Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Ludger Johannes and Version 2 by Dean Liu.
One mucosal vaccine candidate is the B-subunit of Shiga toxin, STxB. STxB is a non-toxic protein that binds to a glycosylated lipid, termed globotriaosylceramide (Gb3), which is preferentially expressed by dendritic cells.
- glycolipid-lectin
- GL-Lect
- endosomal escape
- cross-presentation
- tissue resident memory T cells
1. Shiga Toxin and Its Intracellular Trafficking
The bacterial Shiga toxin belongs to the family of AB5 toxins [1]. These are composed of a catalytic A-subunit and a homopentameric B-subunit which is made from five identical B-fragments. The B-subunits of AB5 toxins bind to glycans of cellular protein or lipids [2]. The cellular receptor of the B-subunit of Shiga toxin (abbreviated as STxB) is the glycosphingolipid globotriaosylceramide (Gb3 or CD77) [3]. Of note, STxB is needed not only for toxin binding to cells, but also for the trafficking of the catalytic A-subunits inside the cells [4] (Figure 1). With the help of STxB, the A-subunit of Shiga toxin is delivered into the cytosol where it inhibits protein biosynthesis by modifying ribosomal RNA. This leads to cell death and contributes to the overall pathology that is associated with Shiga toxin producing enterohemorrhagic Escherichia coli bacteria, which bring about hemolytic-uremic syndrome, the leading cause of pediatric renal failure [5][6][5,6], but which also poses health risks to adults [7].
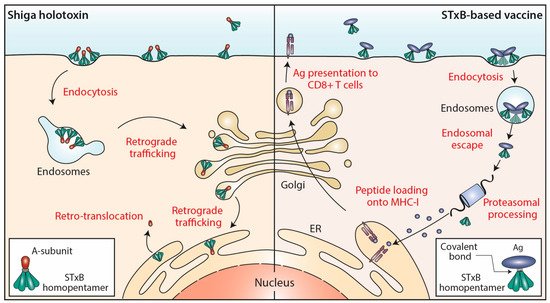
Figure 1. STxB trafficking into cells. Left: Shiga holotoxin molecules are composed of a STxB homopentamer (green) and a catalytic A-subunit (red), which are non-covalently associated. STxB binds to the plasma membrane of target cells via the glycosphingolipid Gb3 (not shown). STxB induces an increment of spontaneous curvature, which upon membrane-mediated clustering of several toxin molecules leads to the formation of endocytic pits from which clathrin-independent carriers are generated for toxin trafficking to early endosomes. From there, the holotoxins are transported via the retrograde trafficking route to the endoplasmic reticulum (ER), via the Golgi apparatus. The catalytic A-subunit is then translocated to the cytosol where it inhibits protein biosynthesis by modifying ribosomal RNAs (not shown). Right: In STxB (green)-based vaccines, antigens (blue) are linked via covalent bonds to the vector. The endocytic process then operates as for Shiga holotoxin molecules. While STxB-antigen conjugates also undergo retrograde trafficking (not shown), a small fraction of them escapes from the lumen of endosomes to reach the cytosol (endosomal escape). Here, proteasomes process the antigens to generate antigenic peptides, that are then imported into the lumen of the ER (or of endo/phagosomal processing compartments; not shown) for loading onto MHC class I molecules and subsequent presentation at the plasma membrane to CD8+ T cells.
The endocytic and intracellular trafficking of STxB has been analyzed in some detail (Figure 1). At the plasma membrane, STxB reorganizes lipids, including its receptor glycolipid Gb3, in a way such that narrow tubular endocytic pits are formed [8] by exploiting a specific geometry of Gb3 binding sites on STxB [9] and its capacity to induce an asymmetric compressive stress onto the membrane leaflet to which it binds [10]. STxB-Gb3 complexes are then clustered by membrane-mediated mechanism, likely involving lipid fluctuation forces [11]. This mechanism of building endocytic pits without the need for the conventional clathrin machinery has been termed the glycolipid-lectin (GL-Lect) hypothesis [12][13][12,13]. This GL-Lect mechanism has been suggested to apply also for the structurally related glycolipid-binding B-subunit of cholera toxin [14][15][16][14,15,16].
