Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Beatrix Zheng and Version 1 by Catalina Iulia Saveanu.
Medical and teaching staff can present useful and complex information about hand hygiene in the courses and can be models for students, leading them to properly practice HD techniques. In addition, prevention lectures are considered a reliable source of information by the investigated subjects. The media also play an important role through public information programs.
- hand hygiene
- antiseptic solution
- decontamination
1. Introduction
Infection control in dentistry is a broad concept on several levels. The increase in the incidence of certain diseases, including SARS-CoV-2 infection, is also linked to the lack of compliance of medical staff on various issues. Hand hygiene (HH) is the basis of any program for infection control [1,2,3,4,5,6][1][2][3][4][5][6]. However, the promotion of hand hygiene behavior remains a complex issue [3,7,8][3][7][8]. Task forces for discussion and expert consensus on critical issues related to hand hygiene in health care are based on behavioral changes, education, training, tools, World Health Organization (WHO)-recommended hand antisepsis formulations, glove use, water quality for handwashing, patient involvement, religious and cultural aspects of hand hygiene, indicators for service implementation and monitoring, regulation and accreditation, communication/campaigning, and national guidelines on hand hygiene [9]. Hand hygiene is a good predictor of nosocomial infections, especially when the medical staff come in contact with a patient’s oral cavity [10]. HH is a widespread topic among students or practitioners. Aspects regarding HH have been addressed in numerous studies conducted during the pandemic period with SARS-CoV-2 [11,12,13][11][12][13].
2. Detailed Analysis
The mean age of the students was 23.15 years (± 2.083), with the youngest being 19 years old and the eldest being 37 years old. The general characteristics of the study group are presented in (Table 1).
Table 3. Response rate percentage regarding infection control by simple hand decontamination. Results of statistical significance tests.
Table 1. General characteristics of the study group.
| Questions | Frequency of Responses %(Count) | G | A | U | S | Y | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| p | p | p | p | p | |||||||
Response rate percentage regarding infection control by simple hand decontamination. Results of statistical significance tests.
| Question | Frequency | G | A | U | S | Y | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | p | p | p | p | P | 0/Day | 1–2/Day | 3–5/Day | 6–10/Day | >10/Day | |||||
| %(Count) | %(Count) | |||||||||||||||
| Q 5 | Frequency of simple hand washing before the SARS-CoV-2 pandemic | 0.8(1) | ||||||||||||||
| Q16 | Antiseptic solutions are used when hands are not visibly dirty? | 77(97)4.8(6) | 43.7(55) | 39.7(50) | 23(29) | 0.5111.1(14) | 0.376 | 0.58 | 0.09 | 0.060.591 | 0.09 | 0.32 | 0.040 | |||
| 0.05 | Q 6 | Frequency of simple hand washing during the SARS-CoV-2pandemic | 0 | 1.6(2) | ||||||||||||
| Q17 | Antiseptic solutions reduce the resident flora from the skin surface? | 85.7(108) | 14.3(18)17.5 (22) | 38.1(48) | 42.9(54) | 0.504 | 0.130.715 | 0.12 | 0.70 | 0.42 | 0.730.66 | 0.07 | 0.42 | |||
| Never | ||||||||||||||||
| Q18 | Antiseptic solutions are used when soap and water are not available?Rarely | Sometimes | Often | Always | ||||||||||||
| 82.5(104) | 17.5(22) | 0.16 | 0.79 | 0.25 | 0.54 | 0.21 | Q 7 | Do you perform HH before and after contact with the patient? | 0 | 0 | 3.2(4) | 0.8(1) | ||||
| Q19 | 96(121) | 0.84 | 0.14 | 0.25 | Antiseptic soap is more effective than antiseptic solutions?0.38 | 43.7(55) | 56.3(71) | 0.40 | 0.380.37 | |||||||
| 0.11 | 0.93 | 0.01 | Q 8 | Do you perform HH before applying gloves? | ||||||||||||
| Q20 | Does soap remove organic matter and transient flora?0.8(1) | 0 | 7.3(11) | 84.1(106) | 15.9(20)9.3(14) | 82(123) | 0.44 | 0.41 | 0.20 | 0.01 | 0.14 | |||||
| 0.24 | 0.54 | 0.30 | 0.08 | 0.57 | Q 9 | Do you perform HH after removing gloves? | 0 | 0 | 4(5) | 15.9(20) | 80.2(101) | 0.09 | 0.60 | 0.20 | 0.92 | 0.17 |
| Q21 | Can simple hand decontamination control the infections before aseptic procedures? | 84.9(107) | 15.1(19) | 0.64 | 0.84 | 0.85 | 0.29 | 0.60 | Q 10 | Do you perform HH after using the toilet? | ||||||
