Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Francesco Bellanti and Version 3 by Dean Liu.
Malnutrition in hospitalized patients represents a heavy healthcare burden worldwide. Indeed, malnutrition in hospitalized patients worsens both prognosis and quality of life by increasing mortality, morbidity, and infection rate, extending the hospital stay, reducing the response to medical treatment, and increasing both the re-hospitalization rate and health expenditure.
- malnutrition
- hospitalized
- old
1. Definition of Malnutrition
Malnutrition is a global health problem affecting more than a billion people of any age group [1][2][6,11]. Despite its worldwide diffusion, a universal definition of malnutrition is not yet accepted, even because the definition and the diagnostic criteria for malnutrition have changed over time [3][12].
The European Society for Clinical Nutrition and Metabolism (ESPEN) defines malnutrition as “a state resulting from lack of intake or uptake of nutrition that leads to altered body composition (decreased fat-free mass) and body cell mass, leading to diminished physical and mental function and impaired clinical outcome from disease” [4][13]. The American Society of Parenteral and Enteral Nutrition (ASPEN) and the Academy of Nutrition and Dietetics (Academy) suggest etiologic-based definitions that consider both time and degree of inflammatory response in acute or chronic illness/injury [5][14]. Considering its clinical and pathophysiological heterogeneity, the term “malnutrition” includes three major groups of conditions: (1) undernutrition, which includes stunting (low height-for-age), underweight (low weight-for-age), and wasting (low weight-for-height); (2) micronutrient-related malnutrition, which includes micronutrient excess or deficiencies (lack of important vitamins and minerals); (3) overnutrition, overweight, obesity, and diet-related non-communicable diseases (such as stroke, heart disease, diabetes, and cancer) [6][15].
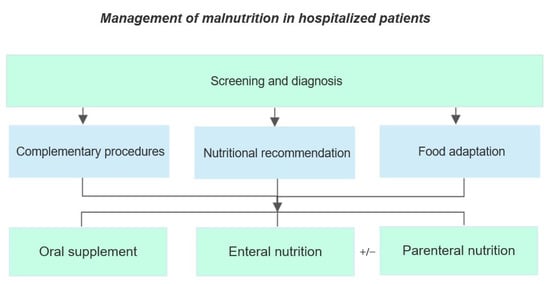
23. Screening and Assessment of Malnutrition in the Acute Setting
Malnutrition in a hospital setting is a costly, morbid, potentially preventable, and treatable issue. Even though malnutrition is a well-known determinant of several serious complications, hospitalized patients are not regularly screened for nutritional status at hospital admission and are seldom diagnosed if malnutrition occurs during hospital stay [7][8][2,20]. Nutritional screening tools in a hospital setting should be easy and quick to use, validated and suitable to be applied for bedside assessment, and highly effective in identifying individuals at risk of malnutrition [9][10][21,22]. The Nutrition Risk screening-2002 (NRS-2002) is one of the nutritional screening tools recommended by ESPEN. NRS-2000 was validated in adult inpatients and considers weight loss, weekly reduction of food intake, worsening of general conditions, disease severity, and age. Low risk of malnutrition is defined by a score <3, while patients with a score ≥3 are considered at medium/high risk of malnutrition. This tool was created to identify patients who should benefit of a nutritional intervention [7][1][11][12][2,6,17,23]. The malnutrition universal screening tool (MUST) is a further useful tool included in the ESPEN guidelines, validated in adult patients, and recommended in hospital, community, and other care settings. The MUST score includes three clinical parameters: weight loss, BMI, and reduction of food-intake for at least five days. Patients are defined at low risk of malnutrition if score is 0 and at medium risk if score is 1, while a score of 3 defines malnutrition [7][1][11][2,6,17]. In older people, ESPEN recommends using the Mini Nutritional Assessment (MNA) either in its full or short form (MNA-SF). MNA-SF is a valid alterative to MNA in hospitalized elderly patients. It evaluates 6 items from MNA: (1) reduction of food intake in the previous three months, (2) mobility, (3) acute disease or psychological stress, (4) neuropsychological problems, and (5) BMI or (6) calf circumference (CC). This tool identifies three categories of patients: those with a preserved nutritional status; those at risk of malnutrition, and those who are malnourished. The MNA is a moderately validated tool, not suitable for old patients that suffer from a severe cognitive decline [7][1][11][2,6,17].
