Nutrition can affect, negatively or positively, sperm quality and this effect depends on both quantitative and qualitative aspects of the diet, such as calorie content of each macronutrient (carbohydrates, protein, and fats), as well as on the specific fatty acid composition, carbohydrates, and protein profiles. While a Western diet is considered a risk factor for male infertility, the Mediterranean diet seems to protect against male infertility; moreover, the role of a vegetarian habitus in the preservation of sperm quality is controversial. Since diet may be an important modifiable determinant of male reproductive potential, the role of daily nutrient exposure needs to be highlighted to preserve male fertility or to prevent male infertility.
- spermatozoa
- infertility
- obesity
- fatty acids
- sugar
- bioactive molecules
1. Introduction
Diet might affect male reproductive potential, even though the biochemical mechanisms involved in the modulation of sperm quality remain poorly understood.
In this context, unhealthy hypercaloric diets and excessive intake of saturated and trans fatty acids have a negative impact on sperm quality and, therefore, on the fertilization process. On the other hand, healthy dietary models are clearly associated with a better sperm quality, suggesting that nutritional intervention could have a key role in the preservation of male fertility. Moreover, an adequate intake of antioxidant molecules has been quite effective in the prevention and/or in the treatment of male infertility. Therefore, the role of daily nutrient exposure needs to be highlighted to preserve male fertility or to prevent male infertility.2. Diets and Male Fertility
In recent decades, the main dietary pattern has become the so-called “Western diet”, which is the consequence of the human lifestyle “westernization”. This diet is characterized by a high intake of industrially processed foods, rich in animal proteins, simple carbohydrates, trans and saturated fats, and poor in dietary fiber and essential unsaturated fatty acids. Recent studies have linked a Western pattern diet with increased risks of metabolic diseases, atherosclerosis, neurodegeneration, cancer, as well as for an increased risk of infertility.Differently from the Western diet, Mediterranean diet, which is one of the healthiest dietary patterns, has evident health benefits, including benefits in terms of semen quality parameters. This diet is characterized by a high consumption of legumes, cereals, fruits, vegetables, a moderate consumption of fish and wine, and a low consumption of dairy products and meat; olive oil is the main source of added fat. Thus, the Mediterranean diet is rich in monounsaturated fatty acids (MUFA), fiber, and antioxidants, and low in saturated fat (SFA).
Another dietary model, the vegetarian diet, is similar in dietary composition to the Mediterranean diet, but it does not include meat and meat products, poultry, seafood, and flesh from any other animal. Recently, there has been considerable interest in the impact of this diet on male fertility because it has been proposed that this dietary model decreased semen quality. Differential impacts of Western, Mediterranean, and Vegetarian diets on male fertility depend on the amount and quality of the nutrients introduced. 3. Western Diet as a Risk Factor for Male InfertilityOver the last several decades Western diet has been therefore a significant contributor to the growing rate of obesity, which has had a significant effect on fertility through changes in hormonal levels, sperm function, and gamete molecular composition. Obesity has been shown to disrupt various components of the hypothalamic-pituitary-gonadal axis, causing hypogonadism, which is mainly associated with reduced levels of testosterone and fewer spermatozoa.
Increased amounts of adipose tissue cause a condition of insulin resistance and have an important role in the development of oxidative stress, thus altering reproductive pathways and sperm function. Hyperinsulinemia and hyperglycemia, which are the hallmark of insulin resistance, seem to be responsible for the reduction in sperm glucose uptake and metabolism, thus having a possible role in the impairment of glycolysis in sperm cells.
Glucose uptake and homeostasis may be also modulated by leptin released from fat cells in adipose tissue depots. It has been found that hyperinsulinemia and hyperleptinemia were associated with an increase of insulin and leptin concentrations in seminal plasma, which may negatively impact male reproductive function and sperm quality.
Leptin has also an important role in the chronic pro-inflammatory state in the testicular microenvironment and/or excurrent ductal system, thus increasing the level of reactive oxygen species (ROS) which are responsible for the decrease in sperm quality.