| Q22 | 0 | 0 | 0.7(1) | 0 | 96.7(145) | 0.85 | 0.13 | Can simple hand decontamination control the infections after touching the surfaces near the patient? | 85.7(108) | 14.3(18)0.14 | 0.40 | 1.0 | 0.88 | 0.830.37 | 0.38 | |
| 0.90 | Q 11 | Do you perform HH before meal? | 0 | 0 | 3.2(4) | 2.4(3) | 94.4(119) | 0.95 | 0.19 | 0.14 | 0.59 | 0.04 | ||||
| Q23 | Can simple hand decontamination control the infections after exposure to biological fluids? | 85.7(108) | 14.3(18) | 0.74 | 0.29 | 0.88 | 0.42 | 0.28 | Q 12 | Do you perform HH when hands are visibly dirty? | 0.8(1) | 0 | ||||
| Q24 | Can simple hand decontamination control the infections after direct contact with the patient? | 93.7(118)3.2(4) | 3.2(4) | 92.9(117) | 0.95 | 6.3(8)0.24 | 0.09 | 0.11 | 0.09 | 0.100.01 | 0.09 | 0.44 | ||||
| 0.80 | Q 13 | How often do you use soap? | 1.6(2) | 2.4(3) | 9.5(12) | 9.5(12) | 77(97) | 0.61 | 0.83 | 0.08 | 0.66 | 0.93 | ||||
| Q25 | Can simple hand decontamination control the infections before direct contact with the patient? | 91.3(115) | 8.7(11) | Q 14 | How often do you use antiseptique soap? | 7.9(12) | 20.6(26) | 30.2(38) | 24.6(31) | 16.7(21) | 0.02 | 0.23 | 0.59 | 0.70 | 0.92 | |
| Q 15 | How often do you use antiseptique gel? | 0 | 6.3(8) | 17.5(22) | 36.5(46) | 39.7(50) | 0.10 | 0.26 | 0.07 | 0.29 | 0.06 | |||||
| Q | Year of Study | Total | ||||||||||||||
| 3rd | 4th | 5th | 6th | |||||||||||||
| N | N | N | N | N | % | |||||||||||
| Total | 29 | 31 | 18 | |||||||||||||
G = gender, A = area, U = University, S = specialization, Y = year of study, p = significance level.
No statistically significant differences were found in terms of educational background or gender. Most students always perform HH before and after contact with the patient, before applying gloves, after removing gloves, after using the toilet, before meals, and when hands are visibly dirty (Table 2).
Statistically significant differences were found in hands washing after using the toilet by year of study, in favor of sixth-year students (p < 0.05) and in hand washing when hands are visibly dirty by the university attended (p < 0.05), with a higher percentage for students attending the university in Iasi (61.9%) compared to those attending the UMP2 (30.95%). Female students use antiseptic soap more often than male students (p < 0.05). Most students consider that simple hand decontamination can prevent the transmission of infections after contact with the patient, followed in descending order by: immediately after exposure to biological fluids (saliva, blood), after touching the areas near the patient, and before aseptic procedures. Although differences were found in the response rate percentage regarding infection control by hand decontamination and the frequency of solutions used, these differences were not statistically significant by gender, background, specialization, university or year of study (p ˃ 0.05). A percentage of 15.9% (20) of the investigated students do not know that washing with soap and water removes organic matter and transient flora from the skin surface, and 43.7% of them (55) consider that antiseptic soap is more effective than antiseptic solutions.
The vast majority of students agree that antiseptic solutions are used when soap and water are not available and 14.3% (18) do not know that rubbing hands with antiseptic solutions reduces the resident flora on the skin surface. A considerable percentage of the students, 77% (97) use antiseptic solutions when the hands are not visibly dirty (Table 3).
| 0.88 |
| 0.86 |
| 0.15 |
| 0.24 |
| 0.42 |
| 48 | ||||||||
| 126 | 100 | |||||||
| Q1 | Gender | Male | 6 | 9 | 7 | 10 | 32 | 25.4 |
| Female | 23 | 22 | 11 | 38 | 94 | 74.6 | ||
| Q2 | Area | Rural | 13 | 10 | 11 | 15 | 49 | 38.9 |
| Urban | 16 | 21 | 7 | 33 | 77 | 61.1 | ||
| Q3 |
G = gender, A = area, U = University, S = specialization, Y = year of study, p = significance level.
A percentage of 40.5% (51) of the investigated students state that they have “to a very large extent”sufficient knowledge, whereas 50.8% (64) of them consider that they have “largely” sufficient knowledge regarding the techniques of hand decontamination. Most students claim that they know that hand decontamination is a measure to control infection. Only 48.4% of them (60) feel guilty and 44.4% (56) feel frustrated when they fail to perform proper hand hygiene. Not all students follow the recommendations of the World Health Organization guide on HH. No significant differences were observed by gender, background, specialization, university or year of study (p ˃ 0.05) (Figure 1).
