Tuberculosis (TB) is a bacterial infection with Mycobacterium tuberculosis. It is a public health problem worldwide and one of the leading causes of mortality. Clinical manifestations and routine laboratory tests have limitations in directing physicians to diagnose TB. Medical imaging examinations play an essential role in detecting tissue abnormalities and suspecting diagnosis of TB. Radiologists and Physicians should be familiar with the radiological manifestations of TB to contribute to the early suspicion and diagnosis. This aentrticley illustrates the common radiological patterns of pulmonary and extrapulmonary TB.
- miliary tuberculosis
- tree-in-bud pattern
- tuberculomas
- tuberculous lymphadenitis
- cavitary lesions
- tuberculous spondylitis
- tuberculosus pericarditis
- tuberculous peritonitis
- tuberculous leptomeningitis
- tuberculous abscess
1. Introduction:
1. Introduction
Tuberculosis (TB) is a bacterial infection with Mycobacterium tuberculosis. TB is considered to be a public health problem and a leading cause of death worldwide [1,2][1][2]. In 2020, the COVID-19 pandemic created unprecedented health challenges and replaced TB as the first deadly infectious disease, thus disrupting the TB health services, especially in high-burden countries [2]. It is estimated that 30% of the world’s population is infected with TB [3]. Typically, infection occurs through prolonged or repeated exposure to Mycobacterium tuberculosis transmitted by airborne droplets from the coughs or sneezes of an actively infected person. The lung is the most common site of TB infection; however, it can involve any other organ in the body [1,3][1][3]. Approximately 90% of exposed individuals carry the bacteria but harbor the infection at a subclinical level with no clinical, radiological, or microbiological manifestations, a condition known as latent infection. Nearly 5% of infected patients develop active infection within the first two years; this category is called primary TB. The remaining 5% of infected individuals with effective immunity can control the primary infection, but viable mycobacteria remain dormant and reactivate; this is known as post-primary or reactivated TB [3,4][3][4].
The lungs are the primary affected organs; however, hematogenous dissemination from latent pulmonary focus can occur in other organs in the body, thus forming extrapulmonary TB. It causes destructive changes in the affected organs due to caseous granulomas, which are formed from the development of cell-mediated hypersensitivity. This process of infection can be confused with many benign or malignant neoplasms [5].
Clinical manifestations of TB include night fever and sweating, unexplained weight loss, loss of appetite, and fatigue. A persistent cough, with or without hematemesis; breathlessness; and chest pain when breathing are additional manifestations in highly contagious patients with pulmonary TB. However, clinical manifestations vary in extrapulmonary TB according to the infected organs; therefore, the diagnosis of extrapulmonary TB requires a high index of suspicion and further laboratory and radiological investigations [4,5][4][5]. The diagnosis of TB requires several tests to be performed. The smear test and culture of Mycobacterium tuberculosis are the gold-standard tests. However, they are expensive and deliver a late diagnosis. Latent TB can be diagnosed by using a tuberculin skin test or an interferon-gamma release assay, which have no role in the diagnosis of active TB. In active TB, nucleic acid amplification tests (NAATs) include DNA extraction and polymerase chain reaction (PCR) amplification; the new molecular diagnostic test Xpert mycobacterium tuberculosis/rifampicin resistance (Xpert MTB/RIF) assay, which can detect the Mycobacterium tuberculosis complex within two hours, and the histopathological examination of biopsy samples and medical imaging are required for evaluation. Recently, Lipoarabinomannan (LAM) has been suggested as a biomarker to diagnose TB based on its identification in urine [6,7][6][7]. In particular, extrapulmonary TB is an important cause of nonspecific clinical manifestations, such as a fever of unknown origin (FUO) in TB-burden regions. However, medical-imaging tests play an essential role in detecting tissue abnormalities and the early suspected diagnosis of TB in different parts of the body [8].
Due to the significant role of medical imaging in the diagnosis of TB, we introduce this radiological pictorial review to elucidate the common various radiological patterns of pulmonary and extrapulmonary TB. This study discusses the most common differencing patterns of TB with radiological images and analyzes the possible differential diagnoses in various body systems. This review will be significant for radiologists, chest physicians, and infectious disease doctors who are interested in diagnosing TB.
2. Discussion
Medical imaging plays a leading role in the detection of tissue changes and primary suspected diagnosis of TB. All of the conventional radiography, computed tomography (CT), ultrasonography, magnetic resonance imaging (MRI), and positron emission tomography CT (PET-CT) methods have a role in the diagnosis of TB and can assist the physicians in their diagnosis of a wide range of diseases in different parts of the body. Various types of TB, namely pulmonary, abdominal, scrotal, brain and spine, and musculoskeletal (MSK), can be diagnosed via a wide range of medical imaging modalities [9,10][9][10]. Here, we discuss the common radiological features of TB in the chest, the central nervous system (CNS), the abdomen, and the MSK using the most appropriate imaging modalities.
2.1. Pulmonary TB:
2.1. Pulmonary TB
Lungs are the most common organ affected and they are often the initial sites of TB infection [11]. Pulmonary TB can be divided into primary and postprimary (reactivation), each with appropriate radiological features that are overlap considerably. It can involve the lung and extrapulmonary organs in the chest, such as pleura or lymph nodes [12,13][12][13] (Figures 1-11).
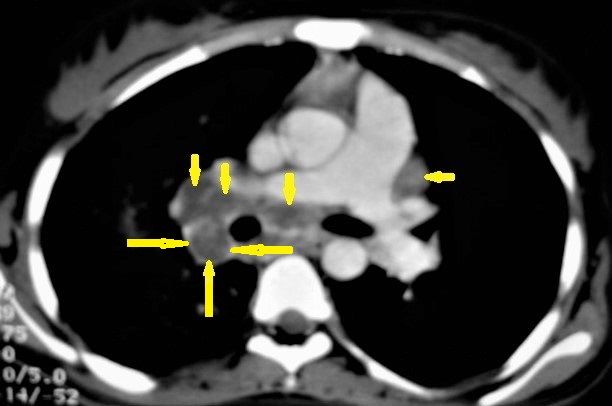
Figure 1. Primary TB in an 18-year-old man. Axial mediastinal-window CT image shows multiple enlarged mediastinal lymph nodes (short arrows), and right hilar lymph nodes are characterized by central low density and peripheral enhancement after contrast administration forming the rim sign (long arrows).
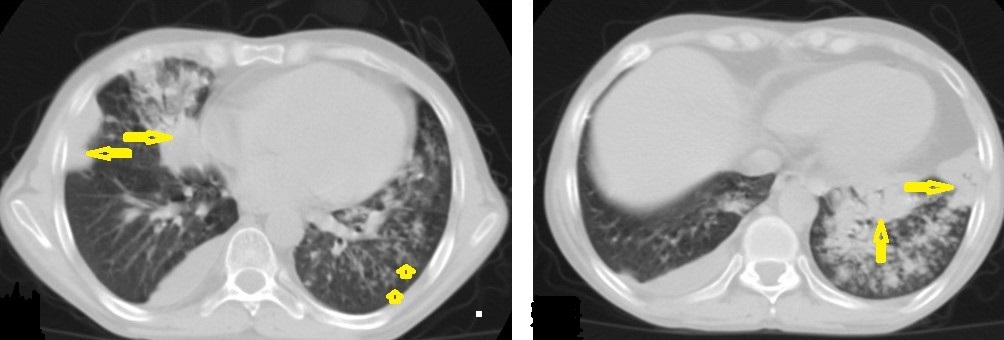
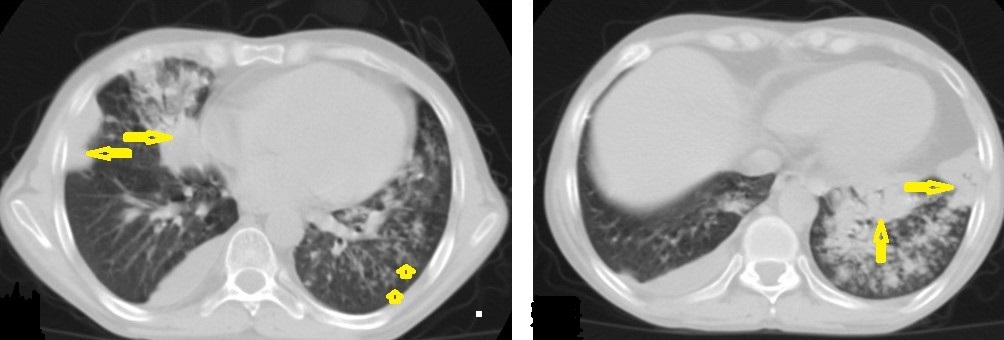
Figure 2. Active TB in a 27-year-old man with extensive endobronchial spread. Selected axial images of chest CT show extensive endobronchial spread characterized by patchy consolidations (long arrows) in the right middle and left lower lobes with tree-in-bud nodules (short arrow) more involved the left lung. Mild right pleural effusion and mild pericardial effusion appear in both images.