Excess fat tissue results in increased activity of aromatase, which is an enzyme responsible for converting testosterone to estradiol. The consequent decrease in the testosterone levels results in low sperm production because this hormone is the major androgen in the testis involved in the regulation of spermatogenesis. Low testosterone levels seem to be related not only to oxidative stress but also to mitochondrial dysfunction in Leydig cells, located in the connective tissue surrounding the seminiferous tubules, where the first step of the synthesis of testosterone occurs.
It has been suggested that also dyslipidemia, which is known to be associated with increased amounts of adipose tissue, may have an impact on semen quality.4. Mediterranean Diet as a Protection Factor against Male Infertility
One reason why the Mediterranean dietary pattern is so positive for male fertility is because it provides a low level of SFA and trans fatty acids, and adequate levels of certain nutrients such as omega-3 fatty acids, antioxidant molecules and vitamins. In fact, it has been shown that intake of antioxidant vitamins and carotenoids was related to higher sperm counts. Moreover, higher intakes of fruit, cereals, and vegetables were positively related to sperm motility and concentration.
Many dietary natural compounds isolated from fruits, vegetables and edible plants can target mitochondria, modulating organelle metabolism, biogenesis, and redox status. The protection of mitochondrial function by these compounds may be important in explaining their beneficial effects on male reproductive performance.
Another characteristic of the Mediterranean diet is the consumption of olive oil as the main source of fat. It has been demonstrated in animal models that olive oil supplementation significantly increased sperm quality. This is because olive oil, which is the main source of MUFA, may modify the sperm membrane lipid composition, reducing oxidative stress damages, and restoring mitochondrial function. Moreover, the Mediterranean pattern induces a reduction of omega-6 fatty acids in favor of omega-3 fatty acids, which were associated with an improvement of sperm energetic metabolism.
5. Vegetarian Diet as Controversial Factor for Male Infertility
Existing studies have reported mostly protective associations between vegetarian pattern and risk factors for chronic diseases. However, the role of a vegetarian diet in the preservation of sperm quality is controversial.
Vegetables and fruits are rich in antioxidant molecules, which can act as sperm ROS regulators, by reducing sperm DNA damage and by increasing sperm motility and vitality. At the same time, it has been proposed that the vegetarian diet reduced sperm concentration and motility but did not extend into the infertile range. This effect may be attributed to estrogenic compounds or chemical residues in the diet which had a negative effect on sperm parameters.
6. Nutrients Impacts on Molecular Aspects Related to Sperm Quality
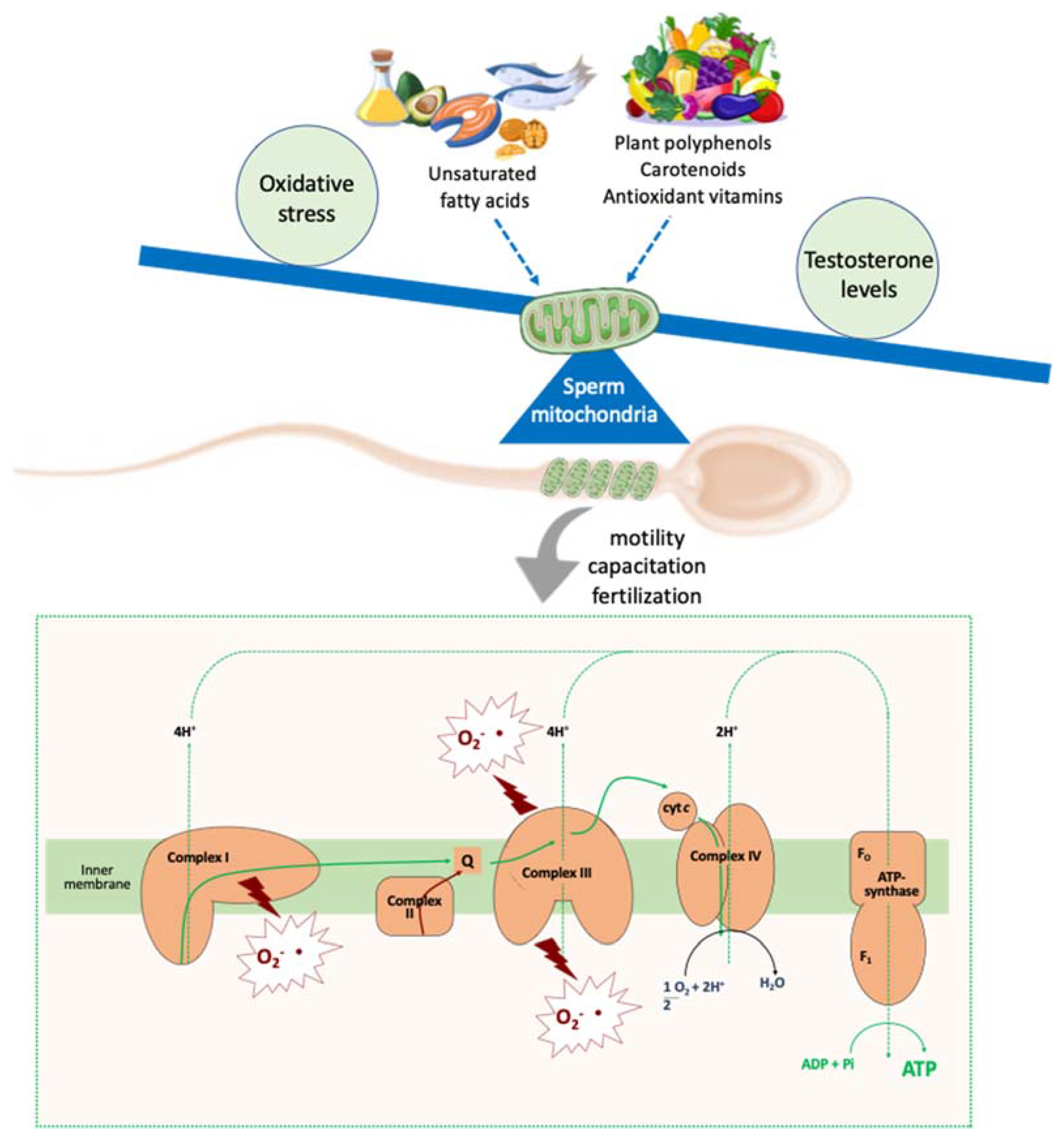
Although the picture of the complex relationship between nutrients/antioxidant molecules and sperm quality is far from complete, some indications can be drawn. First, the amount and quality of the nutrients introduced can act on sperm quality by acting on sperm energetic metabolism. Then, diets rich in SFA and low in PUFA or with an unbalanced ratio omega-6/omega-3 PUFA negatively affect sperm quality, whereas dietary unsaturated fatty acid supplementation ameliorated sperm quality. While an excess of simple carbohydrates negatively affects sperm function, there are no studies about the role of complex carbohydrates on male reproductive potential. Lastly, a low protein diet, as well as the deficiency of some specific amino acids, have been considered a potential risk factor for male-factor infertility.Fat, carbohydrates, and proteins affect sperm quality, by acting on oxidative stress and testosterone levels, whose common target are mitochondria. Mitochondria are key organelle supporting several sperm functions. Since they are involved in energy production, reactive oxygen species (ROS) homeostasis and steroid hormone biosynthesis, all molecules that can influence this crosstalk, may affect male fertility. Among these molecules, dietary fatty acids, and natural polyphenols act as modulator of sperm mitochondrial function.
In fact, the administration of PUFA, especially omega-3 PUFA, determined an increase in the activities of mitochondrial enzymes involved in gamete energetic metabolism and a reduction in oxidative damage. Moreover, many dietary natural polyphenols (mainly flavonoids) found in fruits and vegetables differentially affect (positively or negatively) mitochondrial function, depending on their concentration. Therefore, the modulation of sperm mitochondrial function could play a key role in the improvement of sperm quality (Figure 1).