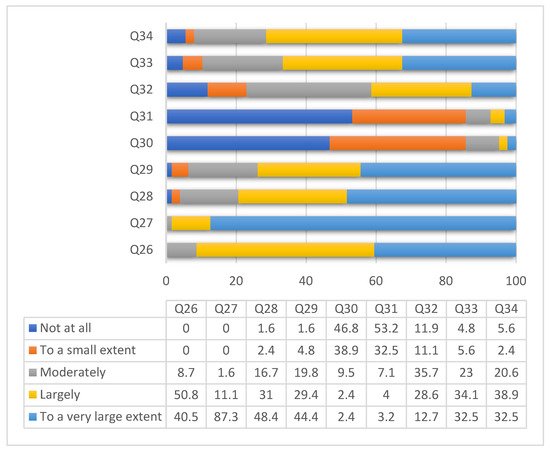
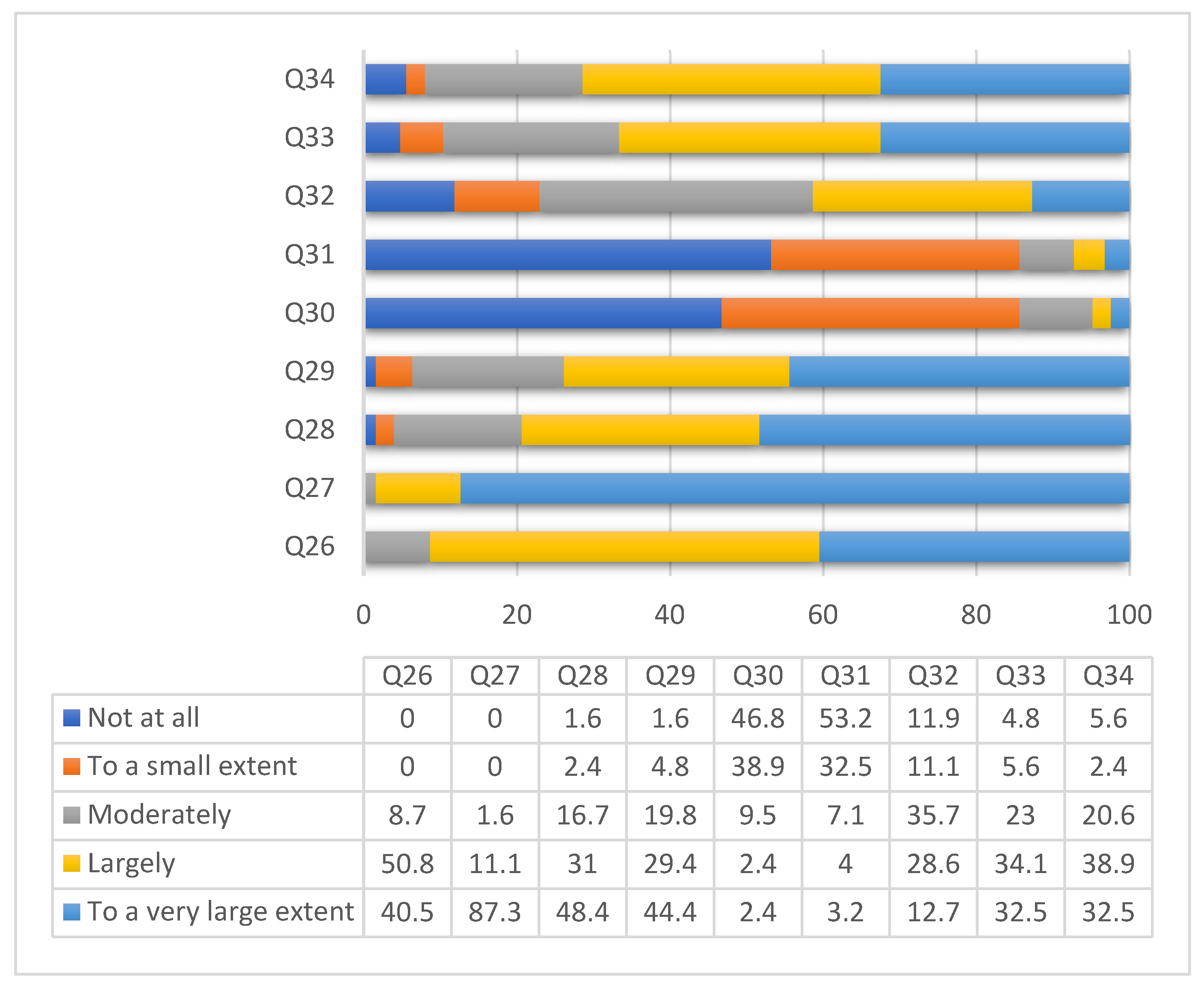 Figure 1.
Figure 1.