The toxin-induced tubular endocytic pits then detach by scission from the plasma membrane to form clathrin-independent endocytic carriers [17]. This scission reaction involves the conventional pinchase dynamin [8] and also actin-driven domain boundary forces [18] and a mechanism that has been termed friction-driven scission in which the pulling of the molecular motor dynein on tubular endocytic pits that are scaffolded by the BAR domain protein endophilin leads to the thinning of their necks and to subsequent detachment [19][20][19,20]. The thereby generated clathrin-independent endocytic carriers are then targeted in a SNARE protein-dependent manner to early endosomes [21].
From early endosomes, STxB is delivered by retrograde transport to the endoplasmic reticulum, via the Golgi apparatus (reviewed in [22][23][24][22,23,24]) (Figure 1). From there, the catalytic A-subunit is translocated to the cytosol using the cellular retrotranslocation machinery [25].
2. STxB Functions as a Mucosal Delivery Vector
2.1. The Mucosal Immune System and Its Specific Effectors
The mucosal immune system, also called MALT (mucosa-associated lymphoid tissue), is an integrated and well-organized architecture covering the lung, head and neck, digestive and genital mucosa. It is made of lymphoid follicles that are associated with a layer of T, B, and antigen presenting cells. These immune cells, which are close to the epithelium and M cells, represent between 10 and 20% of the epithelial barrier. M cells play an important role in the internalization and transfer of antigens to DCs [26][131]. A first priming of immune responses takes place at this follicle-associated epithelium (FAE), which is also called mucosal inductive site. Thereby induced immune cells reach the adjacent lymph nodes upon which they return to the very mucosa in which they had been generated [27][28][132,133].
Compared to the immune response induced by peripheral lymph node priming, the mucosal immune response is characterized by two immune effectors that are specifically found in mucosal tissues: secretory IgA and resident memory T cells [29][134]. In contrast to IgA in serum, secretory (s)-IgA antibodies are produced locally in the mucosa and are more resistant to bacterial enzymes. sIgAs are the key immune effector molecules in the mucosa. After binding to polymeric immunoglobulin (Ig) receptors (pIgRs), sIgAs are transported across mucosal epithelial cells to the intestinal lumen or other mucosa. Only mucosal and not systemic immunization pathways can generate them [30][31][135,136]. Their presence in mucosal sites is associated with optimal vaccine protection against viral infections [32][33][137,138].
More recently, a new non-recirculating lineage of T cells has been described in mucosal tissues, which were termed tissue resident memory (TRM) T cells [34][35][139,140]. TRM specifically differentiate in the mucosal tissue and are not found in the blood. They express the CD103 marker which binds to epithelial cell-specific E-cadherin. TRM are thought to play an immunosurveillance role in the mucosa. Their presence in the vicinity of the epithelium allows them to act rapidly in the event of infection and to promote the swift recruitment of new effectors without the need for a lengthy T-cell differentiation process in lymph nodes [36][141]. TRM have also been found in tumors especially in mucosal localization and are associated with a favorable prognosis [37][38][142,143]. As for sIgAs, mucosal routes of immunization are more efficient in inducing TRM than conventional systemic routes [39][144].
2.2. STxB—The First Non-Live Mucosal Delivery Vector That Induces TRM
ItWe is sshowed that intranasal immunization with conjugates between STxB and the E7 protein from human papilloma virus 16 (HPV16) is more effective in inducing mucosal IgAs and anti-E7 CD8+ T cells in the lung than intramuscular immunization [40][145]. Intranasal STxB-E7 immunization promotes intratumoral CD8+ T cell recruitment and the regression of E7-expressing tumor in the lung or head and neck mucosa. In contrast, intramuscular immunization with STxB-E7 induces CD8+ T cells in blood and spleen, but not in the lung and has no significant effect on the growth of a tumor xenograft in the tongue. The intranasally induced CD8+ T cells express CD103 and CD49a and have a TRM phenotype. Of note, these cells are not induced when STxB-E7 is injected via the intramuscular route of immunization [40][41][145,146].