In order to diagnose malnutrition, a 2-step approach has been recently recommended by the Global Leadership Initiative on Malnutrition (GLIM) in hospitalized patients: the first step consists of a screening within 24–48 h after hospitalization to identify subjects at risk of malnutrition using any validated screening tool; the second step includes the assessment for diagnosis and grading of severity in high-risk patients. Moreover, GLIM recommends to re-assess the nutritional status periodically during hospitalization [2][11].
A comparison among three nutritional screening tools (MUST, SGA and NRS-2002) in old hospitalized patients showed that MUST is the most sensitive, specific, and accurate to identify malnourished patients according to the new GLIM criteria for Malnutrition, despite being less rapid as compared to NRS-2002 and SGA [7][2]. Other validated nutritional screening tools include the Malnutrition Screening Tool (MST), which assesses weight loss and the decrease in food intake, and the Short Nutritional Assessment Questionnaire (SNAQ), which evaluates weight loss, appetite decrease, and the use of nutritional supplements (in the form of drinks or feeding tubes). Both nutritional screening tools are moderately validated and indicated for adult inpatients [1][11][6,17].
Nutritional screening should be included in a defined clinical protocol, followed by concrete interventions when needed [13][24]. A positive screening of malnutrition is followed by the assessment of the nutritional status. Indeed, this evaluation is performed if a patient is classified as at risk by a validated screening tool and by the assessment according to the new GLIM diagnostic criteria [7][2][14][2,11,19].
32. Epidemiology of Hospital Malnutrition
32.1. Prevalence of Malnutrition in Hospital Setting
Malnutrition affects all stages of life, from children to old individuals, but prevalence differs depending on factors such as age, geography, social condition, or the presence of specific situations such as edentulia [1][15][6,25]. Nutritional status in hospitalized patients widely depends on the setting of care [16][26]. Indeed, the prevalence of malnutrition grows with the intensity care level, as shown in Figure 1 [17][27].
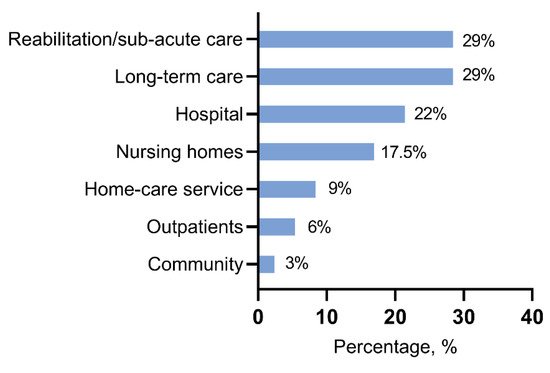
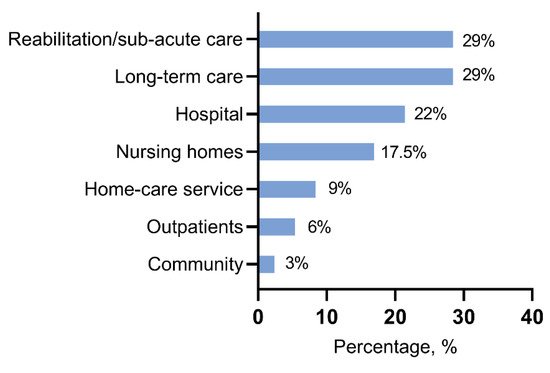
According to most studies, malnutrition prevalence in hospitalized patients ranges from 20% to 50%, according to the use of different diagnostic criteria and screening tools [7][18][2,7]. Among geriatric patients, the rate of poor nutritional status is higher as compared to younger, with a prevalence of up to 90% [18][19][7,28]. In our recenthe work, researcherswe found a prevalence of malnutrition of 46% among hospitalized old patients evaluated by the new GLIM diagnostic criteria [7][2]. In a recent prospective study on geriatric patients, malnutrition and risk of malnutrition were extremely prevalent between acutely ill medical patients, from admission to the Emergency Department up to four weeks after discharge [20][29]. Interestingly, hospitalized old patients do not show agreement between self-perceived and objective nutritional status [21][30].