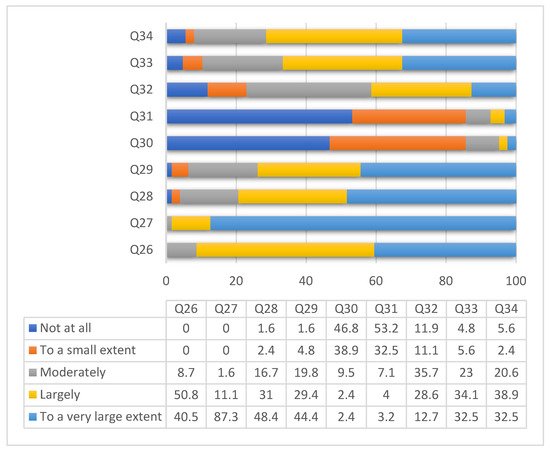
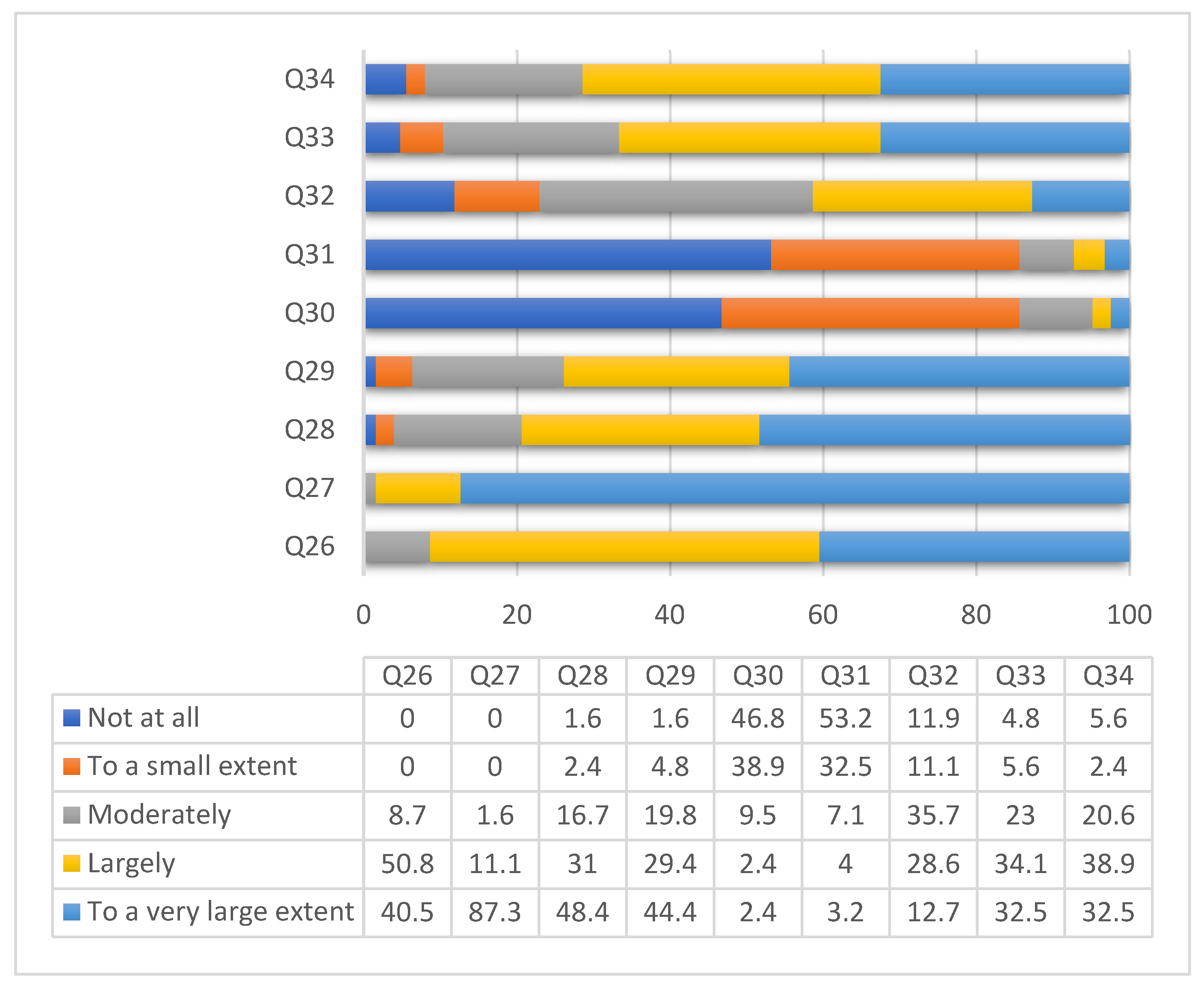 Figure 1.
Figure 1. Distribution of answers concerning knowledge on hand decontamination. The questions were as follows: Q26 = I have sufficient knowledge of HH techniques; Q27 = I consider HH to be a measure of infection control; Q28 = When I fail to do proper HH I feel guilty; Q29 = When others omit HH, I feel frustrated; Q30 = Sometimes I forget to make HH; Q31 = Emergencies make me not practice HH; Q32 = Sometimes I explain to others the correct HH technique; Q33 = I use the HH technique recommended by WHO; Q34 = I perform HH with antiseptic according to WHO recommendations.
Distribution of answers concerning knowledge on hand decontamination. The questions were as follows: Q26 = I have sufficient knowledge of HH techniques; Q27 = I consider HH to be a measure of infection control; Q28 = When I fail to do proper HH I feel guilty; Q29 = When others omit HH, I feel frustrated; Q30 = Sometimes I forget to make HH; Q31 = Emergencies make me not practice HH; Q32 = Sometimes I explain to others the correct HH technique; Q33 = I use the HH technique recommended by WHO; Q34 = I perform HH with antiseptic according to WHO recommendations.
Regarding surgical hand washing, almost all students consider the following issues to be important: removal of jewelry, watch and artificial nails, as well as shortening of nails before surgical HH. A percentage of 70.6% (89) consider that antiseptic soap with 4% chlorhexidine (CHX) can be used for surgical washing, and 73.0% (92) know that the hands should be kept up and the elbows should be kept down during surgical washing. A large percentage of students, 96.8% (122), know the surfaces of the hands that need to be decontaminated during surgical washing. Significant differences were found by year of study regarding the hand areas for decontamination, by year of study, specialization and gender regarding the positioning of hands and elbows, and by gender regarding forearm inclusion in surgical HH (p < 0.05) (Table 4).
Table 4. Response rate percentage regarding infection control by surgical decontamination. Results of statistical significance tests.