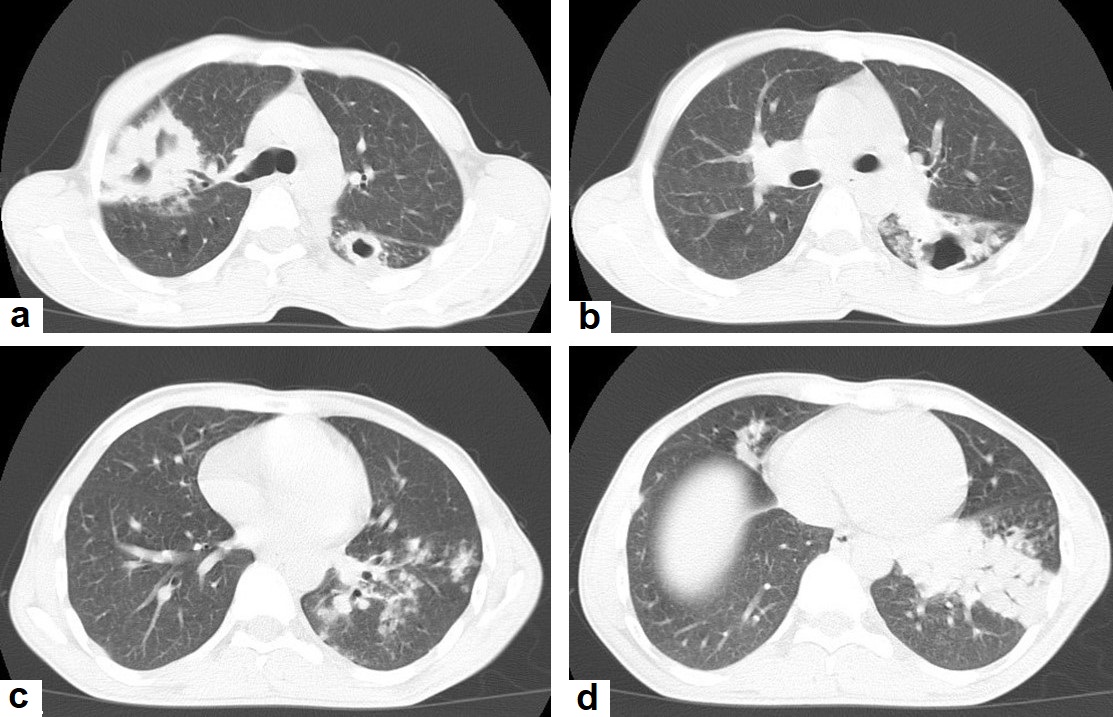
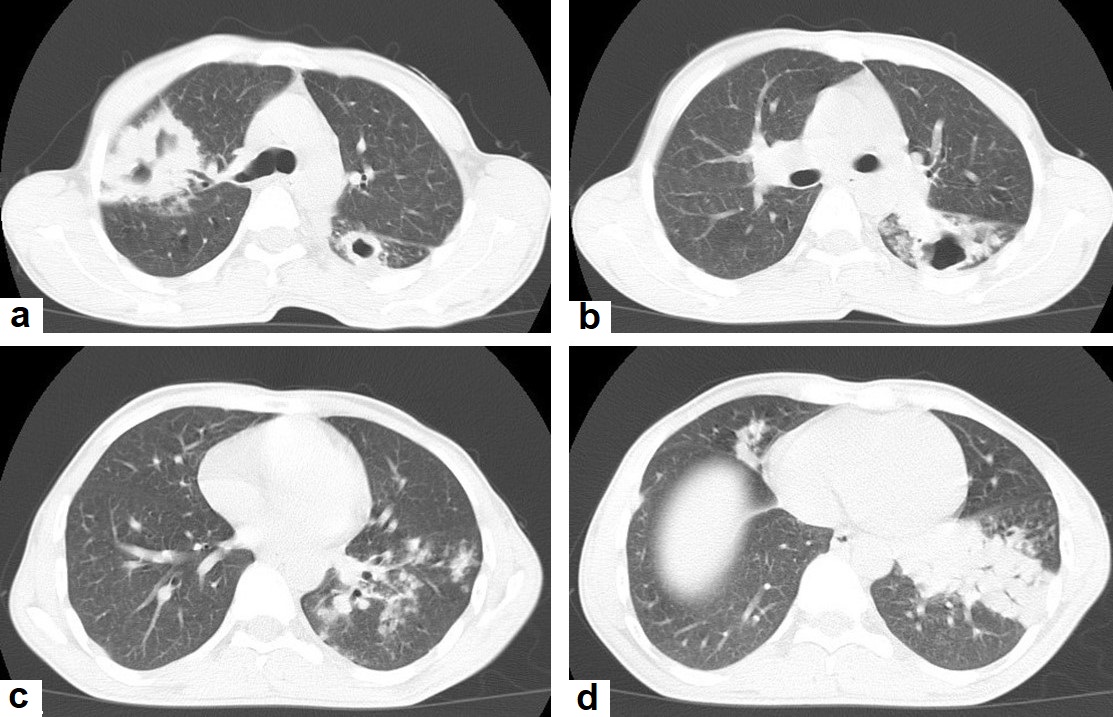
Figure 3. Post primary TB in a 45-year-old male with cough and hemoptysis. Axial images of chest CT show (a) cavitary lesions in the right upper lobe and upper segment of the left lower lobe surrounded with consolidation, (b) cavitary lesion in the upper segment of the left lower lobe with thick irregular wall surrounded by patchy ground glass opacities, (c) centrilobular nodules and tree-in-bud nodules, and (d) consolidation in the left lower lobe with air-bronchograms.
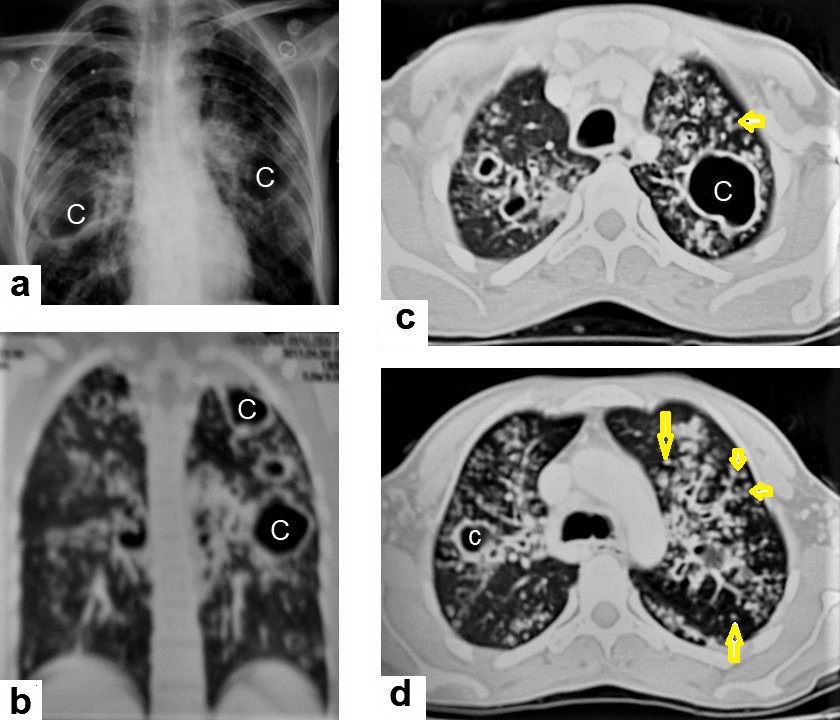
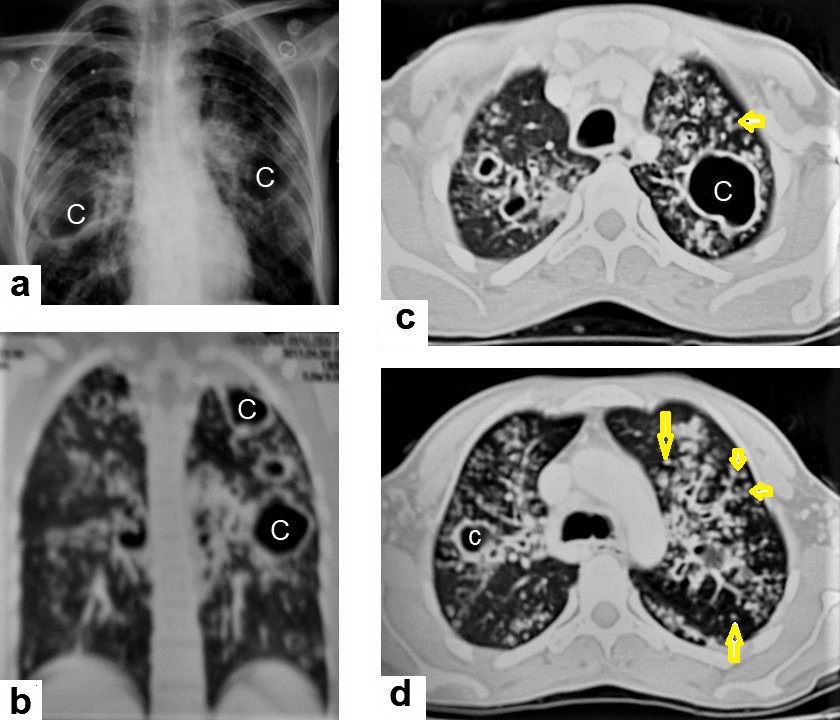
Figure 4. Reactivated TB in a 34-year-old women. (a) Chest radiograph shows extensive reticular shadowing and multiple cavitary lesions in both lungs. (b) Coronal reconstruction CT shows multiple cavitary lesions [c] in both lungs, the large two in the posterior segment of the upper lobe, and in the apical segment of the lower lobe of the left lung. (c,d) Axial CT images of the lung show multiple cavitary lesion, the largest in the posterior segment of the left upper lobe, with multiple centrilobular (long arrows) and tree-in-bud (short arrows) appearance.
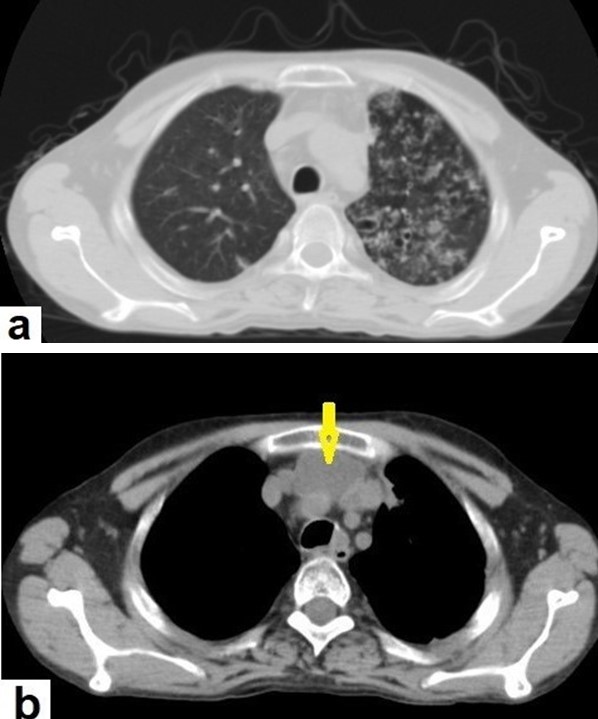
Figure 5. Active TB in a 27-year-old man (same case of Figure 2) with endobronchial spread. (a) Axial image of chest CT shows endobronchial spread characterized centrilobular and tree-in-bud nodules involved the upper lobe of the left lung. (b) CT axial image with mediastinal window shows large necrotic mediastinal lymph node measures 21 × 20 mm (arrow) in the anterior mediastinum.
