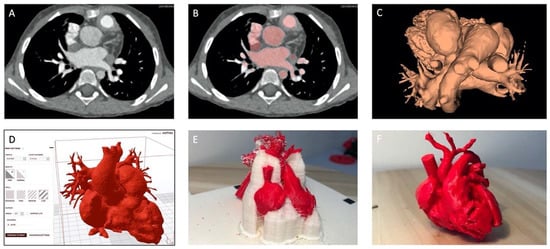
Figure 2. The steps in the process of 3D printing. (A). Source CT; (B). CT after segmentation (red); (C). Digital model (STL); (D). Print setup; (E). Raw print covered in support material; (F). Final 3D printed model. Detailed descriptions in text. (If not stated otherwise, images courtesy of Jarosław Meyer-Szary, Department of Pediatric Cardiology and Congenital Heart Defects, Faculty of Medicine, Medical University of Gdańsk, Gdańsk, Poland).
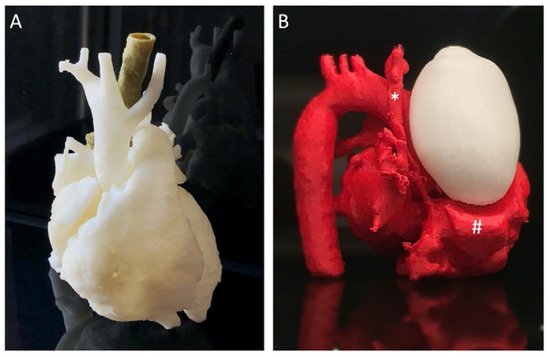
Figure 3. Examples of multi-part models. (A) a case of the aortic ring, to visualize a compressed trachea by adjacent, abnormally positioned vessels, a cardiovascular model is printed in white and, separately segmented, the trachea is printed green and fitted in place; (B) a case of a neonate with a mediastinal tumor (white) compressing the cardiovascular structures (red), the superior vena cava (asterisk) and the right atrium (hashtag), the model was based on multimodality imaging owing to the fact that Angio CT has a superior special and temporal resolution for cardiovascular structures while MRI has superior ability to differentiate soft tissue structures and tumors. Parts of the models coming from different modalities were assembled in post-production.
The source images are imported from Digital Imaging and Communications in Medicine (DICOM) format into a specialized software platform designed for medical image analysis and processing (Figure 2A). Segmentation (Figure 2B) is the key step of identifying target anatomical elements and excluding extraneous components through an automated, manual, or semi-automated process. This segmented dataset is converted into a STereoLithography (STL) file (Figure 2C) and passed on to printer-specific software to set up print parameters (Figure 2D). The resultant file is passed on to the printer. Numerous 3D printing techniques and a vast array of materials are available, with unique properties such as the type of the print process, print time, model durability, compliance, flexibility, and translucency, which lend themselves to various applications. Once the printer is set up and the print is started, little to no user intervention is required. However, the newly-printed model is rarely finished at this point (Figure 2E). Typically, post-processing is required before a finished model (Figure 2F) is made and ready to be used in, for instance, a procedure simulation. This post-processing may include removal of support parts (manually or by dissolving), sanding and polishing, chemical smoothing, UV curing, assembly in case of multi-part models (Figure 3), etc. Each of the steps (image pre-processing and digital model creation, actual printing, and print post-processing) are relatively time-consuming, taking a number of hours on average, while most (with the exception of printing itself) also tend to be labor-intensive. Overall, this currently renders the 3DP process sub-optimally suited to urgent applications or emergency situations.
3. Application of 3D Printing in Medicine
Despite the limitations, 3D printing has found its way to multiple applications in various fields of medicine, as depicted in Figure 4, with each field having come a long way over the recent decades. Overall, the chief advantage of 3DP is the ability to transform two-dimensional imaging of a patient, once merely viewable on a flat screen, into a tactile 3D model that can be appreciated in real space, handled, physically manipulated, and even deformed. Clinical applications, which deal with complex anatomical relationships and rely on advanced imaging modalities to make judgments and plan possible interventions, are poised to derive the greatest benefit from advances in 3DP.