Response rate percentage regarding infection control by surgical decontamination. Results of statistical significance tests.
| Question | Frequency | G | A | U | S | Y | ||
|---|---|---|---|---|---|---|---|---|
| Yes | No | p | p | p | p | p | ||
| %(Count) | %(Count) | |||||||
| 0.02 | ||||||||
| 0.64 | ||||||||
| 0.14 | ||||||||
| 0.06 | 0.68 | |||||||
G = gender, A = area, U = University, S = specialization, Y = year of study, p = significance level.
Most of the students consider that the time required to wash their hands with soap and water is of 30–60 s, and the time required to decontaminate their hands with antiseptic is 20 s (Table 5). The duration of surgical HH was estimated at 2–3 min or 5 min by approximately equal percentages of students. The concentration of ethanol in antiseptic was estimated at 70% by half of the investigated students, and the required amount of antiseptic solution to be used was estimated at 3–5 mL by 69.8% (88) of the students. A little more than a half of respondents consider that the residual action of antiseptics is due to CHX. For hand drying, 52.4% (66) of students use a cotton towel and 45.2% (57) use paper towels. The multitude of answers regarding the importance of washing hands with soap and water confirms the hypothesis. Faculty courses were the main source of information on HH for 65.9% (83) of the students. Significant differences (p < 0.05) were found in the recommended duration for HH by year of study, in the usual concentration of ethanol in antiseptic, in the reason for a residual action and in the method of hand drying by specialization, and in hand washing with soap and water as a habit by gender.
Table 5. Frequency of answers to questions concerning antiseptic substances for HH. Results of statistical significance tests comparing the frequency of answers on antiseptic substances for HH, by variables.
Frequency of answers to questions concerning antiseptic substances for HH. Results of statistical significance tests comparing the frequency of answers on antiseptic substances for HH, by variables.
| Question | Interval | G | A | U | S | Y | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Frequency %(Count) | p | p | p | p | p | ||||||
| Q35 | Do you consider it important to remove jewelry prior to surgical HH? | 97.6(123) | 2.4(3) | 0.31 | 0.84 | 0.19 | 0.49 | 0.17 |
| Q43 | The duration of HH with soap | 10 s | 20 s | 30–60 s | 2 m | 0.23 | 0.82 | 0.17 | 0.11 | 0.02 | ||||||||||
| Q36 | Do you consider it important to remove watch prior to surgical HH? | 95.2(120) | 4.8(6) | 0.65 | 0.15 | 0.93 | 0.39 | 0.45 | ||||||||||||
| 0.8(1) | 38.1(48) | 54(68) | 7.1(9) | Q37 | Do you consider it important to shorten nails prior to surgical HH? | 97.6(123) | 2.4(3) | 0.75 | 0.84 | 0.24 | 0.06 | 0.34 | ||||||||
| Q44 | The duration of HH with antiseptic solution | 10 s | 20 s | 30–60 s | 2 m | 0.62 | 0.87 | 0.28 | 0.83 | 0.05 | Q38 | Do you consider it important to remove artificial nails prior to surgical HH? | 99.2(125) | |||||||
| 18.3(23) | 63.5(80) | 0.8(1) | 0.56 | 0.42 | 0.46 | 0.29 | 0.65 | |||||||||||||
| 18.3(23) | 0.0(0) | Q39 | Do you wash your hands with 4% CHX soap? | 70.6(89) | 29.4(37) | 0.13 | 0.58 | 0.39 | 0.90 | |||||||||||
| Q45 | The duration of surgical HH | 1–2 m | 2–3 m | 0.35 | 5 m | 10 m | 0.57 | 0.41 | 0.73 | 0.05 | 0.61 | University | UMP1 | 26 | 3 | 10 | 43 | 82 | 65.1 | |
| Q40 | The areas to be decontaminated are: palmar and dorsal face, interdigital area, thumbs, fingertips and wrist? | 96.8(122) | 3.2(4) | 0.99 | 0.56 | 0.52 | 0.25 | 0.004 | ||||||||||||
| 0.0(0) | 42.9(53) | 43.7(54) | 13.5(17) | UMP2 | 3 | 28 | 8 | 5 | 44 | |||||||||||
| Q41 | 34.9 | |||||||||||||||||||
| D you keep your hands up and elbows down during surgical HH? | 73(92) | 27(34) | 0.01 | 0.46 | 0.23 | 0.0 | 0.006 | |||||||||||||
| Q46 | What is the concentration of ethanol in antiseptic solutions? | 40–60% | Q4 | Specialization | Dental Medicine | 26 | 7 | 8 | 26 | 67 | ||||||||||
| Q42 | 53.2 | |||||||||||||||||||
| Does surgical HH include the forearms? | General Medicine | 3 | 24 | 10 | 22 | 59 | 46.8 |
Attitude regarding HH before and during the SARS-CoV-2 pandemic indicated that HH was performed by 42.9% of the students more than 10 times a day during the pandemic, compared to 10% before its onset. Statistically significant differences were found only by the year of study (p < 0.05) (Table 2), with students in the 6th year performing HH more frequently.
G = gender, A = area, U = University, S = specialization, Y = year of study, p = significance level, s = secondes; m = minutes, CHX= Chlorhexidine
Table 2. Frequency of answers to questions concerning hand hygiene (HH) in relation to the patient and other situations and the use of HH products. Results of statistical significance tests comparing the frequency of HH in relation to the patient and the use of HH products by variables.