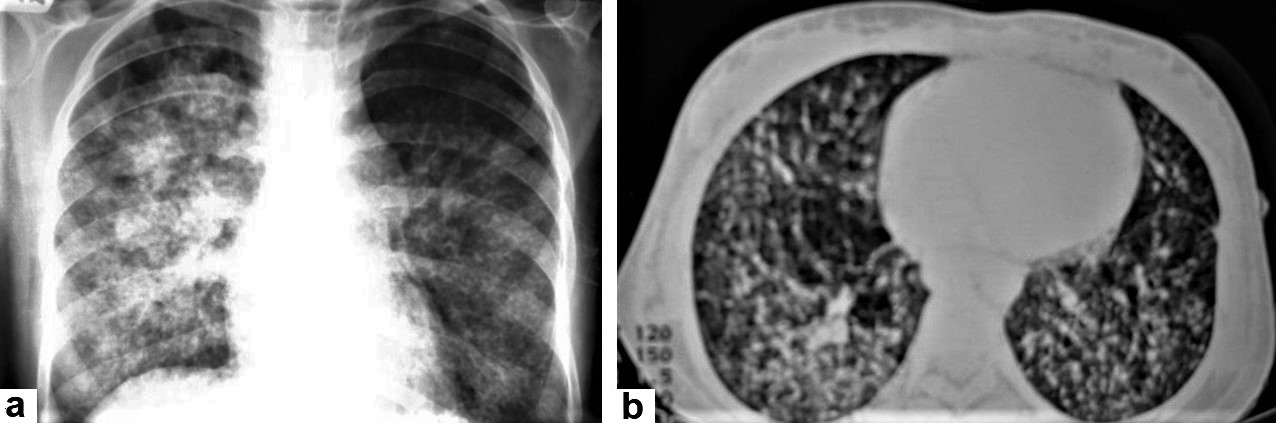
Figure 6. Miliary TB in an 18-year-old man (same patient of Figure 1). (a) Chest radiograph shows superimposed innumerable small nodules in lungs right greater than the left predominantly affecting lung bases due to gravity-dependent high blood flow. (b) Axial chest CT shows innumerable small (1–3 mm) nodules with random distribution in both lung fields.
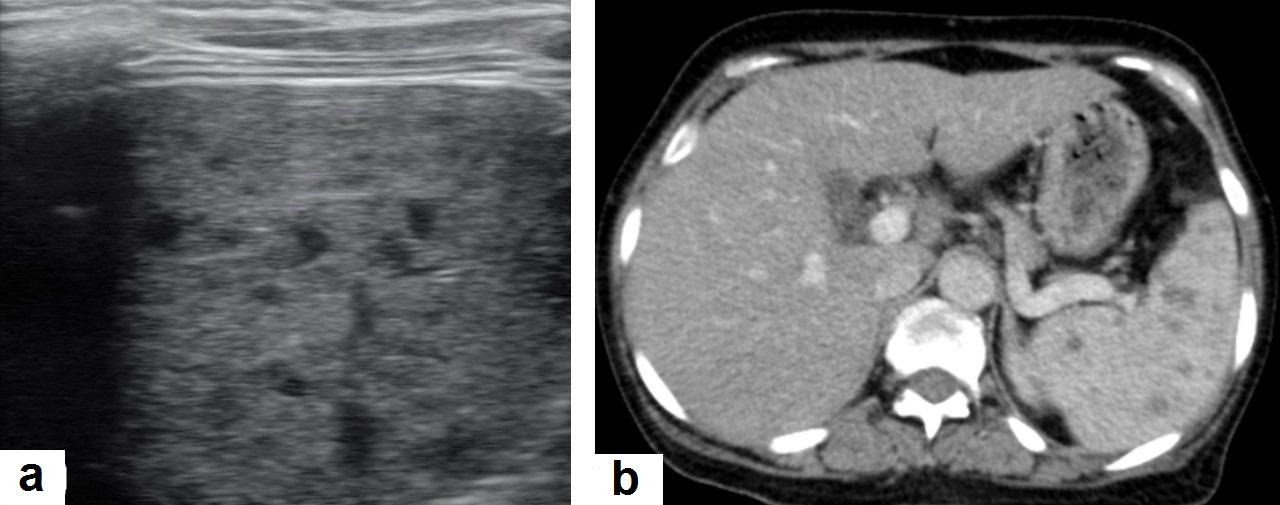
Figure 7. Miliary TB in an adult female with fatigue and loss of appetite. (a) Splenic ultrasonography shows multiple small hypoechoic granulomas with random distribution in the spleen. (b) Axial abdominal CT shows small non-enhancing granulomas with random distribution in the spleen clearly seen during the portal venous phase with multiple enlarged lymph nodes around the portal vein.
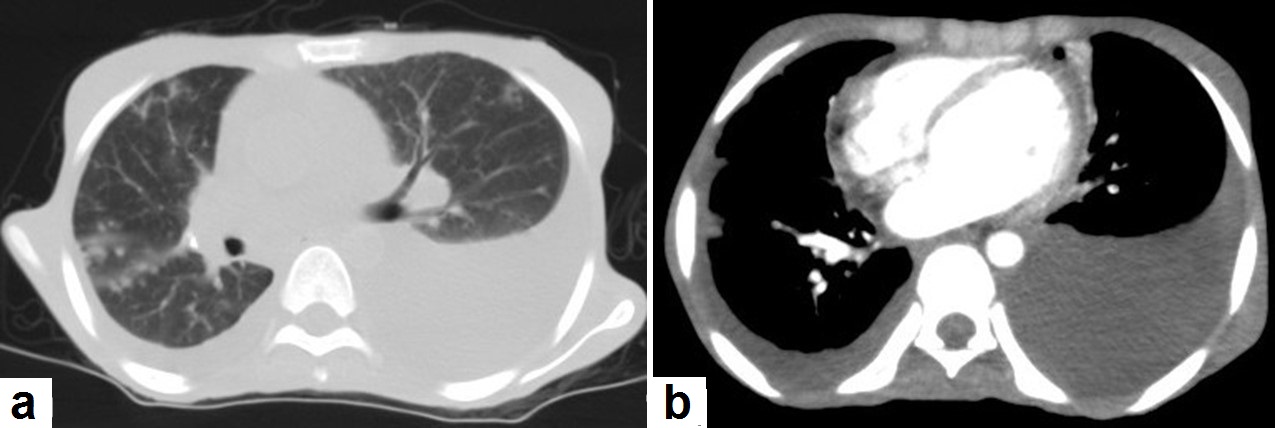
Figure 8. Active TB in a 27-year-old man (same case of Figures 2 and 5). (a) Axial image of chest CT shows moderate left and mild right pleural effusion with discrete pulmonary nodules in active TB. (b) Axial image of the mediastinal window shows moderate left and mild right pleural effusion with mild pericardial effusion.
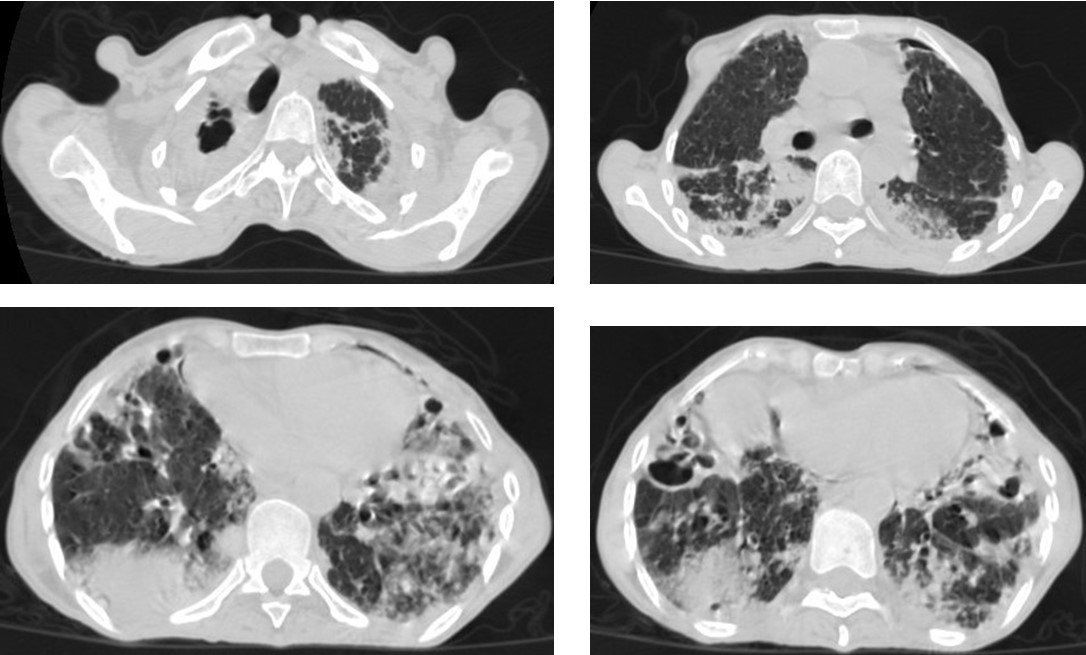
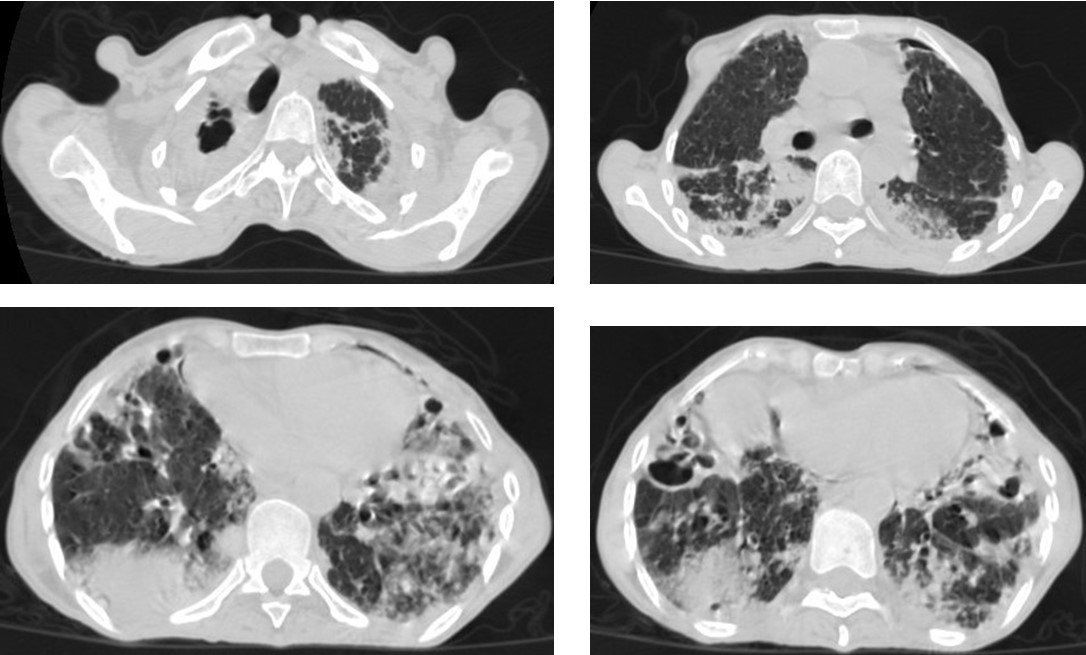
Figure 9. Old reactive TB with superimposed infection in a 75-year-old female with chronic cough and no history of previous medication. Selected axial images of lung CT show prominent fibrotic changes with scarring traction bronchiectasis and decreased volume in the apical and posterior segment of the upper lobes and architectural distortion of the lung parenchyma caused by cystic bronchiectasis predominantly involve bilateral lower lobes, ligula, and right middle lobe. Patchy consolidative areas and ground glass opacities are signs of active infection.