In a series of experiments based on the elimination of TRM, the blocking of their differentiation or migration, or their isolation by parabiosis, rwesearchers have clearly shown their role in the inhibition of tumor growth after immunization of mice with different STxB-antigen conjugates [41][146]. More recently, reswearchers have shown that TRM preferentially express the chemokine receptor CXCR6, when compared to effector CD8+ T cells [42][147]. Immunization via the intranasal route and not the intramuscular route allows to induce the chemokine CXCL16 in the lung, which could explain the recruitment of TRM [42][147].
These studies demonstrate for the first time that a protein-based vector targeting DCs induces TRM, and that the nasal immunization route is required for this. Earlier work had already pointed to the possibility that STxB might act as a mucosal delivery vector. Indeed, a STxB fusion protein with a rotavirus NS4 polypeptide was shown to increase intestinal IgA concentrations and serum IgG when administered orally, and to protect breastfeeding pups against diarrhea after an infectious challenge [43][148].
2.3. Other Mucosal Vaccination Strategies
Preparations based on vesicular stomatitis virus (VSV), adenovirus 26 (ADV26), or modified vaccinia virus Ankara have enabled the commercialization of vaccines against Ebola virus [44][45][149,150]. Intranasal administration of recombinant preparations based on cytomegalovirus (CMV)-derived viruses, influenza virus, ADV, VSV have been shown to induce IgA and TRM in different mucosal locations [46][47][48][49][151,152,153,154]. In a preclinical model of infection with SARS-CoV-2, a recombinant chimpanzee ADV (ChAdOx1)-encoding SARS-CoV-2 Spike administered nasally or subcutaneously was shown to protect against lung infection after a viral challenge, but only intranasal administration of the vaccine protects against upper airway infection. This protection is associated with the preferential induction of local mucosal IgA and TRM [50][155].
Few non-live vectors have been tested for their ability to deliver antigens via the mucosal route. For example, conjugates between the non-toxic B-subunit of cholera toxin and bacterial or viral antigens increase antigen-specific IgA compared to non-vectorized antigen when they are administered nasally or sublingually [51][52][156,157]. Upon nasal or subcutaneous administration, a scFv directed against DEC-205 and coupled to a parasite antigen increases IgA concentrations in nasal washings as well as a CD4+ T-cell response in the spleen, allowing partial protection against a parasite challenge [53][158].
More generally, two main mucosal delivery tools are developed for vaccine:
- (i)
-
Lactic acid bacteria (LAB) that include Lactobacillus spp., Lactococcus spp., and Streptococcus spp. LAB are generally recognized as safe and considered as transiting and non-invasive bacteria [54][55][159,160].