Frequency of answers to questions concerning hand hygiene (HH) in relation to the patient and other situations and the use of HH products. Results of statistical significance tests comparing the frequency of HH in relation to the patient and the use of HH products by variables.
| 70% |
| 90% | |||||||||||
| I don’t know | |||||||||||
| 0.86 | 0.06 | 0.22 | 0.03 | 0.09 | |||||||
| 96.8(122) | 3.2(4) | ||||||||||
| 18.3(23) | 54.8(69) | 5.6(7) | 21.4(27) | ||||||||
| Q47 | What is the recommended amount of antiseptic? | 1–2 mL | 3–5 mL | 7 mL | 10 ml | 0.94 | 0.35 | 0.87 | 0.89 | 0.74 | |
| 22.2(28) | 69.8(88) | 7.9(10) | 0.0(0) | ||||||||
| Q48 | Antiseptics have a residual action if they contain: | Glycerin | CHX | Triclosan | Iodoform | 0.05 | 0.13 | 0.39 | 0.05 | 0.53 | |
| 19.8(25) | 54(68) | 14.3(18) | 11.9(15) | ||||||||
| Q49 | What do you use most often to dry hands? | Cotton | Paper | Gown sleeve | Dryer | I don’t dry | 0.79 | 0.59 | 0.16 | 0.00 | 0.90 |
| 52.4(66) | 45.2(57) | 0.8(1) | 1.6(2) | 0.0(0) | |||||||
| Q50 | Has washing your hands with soap become a habit? | Not at all | To a small extent | Moderately | Largely | Very largely | 0.01 | 0.25 | 0.32 | 0.31 | 0.21 |
| 0.0(0) | 0.0(0) | 0.8(1) | 7.1(9) | 92.1(116) | |||||||
| Q51 | What were your sources of information? | Media | Faculty | Family | Friends | 0.16 | 0.92 | 0.86 | 0.76 | 0.43 | |
| 17.5(22) | 65.9(83) | 10.3(13) | 4.8(6) | 1.6(2) |
3. Current Insights
Knowledge of HH infection control methods is essential for students [3,10,11,12,13,25,26][3][10][11][12][13][14][15]. HH is a routine procedure, which aims to remove organic matter and transient flora. The use of an antiseptic soap will determine, in addition to the cleansing action by the physical removal of organic matter, the inactivation of microorganisms, by the action of antiseptic substances in its composition [3]. The results of the present study show that the level of students’ knowledge on the five moments of HH is high. In tThis study, we did not assess the e level of knowledge before the onset of the SARS-CoV-2 pandemic was not assessed here, but the results of other studies indicate that the majority of respondents (83%) had a high knowledge of HH, due to the development of student training programs [27][16]. However, another study conducted before the onset of the SARS-CoV-2 pandemic found that only 63% of medical students included in their study knew the five moments of HH [28][17].
Another parameter considered was the duration of simple and antiseptic decontamination of the hands. Approximatively half of all respondents (54%) know the recommended duration of 20–30 s for simple HH whereas 38% consider that 20 s is enough for complete hand cleaning. In the field of HH, there is a European standard for the evaluation of the effectiveness of antiseptic agents for HD: EN 1499 (HH washing), EN1500 (HH rubbing) and EN12791 (surgical HH) [10]. However, many students enrolled in the present study consider that glycerin is used for its antiseptic action and, moreover, that it would have a residual action. The fact that some students consider that triclosan has remanent action and not CHX again indicates a low level of knowledge. Compared to simple soap, the one containing 0.3% triclosan did not lead to a significant reduction in microorganisms, except E. faecalis [10,29][10][18]. In addition, the use of triclosan is controversial because of several side effects that have been reported, such as carcinogenic effects, allergies, endocrine disorders, acute or chronic toxicity, antibiotic resistance. Therefore, in 2016, the US Food and Drug Administration banned triclosan and 17 other ingredients in antiseptic soaps, requesting more data on the efficacy and safety of these antiseptic agents [30][19].
A particularly important aspect is the fact that 44.7% (67) of the students do not know the action of CHX although, currently, it is considered to be the most frequently used antiseptic agent. In this context we can, say that the ignorance of the advantages of using CHX implicitly attracts its non-use in practice. CHX is used in concentrations of 2% and 4% with a very wide spectrum of action and a residual action that lasts several hours [31][20]. CHX in the 0.5% concentration may increase the effectiveness of alcohol-based antiseptic. CHX is inactivated by anionic agents, and for this reason, it is recommended to avoid the use of creams or soaps [32,33][21][22].
The use of iodophors was indicated by only 10.7% (16) of the students. The majority of students did not know that the iodophors are antibacterial agents with a broad spectrum of activity and a prolonged action.
Alcohol is the most effective, the safest and the most widely used HH agent. Ethyl alcohol has a broad spectrum of activity at an increased concentration of 70–80%, but with limited action in eliminating spores [10]. The effectiveness of alcohol is influenced by many factors such as: the type of alcohol used and its concentration, the contact time, the amount applied and skin moisture. In vitro studies have shown that hydroalcoholic solutions containing 60–80% alcohol have reduced bacteria by 4-log to 6-log in 30 s; a shorter application time decreases the efficiency of the hydroalcoholic solution and is associated with the use of a smaller amount of product [34][23]. N-propanol is effective against hepatitis B virus, HIV, influenza A virus, rotavirus, adenovirus and bacteria at 60–90% concentration. HH with alcohol-based agents is the key measure in the prevention of healthcare-associated infections and nosocomial transmission of pathogens. A study conducted in Germany which involved dental students showed that improvements in general knowledge and special efforts were needed to increase compliance with HH [35][24].