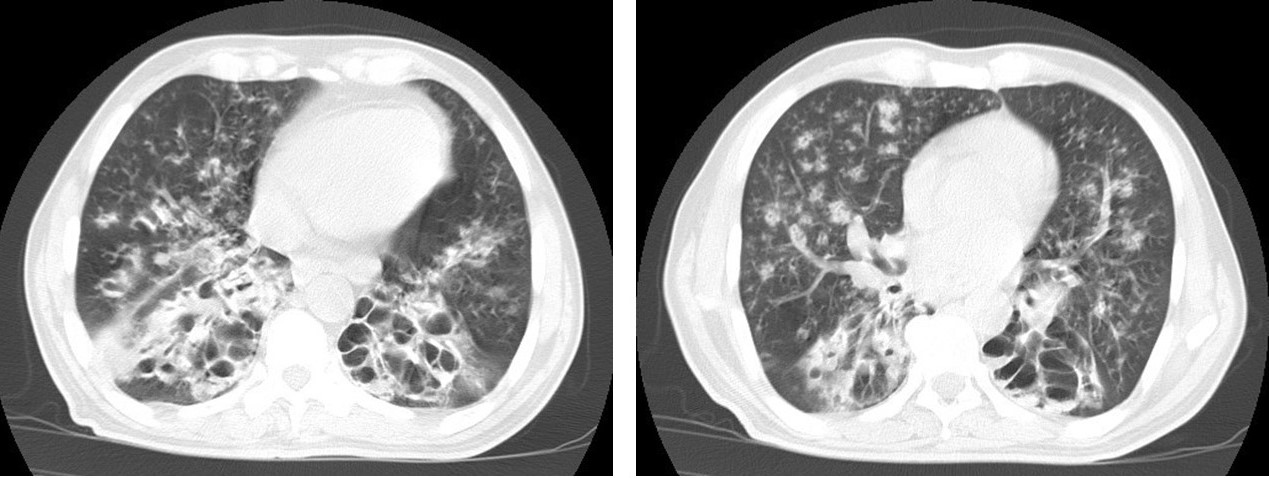
Figure 10. Reactivation of TB in an adult man with chronic cough. Selected axial images of lung CT show cystic bronchiectasis, due to old infection, with peribronchial thickening and air fluid level involving both lower lobes. Scattered tree in bud pattern and infected cystic bronchiectasis indicate active TB.
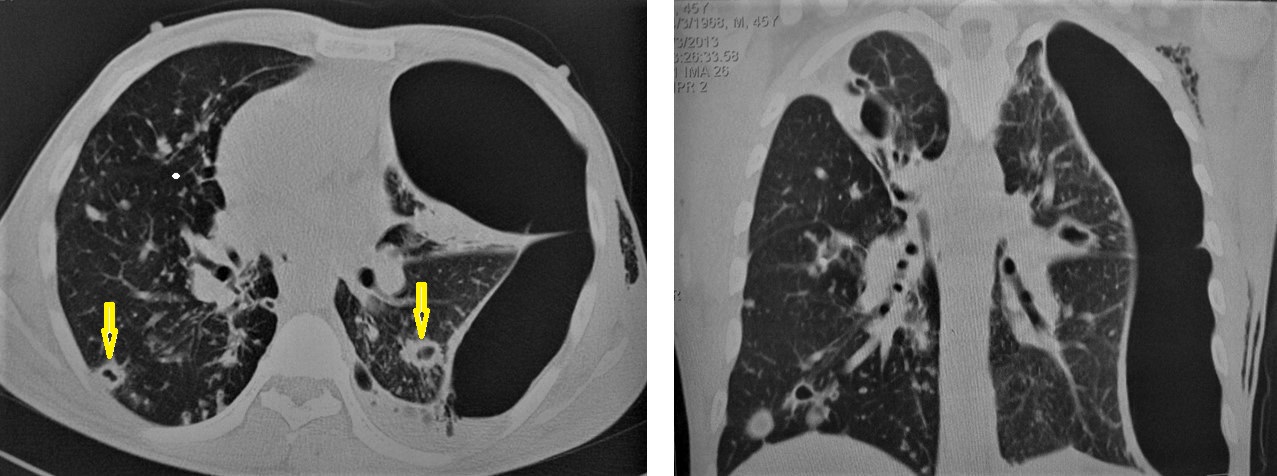
Figure 11. Post-primary-TB in a 45-year-old man. Selected axial and coronal reconstruction images of chest CT show multiple thick-walled cavitary lesions (arrows) in both lungs, with left pneumothorax as a complication of TB. Surgical emphysema in the left chest wall, due to chest-tube insertion.
2.2. Central Nervous System (CNS):
2.2. Central Nervous System (CNS)
TB can involve the CNS in 10% of cases, and it is the most devastating form of systemic TB, due to its serious neurological complications and sequelae, with high mortality rate [14,15][14][15]. In the majority of cases, infection comes via hematogenous spread from a pulmonary focus and is rarely via a direct spread from paranasal sinuses, mastoids, or orbit. It can present in various clinical conditions with clinical manifestations that are similar to other diseases, including bacterial meningitis, intracranial hemorrhage, and primary or secondary neoplasms. In addition to the rarity and unfamiliarity, the diagnosis of extrapulmonary TB is difficult. However, radiological patterns can be identified well by using an MRI, which plays a crucial role in the suggested diagnosis of TB [14,16]. It can affect leptomeninges (pia matter and arachnoid), causing tuberculous leptomeningits or pachymeninges (dura matter), thus resulting in pachymeningitis [15,16][15][16]. TB can affect the brain parenchyma, causing tuberculoma, miliary tuberculomas, cerebritis or abscesses. Moreover, it can affect the spinal cord, causing spinal tuberculoma, tuberculous myelitis, arachnoiditis, or spondylodiscitis (Potts disease) [17][17] (Figures 12-19).
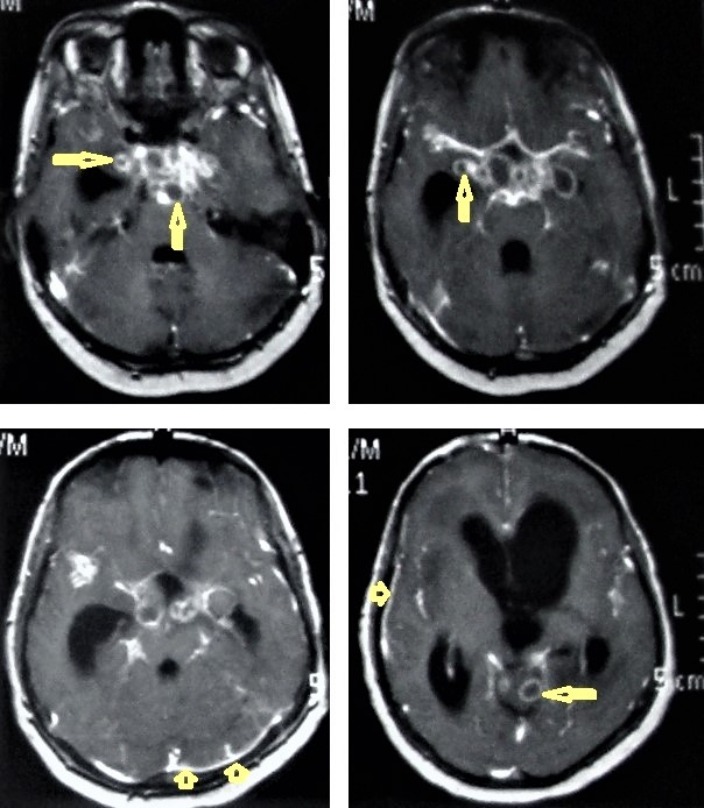
Figure 12. Tuberculous leptomeningitis. Selected axial T1-weighted images of brain MRI post-contrast administration show diffuse leptomeningeal enhancement (short arrows) with predilection to involve the basal cisterns complicated with hydrocephalus. Multiple ring-enhancing lesions (long arrows) in different regions of the brain.
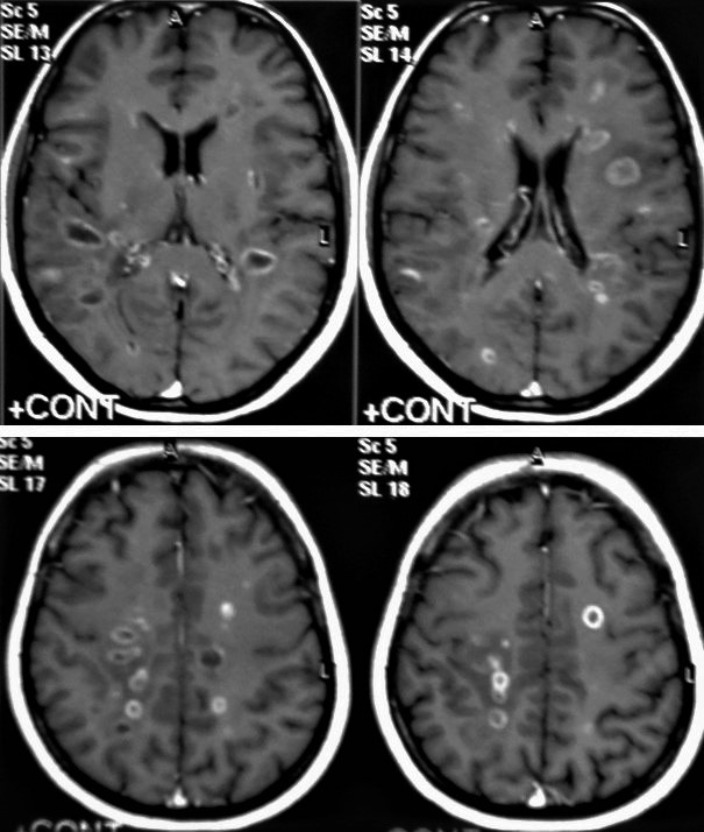
Figure 13. Multiple tuberculomas in an adult man. Selected MRI axial images post-contrast T1-weighted images show multiple small ring-enhancing lesions distributed in both cerebral hemispheres, with no significant surrounding cerebral edema, as is consistent with cerebral tuberculomas.