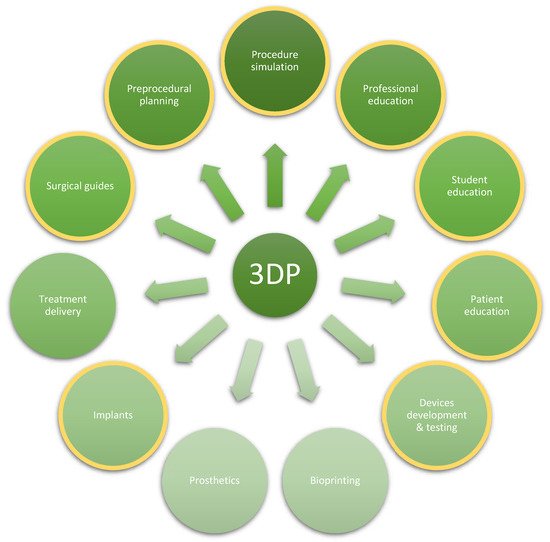
Figure 4. The breadth of medical applications of 3D printing. Highlighted in yellow are those in focus in this review. The list is non-exhaustive, and new applications are evolving.
Likewise, improvements in 3DP technology have created new avenues for the development and applications across other specialties and domains. Today, 3D printing is being progressively integrated into and has begun to reshape surgical practice as well as surgical training, with recent reports having shown possible uses of 3DP across several subspecialties. Perhaps best suited to take advantage of 3DP are those that deal with the skeleton. The significantly higher density of bone compared to surrounding soft tissue facilitates imaging segmentation and thus lends itself optimally to 3D modeling. However, specialists in multiple fields, whether dealing primarily with bone or with soft tissues, are poised to derive benefits from 3DP technology as an adjunct to pre-procedural planning in education, training, simulation, or practice ahead of complex, uncommon, or high-risk procedures, or as means of surgical guidance, or even for custom 3D-printed tools, devices, and patient-specific prostheses and implants.
Selected examples of the various applications of 3DP are showcased in the following sections, as pertaining to the respective individual disciplines of pediatric (cardiac) surgery, and interventional cardiology, adult general and orthopedic surgery, otorhinolaryngology, head and neck surgery, neurosurgery, gynecology, and obstetrics, urology, as well as emergency medicine, anesthesiology, and radiation oncology.
From education, through diagnostics, to definitive treatment, the modern multidisciplinary approach has progressed to a stage where individualized therapy has become simpler and more broadly accessible. This is further facilitated by the implementation of 3DP technology with models being utilized for surgical planning, simulation-based training, and education, developing surgical guides and other tools, as well as counseling of patients. Manufacturing options range from Fused Deposition Manufacturing (FDM) Polylactic Acid (PLA) prints of fracture sites, used for pre-operative planning, to more complex Direct Metal Laser Sintering (DMLS) Titanium prints of patient-specific implants, and finally, bio-implants 3D printed with bio-ink currently undergoing animal testing. Current clinical applications, shown to benefit directly from the involvement of 3DP models, ranging from treatment of pectus excavatum, diaphragmatic hernia, hydrocephalus, tracheobronchomalacia, as well as oncologic resection and reconstruction, to name a few. Hence, 3D printing clearly has a wide area of potential applicability (Figure 4). However, it is not yet established as the first method of choice, with traditional solutions preferred in many centers. Nevertheless, moving forward, 3D printing offers extensive opportunities not only to improve treatment and patient outcomes but also to enable advanced training of future physicians and surgeons. It can also be used as a valuable tool for patient education prior to complex surgical procedures or less invasive interventions.
References
- Antreas, K.; Piromalis, D. Employing a Low-Cost Desktop 3D Printer: Challenges, and How to Overcome Them by Tuning Key Process Parameters. Int. J. Mech. Appl. 2021, 10, 11–19.
- Luo, H.; Meyer-Szary, J.; Wang, Z.; Sabiniewicz, R.; Liu, Y. Three-Dimensional Printing in Cardiology: Current Applications and Future Challenges. Cardiol. J. 2017, 24, 436–444.
- Garg, R.; Zahn, E.M. Utility of Three-Dimensional (3D) Modeling for Planning Structural Heart Interventions (with an Emphasis on Valvular Heart Disease). Curr. Cardiol. Rep. 2020, 22, 125.
- Meyer-Szary, J.; Woźniak-Mielczarek, L.; Sabiniewicz, D.; Sabiniewicz, R. Feasibility of In-House Rapid Prototyping of Cardiovascular Three-Dimensional Models for Planning and Training Non-Standard Interventional Procedures. Cardiol. J. 2020, 26, 790–792.
More