The time required to rub hands with hydro-alcoholic solutions was known by 65.3% of students involved in this study. This result is in contrast to a study conducted in Pakistan, which reported that only 20% of respondents were aware of this issue [36][25]. A prospective study in an intensive-care and pediatrics unit in France showed that only a third of students knew the appropriate duration of hand rubbing before theoretical training and, furthermore, the duration of hand decontamination was found to decrease significantly during repeated procedures [37][26].
It was noteworthy that the stages of preoperative preparation of the hands were known by more than 90% of the students, and almost all respondents (97.3%) stated that the areas that need to be decontaminated are the palmar and dorsal face of the hands, the interdigital area, the thumbs, the fingertips and the wrist. On the other hand, the answers regarding surgical HH technique showed that the respondents have knowledge regarding surface area: although 97.3% of them stated that surgical HH includes the forearms, only one third (31.3%) had deeper knowledge of the notion of the correct position of the forearms during the preoperative preparation of the hands. HH is a behavioral practice, so it is important to identify the reasons for non-compliance with recommendations. In the current study, 6.7% of students answered that emergencies and other priorities make it difficult to practice HH; however, 98.7% noted that they feel guilty when they fail to perform HH, and 98% feel frustrated when those around them omit HH. Similar findings were found in a study conducted in India on a group of 130 students, where about 40% of medical students said that emergencies cause them to practice HH with difficulty and that they considered they could adhere to good HH practices if hygiene facilities were adequate and handy [38][27].
In this study, it was observed that students wash their hands more than 10 times a day after the onset of the SARS-CoV-2 pandemic. A similar result was reported by Dwipayanti et al. in Indonesia [12].
Hand drying is a routine procedure but certain aspects must be taken into account, namely: the cotton towel can be recommended but should be used only once and then reprocessed because the humid environment will favor microbial colonization; the disposable paper towel is the best option—in addition to drying, it also removes the bacteria from the skin. A hot air dryer is not recommended because it causes the aerial dissemination of microorganisms, especially when the hands are rubbed together, and, in addition, requires a longer use time of about 40 s, produces noise, causes excessive drying of the skin and should be cleaned often [39][28]. Factors associated with the choice of hand-drying method include the availability of the method, the possibility of minimizing contact with the surrounding surfaces, the perception and the rapidity of the method [40][29]. On the other hand, there are studies showing that, instead of electric dryers, the use of paper towels reduces the spread of bacteria, recommended in hospitals or in areas at high risk of cross-contamination, [41][30]. In recent years, a new version of the hot air dryer has been introduced, the air-jet dryer with antibacterial filter. It has a similar efficiency to disposable wipes and requires a relatively shorter drying time compared to the hot air dryer, which helps to improve compliance. However, it has been noticed that the dispersion of bacteria in the air can reach up to 3 m, due to the high speed of air emission during use, therefore such devices are not recommended within medical facilities [42,43][31][32].
4. Conclusions
Within the limits of this study, we can admit that eEducational measures are needed in order to guide medical staff for 100% compliance with the knowledge and adoption of HH measures. In order to prevent the transmission of microorganisms between patients and dental staff, high compliance with infection control practices is required. The study shows that most students know the moments of HH, meaning that high compliance is needed to prevent infection control. The causes of non-compliance with hand decontamination rules are emergencies and other priorities. Most students explain, to some extent, to those around them the appropriate HH technique, an attitude of responsibility emphasized also by the fact that most students follow WHO recommendations. The most commonly used product for drying hands was the cotton towel (51.3%), followed by the paper towel (44%) and the hand dryer (2.7%). Only 2% said they do not dry their hands. Unfortunately, half of the students use a cotton towel to dry their hands instead of a paper towel. A very small percentage of students are unaware of the disadvantages of drying their hands with a hand dryer and, therefore, use it. The most important sources of information on the correct HH are faculty courses and the media. The study highlights the need to improve training programs to achieve a higher level of knowledge related to hand hygiene.
References
- Rotter, M. Hand washing and hand disinfection. In Hospital Epidemiology and Infection Control, 2nd ed.; Mayhall, C.G., Ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1999; Chapter 87.
- Centers for Disease Control and Prevention: Show Me the Science—When & How to Use Hand Sanitizer in Community Settings. Available online: https://www.cdc.gov/handwashing/show-me-the-science-hand-sanitizer.html (accessed on 25 February 2021).
- World Health Organization. Hand Hygiene—Why, How and When? 2009. Available online: https://www.who.int/gpsc/5may/Hand_Hygiene_Why_How_and_When_Brochure.pdf (accessed on 2 March 2021).
- Nuwagaba, J.; Rutayisire, M.; Balizzakiwa, T.; Kisengula, I.; Nagaddya, E.J.; Dave, D.A. The Era of Coronavirus: Knowledge, Attitude, Practices, and Barriers to Hand Hygiene Among Makerere University Students and Katanga Community Residents. Risk Manag. Healthc. Policy 2021, 14, 3349–3356.