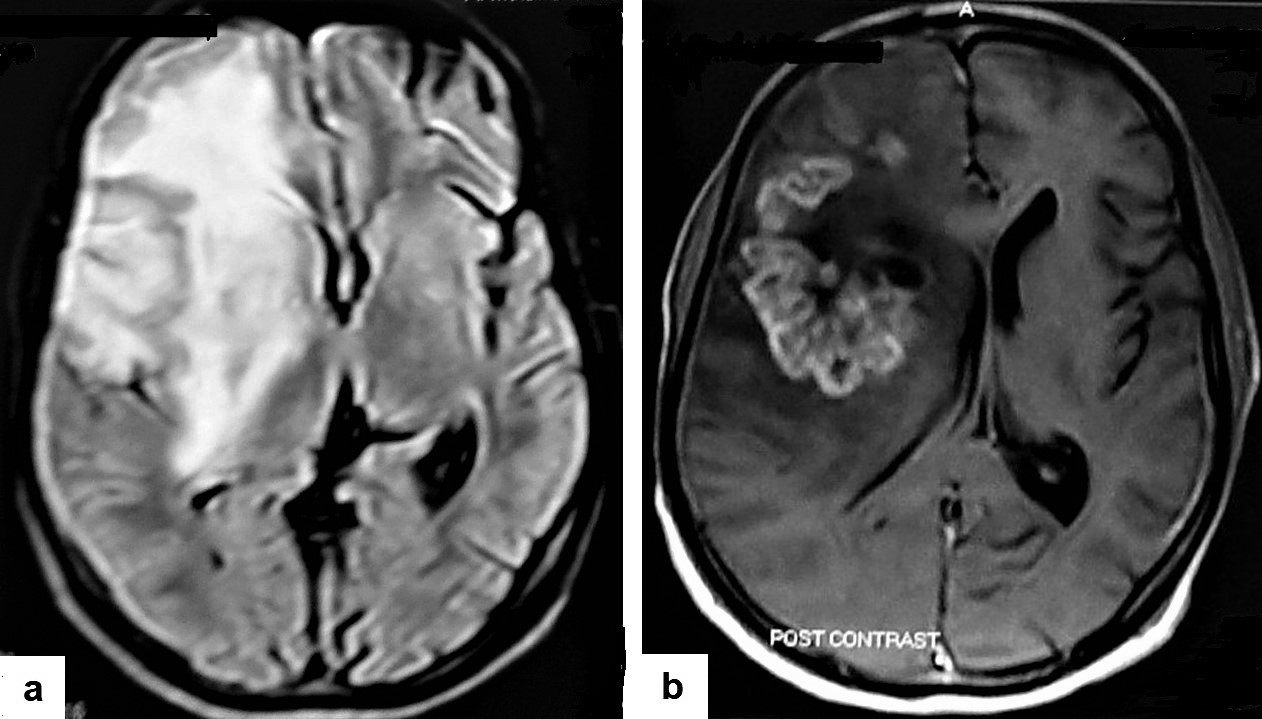
Figure 14. Tuberculous cerebritis in an adult man with fever and seizures. (a) Axial FLAIR-weighted images of brain MRI show high signal intensity in the right parietal and frontal lobes causing mass effect compressing the right lateral ventricle with mild shifting of the midline to the contralateral side. (b) Axial brain T1-weighted images post-contrast administration show intense serpentine (gyriform) enhancement in the right parietal and frontal lobes, with significant surrounding edema, suggesting tuberculous cerebritis.


Figure 15. Tuberculous abscesses and tuberculomas in a 70-year-old woman with disturbance of consciousness and long history of headache. Selected axial computed tomography (CT) images of the brain (a) axial non-enhanced CT show significant vasogenic edema in the frontal and parietal lobes of the right cerebral hemisphere, with severe mass effect manifested as loss of the cortical sulci, total effacement of the right lateral ventricle and mild midline shift to the left side. (b) Contrast-enhanced CT (CECT) shows loculated rim-enhancing lesion centered in the right frontal lobe measures about 39 × 16 × 12 mm, suggesting cerebral abscess (arrows). (c) Axial CECT shows multiple ring-enhancing lesions in the right cerebral hemispheres and right basal ganglia (short arrows) suggesting of cerebral abscesses or tuberculomas. (d) Coronal CECT shows multiple ring-enhancing lesions in the right cerebral hemispheres (short arrows), suggesting cerebral tuberculomas or abscesses.
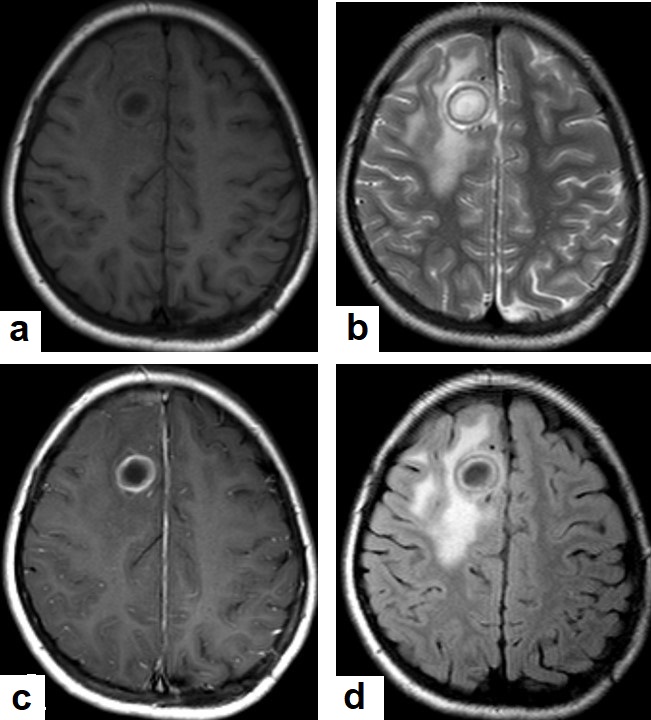
Figure 16. Tuberculous abscess in the right cerebrum of a 13-year-old female. Selected images of brain MRI (a) T1-weighted image (WI), (b) T2-WIs, (c) T1-WI with contrast, and (d) FLAIR-WI. The images show a well-defined lesion in the right cerebral hemisphere with low-signal-intensity content and a high-signal-intensity capsule on T1WI, which appear as high-signal-intensity content and a low-signal-intensity capsule on T2WI (b); there is marginal enhancement on T1WI with contrast administration (c), and there are low-signal-intensity contents and a high-signal-intensity capsule on FLAIR (d). Obvious grade-2 vasogenic oedema around the lesion on T2WI and FLAIR.
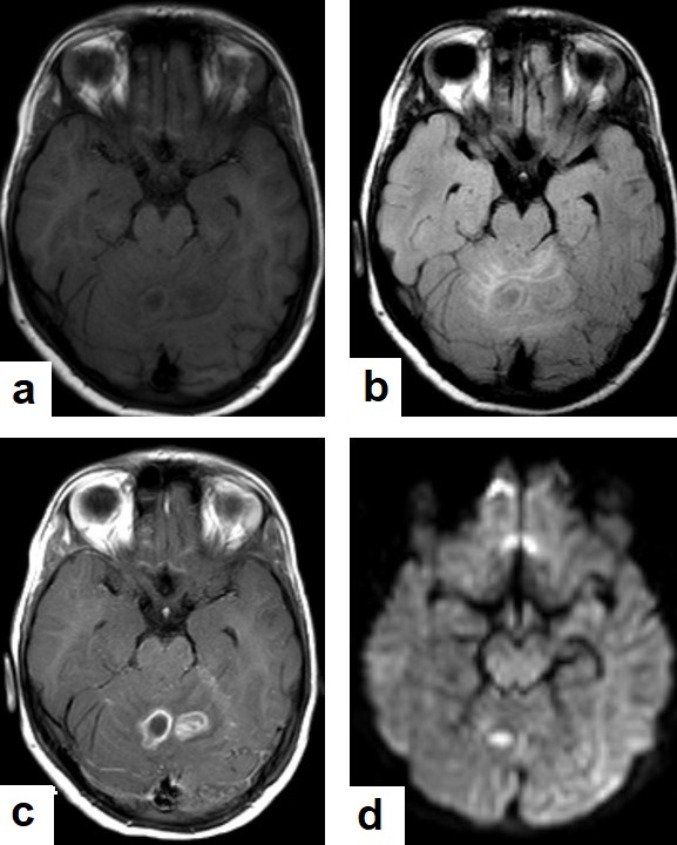
Figure 17. A tuberculous abscess in the cerebellum of a 13-year-old female (same patient as Figure 16). Selected images of brain MRI (a) T1-weighted image (WI), (b) FLAIR-WIs, (c) T1-WI with contrast, and (d) diffusion-weighted (DW) image. The images show a well-defined lesion in the cerebellum with low signal intensity content and a high signal intensity capsule on T1WI and FLAIR (b), marginal enhancement on T1WI with contrast administration (c), and restricted diffusion on DWI (d).