32.2. Risk of Malnutrition during Hospitalization
About 60–65% of hospitalized patients experience a poorer nutritional status as compared to healthy individuals [22][23][31,32]. Indeed, hospitalization is associated with important changes in regular nutritional intake because of several factors, such as restricted timing of food provision, decreased appetite, adverse effects of medication, and prescribed periods of fasting [24][33]. A previous study demonstrated that, despite a protein provision of 1.0 g/Kg/day, the effective protein intake during hospitalization was lower in terms of reduced intake in both provided food and oral nutritional supplements [24][33]. Poor appetite, hospital meal refusal, and operation-related fasting are the most frequent causes of avoidable hospital-acquired malnutrition (HAM) [25][34]. Indeed, evidence indicates how the risk of malnutrition is higher when evaluated during hospitalization than assessed at hospital admission [26][35]. A prospective observational study demonstrated that decline in nutritional status and weight loss were significantly associated with protracted length of stay (LOS), independently of demographic features and disease severity [27][36]. On the other hand, malnutrition exerts a negative impact on LOS and several other clinical and economic outcomes [27][28][36,37]. A recent retrospective study reported a 1% incidence of malnutrition during hospitalization longer than 14 days [29][38]. Furthermore, HAM was significantly associated with extended LOS, cognitive impairment, pressure wound, or fall during hospital stay [29][38].
32.3. Risk Factors for Malnutrition in Hospitalized Patients
Several risk factors are described as associated with malnutrition in hospitalized patients [20][29]. Generally, these risk factors can be classified into two main groups: individual (physical and social) and organizational [30][39]. Old age, comorbidities, and polypharmacy are the most important physical risk factors for malnutrition [20][30][29,39].
Aging is associated with a higher risk of malnutrition because of several age-related changes able to affect nutritional statuses, such as deficit of physical activity, poor appetite, the feeling of unwantedness, or a sense of neglect. Furthermore, old age is characterized by a loss of taste, which can impact eating habits with negative consequences on health status [31][40]. Other important changes involve loss of bone density or skeletal muscle mass, with gain in body fat that can lead to osteoporosis, sarcopenia, or sarcopenic obesity [15][32][25,41]. In this scenario, malnourished old patients show a high risk of developing geriatric syndrome as compared to well-nourished, resulting in significant impairment of health status [33][42]. Cancer is highly associated with malnutrition in hospitalized patients. Malnutrition in cancer patients may depend on several mechanisms, including the tumor type, disease stage, side effects related to the treatment, and inadequate nutritional therapy [34][35][43,44]. Moreover, heart failure or diabetes mellitus are common diseases with a high prevalence of malnutrition and higher in-hospital mortality rates [36][37][38][39][45,46,47,48]. Polypharmacy is associated with malnutrition, especially proton pump inhibitors, anti-constipation, and antihypertensive drugs [40][49]. Malnutrition and polypharmacy are tightly related since an impairment of nutritional status induces the use of higher drug doses, creating a vicious cycle. Drugs can affect nutritional status through various mechanisms such as reduced appetite, decreased nutrient absorption, or adverse reactions [22][40][31,49].
Female sex is also associated with a higher risk of malnutrition due to several factors such as longer life expectancies than men or a higher probability to suffer from adverse economic and social circumstances in old age [41][50].
Low adherence to a Mediterranean diet is an important predictor of malnutrition in old patients [42][43][51,52].
Further factors include depression, low functional capacity, cognitive impairment, dysphagia, and eating-related problems [20][44][29,53]. Overall, the prevalence of eating difficulties during hospitalization was found to involve 46% of patients [45][54]. An important role in the risk of malnutrition is played by social factors such as low educational level and living alone [44][53]. In old patients, loneliness is recognized as an independent factor associated with poor nutritional status. Old people show a greater risk of reduced social relationships, isolation at home, and fewer opportunities to socialize with other people [46][47][55,56]. Nutritional status is further affected by marital status since unmarried subjects present with a higher risk of malnutrition [48][49][57,58].
Alcohol abuse, tobacco use, or socio-economic status are common independent risk factors of malnutrition [30][34][50][51][39,43,59,60]. Organizational factors play an important role in enhancing the risk of malnutrition, especially in hospitalized patients. Indeed, hospitalization is a risk factor itself for malnutrition [4][30][13,39]. Inadequate meal service, limited food choice, insufficient time to consume meals, and need to help for meal assumption are some of the principal risk factors to promote the decline in nutritional status during hospitalization [4][13]. Furthermore, malnutrition often remains unrecognized because nutrition screening is frequently underperformed in hospitalized patients [4][19][13,28]. In a European-wide survey, data show how only half of the hospital units reported routine use of nutrition screening [23][32].