- (ii)
-
Nanoparticles, i.e., (a) polysaccharide-based natural polymers such as chitosan, pullulan, alginate, inulin, hyaluronic acid, maltodextrin; (b) lipid-based delivery systems (i.e., cationic liposomes, virions, archaeological bodies, small cochlea, and immunostimulating complexes); (c) synthetic polymeric nanoparticles (poly(lactic-co-glycolic acid), polycaprolactone, polyahydrides, polyphosphazene). These polymers have the advantage of being biodegradable.After mucosal administration, LABs and nanoparticles generate mucosal responses against entrapped antigens [56][57][58][59][161,162,163,164]. To improve their efficacy, LABs such as lactobacillus have been coupled with DC targeting peptides; alternatively, complement C3d3, anti-CD205, anti-CD11c, or neonatal Fc receptors (FcRn) have been expressed at their surface [60][61][62][63][165,166,167,168]. Nanoparticles such as poly(lactic-co-glycolic acid) and liposomes have also been functionalized with anti-DEC-205 [64][169], anti-CD40 [65][170], anti-mannose receptor [66][171], or anti-CD11c [67][172] antibodies to target them to DCs. These elegant strategies, which combine mucosal delivery, DC targeting, and the possibility to incorporate multiple cargo molecules are up until now limited by issues related to reproducibility of their synthesis and scale up for clinical application.Regarding RNA vaccines, their direct intranasal administration without encapsulation does not lead to the induction of a mucosal immune response [68][173]. Some studies show that their encapsulation as nanoparticles, cationic liposome/protamine complexes (LPC), or mannose-conjugated lipid nanoparticles generate cellular responses that inhibit tumor growth [68][69][70][173,174,175]. Xun Sun’s group demonstrated that cationic cyclodextrin-polyethylenimine 2k conjugates (CP 2k) which are complexed with anionic mRNA-encoding HIV gp120 induce strong systemic and mucosal anti-HIV immune responses [71][176]. Nevertheless, toxicity problems have been reported with polyethyleneimine and lipid nanoparticles when these are injected via the nasal route [72][73][74][177,178,179]. Improving the benefit-risk balance and the efficacy of these mucosal RNA vaccines is the subject of numerous ongoing studies.
3. STxB in Combination with Other Cancer Treatment Modalities
Apart from a few positive clinical signals of therapeutic HPV vaccines in pre-neoplastic cervical lesions, no therapeutic vaccine has demonstrated sufficient efficacy in patients with advanced cancer or chronic infection (e.g., HIV) to change clinical practice [35][140]. An in-depth investigation of the tumor microenvironment has revealed the existence of immunosuppressive mechanisms that likely explain the failure of therapeutic vaccines in advanced stage cancers [75][180]. Indeed, T cells that migrate into tumors quickly become exhausted and express inhibitory receptors like PD-1. Blocking the interaction between PD-1 and PD-L1 has led to the success of immunotherapy in many clinical indications [76][77][181,182]. Second generation immunotherapy protocols are therefore developed in which an inhibition of the PD-1/PD-L1 pathway is combined with vaccines or conventional treatments [78][183].In preclinical models, reswearchers were one of the first teams to show that this combinatorial approach might indeed be successful [79][184]. In mice with HPV E7-expressing tumors, administration of either a STxB-E7 vaccine or an anti-PD-1 antibody led to only a partial therapeutic response. In contrast, the combination of both induced total tumor regression [79][184]. The value of combining a STxB-based vaccine with anti-PD-1 antibodies (and the local injection of IFNα) was also confirmed by another group [80][81][185,186].Regulatory T cells are another type of the immunosuppressive cells in the tumor microenvironment that counteract vaccine efficacy. RWesearchers have shown that the combination of a Treg inhibitor targeting the CCR4 pathway with a vaccine composed of STxB coupled to self-antigens overcomes tolerance and allows to eliminate tumors that express these self-antigens [82][187]. This combination proved to be effective in inhibiting the growth of numerous tumors (i.e., melanoma, colon cancer, and lung cancer). A similar synergistic effect was observed in the presence of a mTor pathway inhibitor [83][188].In many clinical indications, a therapeutic vaccine would need to be combined with conventional treatments such as radiotherapy or chemotherapy. In collaboration with Eric Deutsch’s group, rwesearchers have shown in a head and neck cancer model that radiotherapy increases the effect of a STxB-E7 vaccine by making endothelial cells more permissive to infiltration by CD8+ T cells [84][189].As summarized above and also in other studies [85][86][190,191], the STxB vector has been used reproducibly by independent groups for the preclinical development of immunotherapy applications. These studies support the design of clinical trials including STxB-based vaccines in 2nd generation immunotherapy strategies.