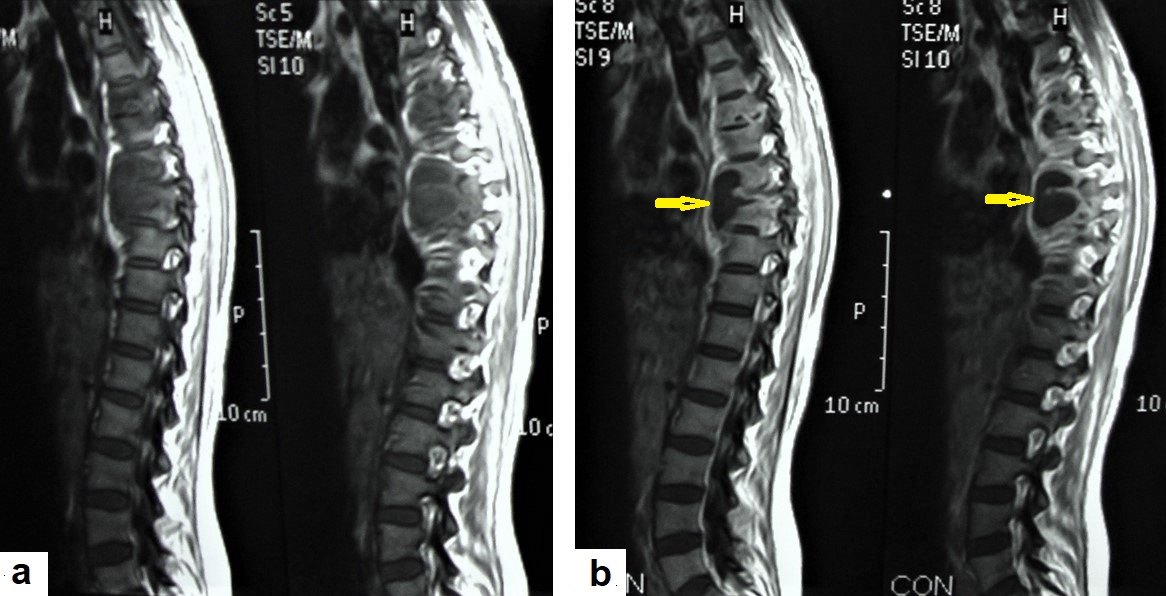
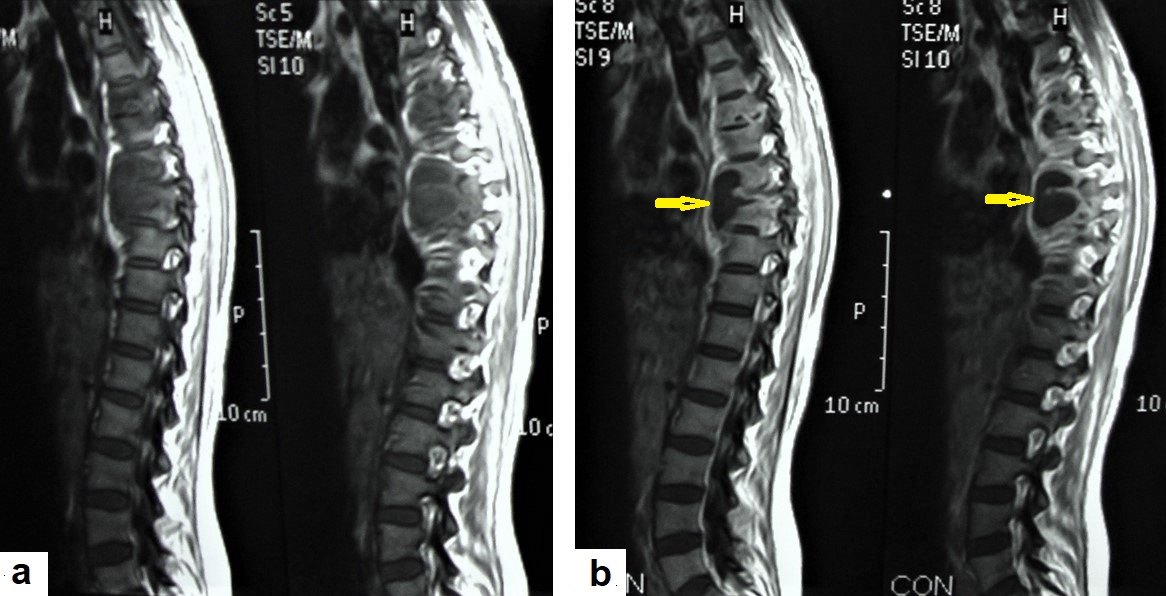
Figure 18. Pott’s disease in a 28-year-old female. Selected images of sagittal MRI of thoracic spine show destructive lesion affects multiple contiguous thoracic vertebrae with paraspinal collection. (a) Pre-contrast and (b) post-contrast T1-weighted images show subligamentous spread of the infection to involve five vertebrae with peripheral enhancement of the lesions, suggesting an abscess (arrow).
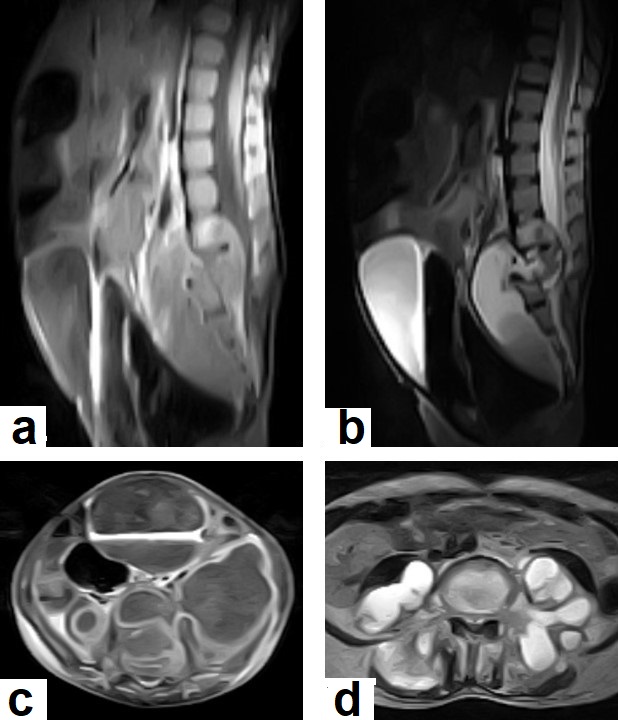
Figure 19. Pott’s disease in a 6-year-old female patient. Selected images of lumbosacral MRI. Sagittal (a) T1-weighted images and (b) T2-weighted images show that destructive lesion involves the T4/T5 disc and vertebrae, with extensive pre-vertebral loculated fluid collection. Selected axial images of MRI (c) T1-weighted image with gadolinium, and (d) T2-weighted image shows bilateral paravertebral loculated fluid collections involved in bilateral psoas; paravertebral muscles appear to have low-signal-intensity contents on T1-WIs with marginal enhancement after contrast administration and high-signal-intensity contents on T2-WIs (arrows). The picture is typical of Pott’s disease with bilateral psoas and paravertebral abscesses.
2.3. Abdominal TB
2.3. Abdominal TB:
TB can affect any organ or tissue in the abdominal cavity and can be mistakenly diagnosed as other inflammatory or neoplastic conditions. The most common affected organs are lymph nodes, the genitourinary system, the peritoneal cavity, and the gastrointestinal tract. The spleen, hepatobiliary, pancreas, and adrenals are rarely affected. However, these organs are more likely affected in HIV patients and in miliary TB [18][18] (Figures 20-22).
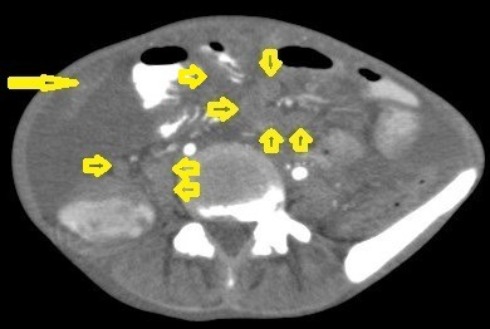
Figure 20. Tuberculous lymphadenitis in a 27-year-old women with cachexia, loss of appetite and cough. Axial abdominal CT image shows enlarged mesenteric, periaortic, and portahepatis lymph nodes (LNs), (short arrows) due to TB, which usually involves multiple groups, such as mesenteric and upper paraortic LNs. The image also shows relatively dense ascites and remarkable omental thickening forming cake-like mass (long arrow).
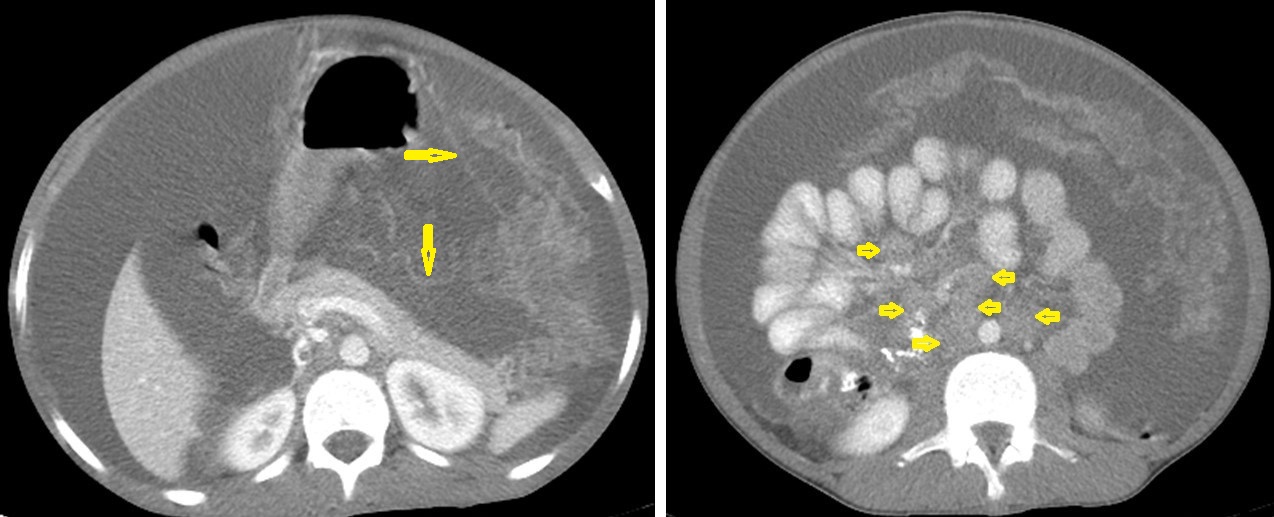
Figure 21. Wet peritonitis in a 16-year-old man with cachexia and loss of appetite. Selected axial abdominal images show marked relatively dense ascites and gross thickened omentum with faint enhancement of peritoneal reflections (long arrows) with multiple enlarged mesenteric and upper paraortic conglomerated lymph nodes (short arrows) with slight homogeneous enhancement.