- UNICEF. Everything You Need to Know about Washing Your Hands to Protect Against Coronavirus (COVID-19). Washing Your Hands can Protect You and Your Loved Ones. Available online: https://www.unicef.org/coronavirus/everything-you-need-know-about-washing-your-hands-protect-against-coronavirus-COVID-19 (accessed on 3 August 2021).
- Ejemot-Nwadiaro, R.I.; Ehiri, J.E.; Arikpo, D.; Meremikwu, M.M.; Critchley, J.A. Hand washing promotion for preventing diarrhoea. Cochrane Database Syst. Rev. 2015, 9, 12.
- Curtis, V.; Cairncross, S. Effect of washing hands with soap on diarrhoea risk in the community: A systematic review. Lancet Infect. Dis. 2003, 3, 275–281.
- Stone, S.; Teare, L.; Cookson, B. Guiding hands of our teachers. Hand-hygiene Liaison Group. Lancet 2001, 357, 479–480.
- Pittet, D. Improving compliance with hand hygiene in hospitals. Infect. Control Hosp. Epidemiol. 2000, 21, 381–386.
- WHO. Clean Care is Safer Care, Clean Hands Protect Against Infection. Available online: https://www.who.int/gpsc/clean_hands_protection/en/. (accessed on 22 December 2021).
- Rahim, M.H.A.; Ibrahim, M.I.; Noor, S.S.M.; Fadzil, N.M. Predictors of Self-Reported Hand Hygiene Performance among Nurses at Tertiary Care Hospitals in East Coast Malaysia. Int. J. Environ. Res. Public Health 2021, 18, 409.
- Dwipayanti, N.M.U.; Lubis, D.S.; Harjana, N.P.A. Public Perception and Hand Hygiene Behavior During COVID-19 Pandemic in Indonesia. Front. Public Health 2021, 9, 621800.
- Alsoufi, A.; Alsuyihili, A.; Msherghi, A.; Elhadi, A.; Atiyah, H.; Ashini, A.; Ashwieb, A.; Ghula, M.; Ben Hasan, H.; Abudabuos, S.; et al. Impact of the COVID-19 pandemic on medical education: Medical students’ knowledge, attitudes, and practices regarding electronic learning. PLoS ONE 2020, 15, e0242905.
- Pittet, D.; Allegranzi, B.; Sax, H.; Dharan, S.; Pessoa-Silva, C.L.; Donaldson, L.; Boyce, J.M. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect. Dis. 2006, 6, 641–652.
- The Joint Commission. Measuring Hand Hygiene Adherence: Overcoming the Challenges; Joint Commission: Oakbrook Terrace, IL, USA, 2009.
- Ekwere, T.; Okafor, I. Hand hygiene knowledge and practices among healthcare providers in a tertiary hospital, south west, Nigeria. Int. J. Infect. Control 2013, 9, 1–10.
- Van De Mortel, T.F.; Kermode, S.; Progano, T.; Sansoni, J. A comparison of the hand hygiene knowledge, beliefs and practices of Italian nursing and medical students. J. Adv. Nurs. 2012, 68, 569–579.
- Kim, S.A.; Rhee, M.S. Microbicidal effects of plain soap vs triclocarban-based antimicrobial soap. J. Hosp. Infect. 2016, 94, 276–280.
- Lin, Q.; Lim, J.; Xue, K.; Yew, P.Y.M.; Owh, C.; Chee, P.L.; Loh, X.J. Sanitizing agents for virus inactivation and disinfection. View 2020, 1, e16.
- U.S. Food&Drug Administration. FDA issues final rule on safety and effectiveness of antibacterial soaps. In Rule Removes Triclosan and Triclocarban from over-the-counter Antibacterial Hand and Body Washes. Available online: https://www.fda.gov/news-events/press-announcements/fda-issues-final-rule-safety-and-effectiveness-antibacterial-soaps (accessed on 20 February 2021).
- Kaiser, N.; Klein, D.; Karanja, P.; Greten, Z.; Newman, J. Inactivation of chlorhexidine gluconate on skin by incompatible alcohol hand sanitizing gels. Am. J. Infect. Control 2009, 37, 569–573.
- Karpiński, T.M.; Szkaradkiewicz, A.K. Chlorhexidine—Pharmaco-biological activity and application. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 1321–1326.
- Golin, A.P.; Choi, D.; Ghahary, A. Hand sanitizers: A review of ingredients, mechanisms of action, modes of delivery, and efficacy against coronaviruses. Am. J. Infect. Control. 2020, 48, 1062–1067.
- Baier, C.; Albrecht, U.V.; Ebadi, E.; Vonberg, R.P.; Schilke, R. Knowledge about hand hygiene in the Generation Z: A questionnaire-based survey among dental students, trainee nurses and medical technical assistants in training. Am. J. Infect. Control 2020, 48, 708–712.
- Naqvi, S.G.Z.; Jaffar, N.; Zehra, S.A.; Ghani, R.; Ali, H. Correlation of Hand Hygiene Knowledge and Hand Decontamination Practices of Medical Students. J. Bahria Univ. Med. Dent. Coll. 2020, 10, 147–151.
- Ghazali, A.D.; Deilhes, E.; Thomas, J.; Laland, C.; Thévenot, S.; Richer, J.P.; Oriot, D. Impact of a simulation-based training in hand hygiene with alcohol-based hand rub in emergency departments. Infect. Control Hosp. