Where OC is potentially curable at presentation, it is locally advanced in the majority of cases. Standard of care treatments in this setting for both OSCC and OAC are usually extensive and invasive, requiring neoadjuvant chemotherapy or chemo-radiotherapy (NAT) followed by surgical resection as recommended by NICE guidelines
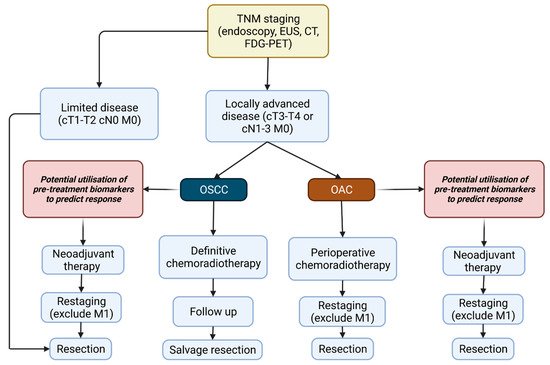
[26]. Guidance on the treatment pathway of OSCC and OAC based upon staging and functional assessment of the patient, as recommended by the European Society of Medical Oncology are outlined in
Figure 1 [27]. A variety of studies have investigated the benefits of NAT. The MRC MAGIC trial showed patients who receive a neoadjuvant regimen of epirubicin, cisplatin and 5-fluorouracil (5-FU) (ECF) therapy had a higher rate of overall survival (5-year survival, 36% vs. 23%) and progression free survival (0.53 to 0.81,
p< 0.001) in comparison to patients undergoing surgery alone
[28]. Similarly, the CROSS trial demonstrated that neoadjuvant chemoradiotherapy improved median overall survival from 24 to 49.4 months vs. surgery alone
[29]. However, only 25% to 30% of patients achieve a partial or complete pathological response
[30][31][30,31], and it carries a 0.5 to 2% mortality rate
[32]. Early identification of patients that respond well could improve outcomes by preventing the administration of treatment regimens that are unlikely to be effective and facilitating treatment modulation
[33]. Response to therapy is usually assessed via assignment of the Mandard Tumour Regression Grade (TRG) ranging 1 to 5
[34]. Responders are usually defined as TRG1 (complete regression with no viable tumour cells evident) and TRG2 (presence of residual cancer cells), at least for patients receiving chemotherapy. By administering NAT in patients who do not respond well, surgery is delayed, which if carried out earlier may have proven more effective. The main benefits of NAT are the increased chance of complete resectability of the primary tumour, as reduced tumour mass induced by NAT decreases the area of resection required, as well as improved prognostic outcome due to the decreased incidence of nodal micrometasteses
[32][35][36][32,35,36]. On the contrary, tumour progression during therapy can occur in those patients who do not respond well to NAT or conversely overtreatment of tumours with a favourable prognosis that are unlikely to respond to NAT. Therefore, identifying biomarkers that allow successful identification of who will or will not respond to therapy are desperately needed to allow rational treatment decisions to be made.