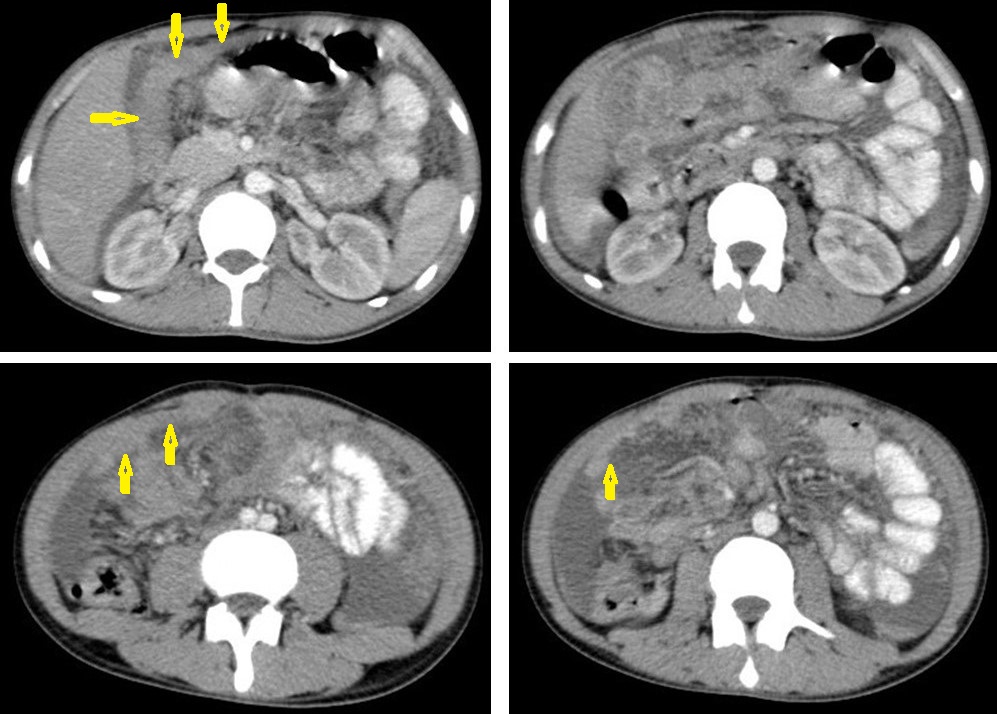
Figure 22. Fibrotic peritonitis in a 20-year-old man with fatigue, abdominal distension, and loss of appetite. Selected axial images of abdominal CT show remarkable omental thickening, forming cake-like masses (arrows) with faint enhancement and mild smooth thickening of peritoneal reflections associated with mild-to-moderate dense ascites and several low-attenuation mesenteric lymph nodes that are challenging to be distinguished from small bowel loops.
2.4. Genitourinary TB:
2.4. Genitourinary TB
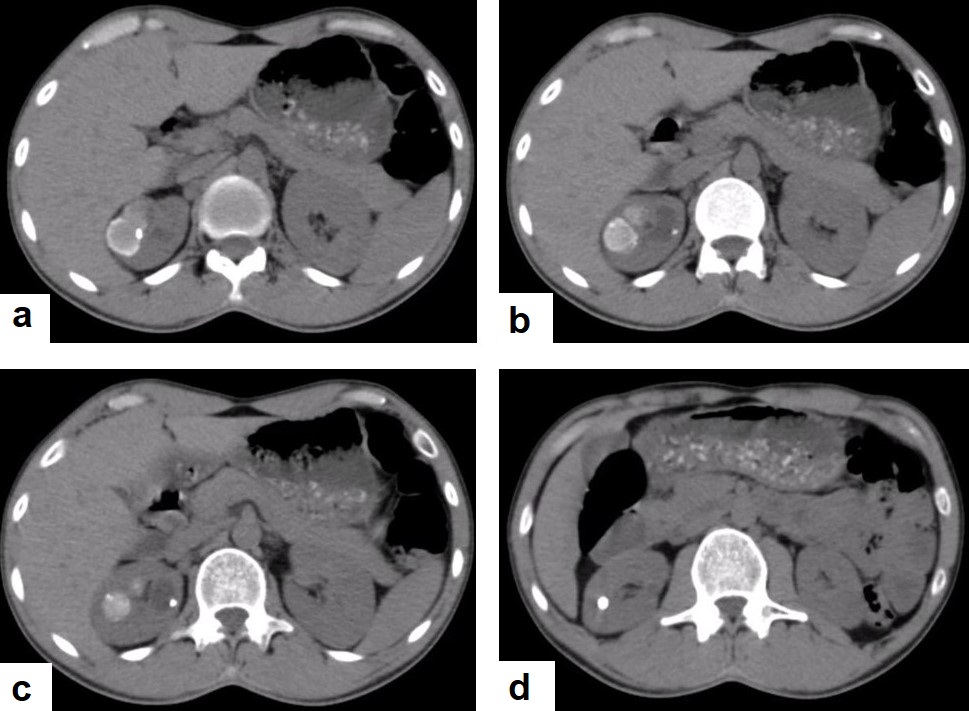
Figure 23. Renal TB in a 39-year-old man. Selected axial computed tomography images show (a) focal hyperdense non-enhancing nodules, with the largest at 26 mm, with calcified rim in the upper pole of the right kidney with focal scarring of the kidney. (b,c) Approximately, 20 mm cystic lesion in the upper calyx with focal calcification, most likely dilated calyx; and (d) 11 mm focal parenchymal calcification in the middle calyx.
2.5. Musculoskeletal (MSK) TB:
2.5. Musculoskeletal (MSK) TB
TB can affect any part of the MSK system, and symptoms of TB may be insidious, causing TB not to be considered. CT and MRI imaging modalities can bring suspicion to TB diagnosis [19]. MSK TB is a differential diagnosis of a wide range of bone lesions. High suspcion of TB is required, and a final diagnosis of TB can be carried out by using culture; in addition, a synovial biopsy may be needed [20][20] (Figure 24).
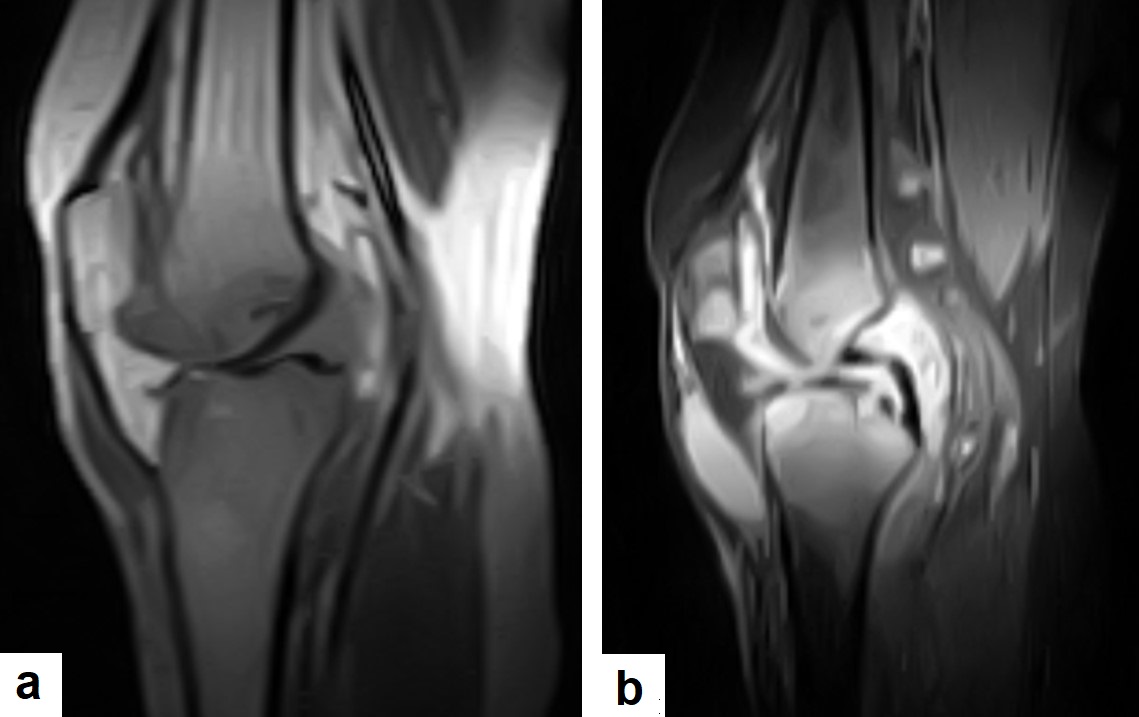
Figure 24. Knee TB in a 45-year-old patient with proved case of knee TB infection. Selected sagittal MRI images of (a) T1-weighted image and (b) T2-weighted image show extensive oedema of the articular surfaces of the knee, appearing as low signal intensity on T1 and high signal intensity on T2 with diffuse synovial thickening and large bone erosions (arrow heads), with mild joint effusion and a prepatellar pocket of fluid collection, which appear as low signal intensity on T1 and high signal intensity on T2. In addition, multiple enlarged popliteal lymph nodes were present.
Conclusions
3. Conclusions
TB is an important cause of nonspecific clinical and radiological manifestations, and it can masquerade as any benign or malignant medical case. Pulmonary TB can mimic any acute or chronic lung infection and even pulmonary carcinoma and metastasis. TB can masquerade as benign or malignant acute or chronic brain and spinal lesions. TB can cause ambiguous abdominal clinical and radiological manifestations, causing disastrous conditions and diagnostic challenges. TB can appear similar to any acute or chronic disease of the kidney and genitourinary system. TB is an important differential diagnosis to most of acute and chronic lesions in the joints and bones. Clinical manifestations and routine laboratory tests have limitations in directing physicians to diagnosing TB. Medical-imaging tests play an essential role in detecting tissue abnormalities and the early suspected diagnosis of TB in different body parts. Radiologists and physicians should be familiar with and aware of the radiological manifestations of TB to contribute to the early suspicion and diagnosis of TB. This review highlights the frequent radiological manifestations of TB that should be known by any physician.
References
- Nachiappan, A.C.; Rahbar, K.; Shi, X.; Guy, E.S.; Mortani Barbosa, E.J., Jr.; Shroff, G.S.; Ocazionez, D.; Schlesinger, A.E.; Katz, S.I.; Hammer, M.M. Pulmonary Tuberculosis: Role of Radiology in Diagnosis and Management. Radiographics 2017, 37, 52–72. https://doi.org/10.1148/rg.2017160032.
- Sahu, S.; Ditiu, L.; Sachdeva, K.S.; Zumla, A. Recovering from the Impact of the COVID-19 Pandemic and Accelerating to Achieving the United Nations General Assembly Tuberculosis Targets. Int. J. Infect. Dis. 2021, S1201–S9712, 164–168. https://doi.org/10.1016/j.ijid.2021.02.078.
- Ringold, S.; Lynm, C.; Glass, R.M. Tuberculosis. JAMA 2005, 293, 2820. https://doi.org/10.1001/jama.293.22.2820
- Lee, S.H. Tuberculosis Infection and Latent Tuberculosis. Tuberc. Respir. Dis. 2016, 79, 201–206. https://doi.org/10.4046/trd.2016.79.4.201.
- Tan, C.H.; Kontoyiannis, D.P.; Viswanathan, C.; Iyer, R.B. Tuberculosis: a benign impostor. AJR Am. J. Roentgenol. 2010, 194, 555–561. https://doi.org/10.2214/AJR.09.3055.
- Sari, N.I.P.; Mertaniasih, N.M.; Soedarsono Maruyama, F. Application of serial tests for Mycobacterium tuberculosis detection to active lung tuberculosis cases in Indonesia. BMC Res. Notes 2019, 12, 313. https://doi.org/10.1186/s13104-019-4350-9.
- Flores, J.; Cancino, J.C.; Chavez-Galan, L. Lipoarabinomannan as a Point-of-Care Assay for Diagnosis of Tuberculosis: How Far Are We to Use It? Front Microbiol. 2021, 15, 638047. https://doi.org/10.3389/fmicb.2021.638047.
- Kim, J.H.; Kim, E.S.; Jun, K.I.; Jung, H.G.; Bang, J.H.; Choe, P.G.; Park, W.B.; Song, K.H.; Kim, H.B.; Kim, N.J.; et al. Delayed diagnosis of extrapulmonary tuberculosis presenting as fever of unknown origin in an intermediate-burden country. BMC Infect. Dis. 2018, 18, 426. https://doi.org/10.1186/s12879-018-3349-5.
- Bomanji, J.B.; Gupta, N.; Gulati, P.; Das, C.J. Imaging in tuberculosis. Cold Spring Harb. Perspect. Med. 2015, 5, a017814. https://doi.org/10.1101/cshperspect.a017814.
- Skoura, E.; Zumla, A.; Bomanji, J. Imaging in tuberculosis. Int. J. Infect. Dis. 2015, 32, 87–93. https://doi.org/10.1016/j.ijid.2014.12.007.
- Yadav, J.; Verma, S.; Chaudhary, D.; Jaiwal, P.K.; Jaiwal, R. Tuberculosis: Current Status, Diagnosis, Treatment and Development of Novel Vaccines. Curr. Pharm. Biotechnol. 2019, 20, 446–458. https://doi.org/10.2174/1389201020666190430114121.
- Rasheed, W.; Qureshi, R.; Jabeen, N.; Shah, H.A.; Naseem Khan, R. Diagnostic Accuracy of High-Resolution Computed Tomography of Chest in Diagnosing Sputum Smear Positive and Sputum Smear Negative Pulmonary Tuberculosis. Cureus 2020, 12, e8467. https://doi.org/10.7759/cureus.8467.
- Bhalla, A.S.; Goyal, A.; Guleria, R.; Gupta, A.K. Chest tuberculosis: Radiological review and imaging recommendations. Indian J. Radiol. Imaging 2015, 25, 213–225. https://doi.org/10.4103/0971-3026.161431.
- Zou, H.; Pan, K.H.; Pan, H.Y.; Huang, D.S.; Zheng, M.H. Cerebral hemorrhage due to tuberculosis meningitis: a rare case report and literature review. Oncotarget 2015, 6, 45005–45009. https://doi.org/10.18632/oncotarget.6528.
- Khatri, G.D.; Krishnan, V.; Antil, N.; Saigal, G. Magnetic resonance imaging spectrum of intracranial tubercular lesions: one disease, many faces. Pol. J. Radiol. 2018, 83, e524–e535. https://doi.org/10.5114/pjr.2018.81408.
- Sanei Taheri, M.; Karimi, M.A.; Haghighatkhah, H.; Pourghorban, R.; Samadian, M.; Delavar Kasmaei, H. Central nervous system tuberculosis: An imaging-focused review of a reemerging disease. Radiol. Res. Pract. 2015, 2015, 202806. https://doi.org/10.1155/2015/202806.
- Chaudhary, V.; Bano, S.; Garga, U.C. Central Nervous System Tuberculosis: An Imaging Perspective. Can. Assoc. Radiol. J. 2017, 68, 161–170. https://doi.org/10.1016/j.carj.2016.10.007.
- Lee, W.K.; van Tonder, F.; Tartaglia, C.J.; Dagia, C.; Cazzato, R.L.; Duddalwar, V.A.; Chang, S.D. CT appearances of abdominal tuberculosis. Clin. Radiol. 2012, 67, 596–604. https://doi.org/10.1016/j.crad.2011.11.003.
- Leonard, M.K.; Blumberg, H.M. Musculoskeletal Tuberculosis. Microbiol. Spectr. 2017, 5. https://doi.org/10.1128/microbiolspec.
- Smits, M.; van de Groes, S.; Thurlings, R.M. Synovial Tissue Biopsy Collection by Rheumatologists: Ready for Clinical Implementation? Front. Med. 2019, 6, 138. https://doi.org/10.3389/fmed.2019.00138.
References
- Nachiappan, A.C.; Rahbar, K.; Shi, X.; Guy, E.S.; Mortani Barbosa, E.J., Jr.; Shroff, G.S.; Ocazionez, D.; Schlesinger, A.E.; Katz, S.I.; Hammer, M.M. Pulmonary Tuberculosis: Role of Radiology in Diagnosis and Management. Radiographics 2017, 37, 52–72. https://doi.org/10.1148/rg.2017160032.
- Sahu, S.; Ditiu, L.; Sachdeva, K.S.; Zumla, A. Recovering from the Impact of the COVID-19 Pandemic and Accelerating to Achieving the United Nations General Assembly Tuberculosis Targets. Int. J. Infect. Dis. 2021, S1201–S9712, 164–168. https://doi.org/10.1016/j.ijid.2021.02.078.
- Ringold, S.; Lynm, C.; Glass, R.M. Tuberculosis. JAMA 2005, 293, 2820. https://doi.org/10.1001/jama.293.22.2820
- Lee, S.H. Tuberculosis Infection and Latent Tuberculosis. Tuberc. Respir. Dis. 2016, 79, 201–206. https://doi.org/10.4046/trd.2016.79.4.201.
- Tan, C.H.; Kontoyiannis, D.P.; Viswanathan, C.; Iyer, R.B. Tuberculosis: a benign impostor. AJR Am. J. Roentgenol. 2010, 194, 555–561. https://doi.org/10.2214/AJR.09.3055.
- Sari, N.I.P.; Mertaniasih, N.M.; Soedarsono Maruyama, F. Application of serial tests for Mycobacterium tuberculosis detection to active lung tuberculosis cases in Indonesia. BMC Res. Notes 2019, 12, 313. https://doi.org/10.1186/s13104-019-4350-9.
- Flores, J.; Cancino, J.C.; Chavez-Galan, L. Lipoarabinomannan as a Point-of-Care Assay for Diagnosis of Tuberculosis: How Far Are We to Use It? Front Microbiol. 2021, 15, 638047. https://doi.org/10.3389/fmicb.2021.638047.
- Kim, J.H.; Kim, E.S.; Jun, K.I.; Jung, H.G.; Bang, J.H.; Choe, P.G.; Park, W.B.; Song, K.H.; Kim, H.B.; Kim, N.J.; et al. Delayed diagnosis of extrapulmonary tuberculosis presenting as fever of unknown origin in an intermediate-burden country. BMC Infect. Dis. 2018, 18, 426. https://doi.org/10.1186/s12879-018-3349-5.
- Bomanji, J.B.; Gupta, N.; Gulati, P.; Das, C.J. Imaging in tuberculosis. Cold Spring Harb. Perspect. Med. 2015, 5, a017814. https://doi.org/10.1101/cshperspect.a017814.
- Skoura, E.; Zumla, A.; Bomanji, J. Imaging in tuberculosis. Int. J. Infect. Dis. 2015, 32, 87–93. https://doi.org/10.1016/j.ijid.2014.12.007.
- Yadav, J.; Verma, S.; Chaudhary, D.; Jaiwal, P.K.; Jaiwal, R. Tuberculosis: Current Status, Diagnosis, Treatment and Development of Novel Vaccines. Curr. Pharm. Biotechnol. 2019, 20, 446–458. https://doi.org/10.2174/1389201020666190430114121.
- Rasheed, W.; Qureshi, R.; Jabeen, N.; Shah, H.A.; Naseem Khan, R. Diagnostic Accuracy of High-Resolution Computed Tomography of Chest in Diagnosing Sputum Smear Positive and Sputum Smear Negative Pulmonary Tuberculosis. Cureus 2020, 12, e8467. https://doi.org/10.7759/cureus.8467.
- Bhalla, A.S.; Goyal, A.; Guleria, R.; Gupta, A.K. Chest tuberculosis: Radiological review and imaging recommendations. Indian J. Radiol. Imaging 2015, 25, 213–225. https://doi.org/10.4103/0971-3026.161431.
- Zou, H.; Pan, K.H.; Pan, H.Y.; Huang, D.S.; Zheng, M.H. Cerebral hemorrhage due to tuberculosis meningitis: a rare case report and literature review. Oncotarget 2015, 6, 45005–45009. https://doi.org/10.18632/oncotarget.6528.
- Khatri, G.D.; Krishnan, V.; Antil, N.; Saigal, G. Magnetic resonance imaging spectrum of intracranial tubercular lesions: one disease, many faces. Pol. J. Radiol. 2018, 83, e524–e535. https://doi.org/10.5114/pjr.2018.81408.
- Sanei Taheri, M.; Karimi, M.A.; Haghighatkhah, H.; Pourghorban, R.; Samadian, M.; Delavar Kasmaei, H. Central nervous system tuberculosis: An imaging-focused review of a reemerging disease. Radiol. Res. Pract. 2015, 2015, 202806. https://doi.org/10.1155/2015/202806.
- Chaudhary, V.; Bano, S.; Garga, U.C. Central Nervous System Tuberculosis: An Imaging Perspective. Can. Assoc. Radiol. J. 2017, 68, 161–170. https://doi.org/10.1016/j.carj.2016.10.007.
- Lee, W.K.; van Tonder, F.; Tartaglia, C.J.; Dagia, C.; Cazzato, R.L.; Duddalwar, V.A.; Chang, S.D. CT appearances of abdominal tuberculosis. Clin. Radiol. 2012, 67, 596–604. https://doi.org/10.1016/j.crad.2011.11.003.
- Leonard, M.K.; Blumberg, H.M. Musculoskeletal Tuberculosis. Microbiol. Spectr. 2017, 5. https://doi.org/10.1128/microbiolspec.
- Smits, M.; van de Groes, S.; Thurlings, R.M. Synovial Tissue Biopsy Collection by Rheumatologists: Ready for Clinical Implementation? Front. Med. 2019, 6, 138. https://doi.org/10.3389/fmed.2019.00138.
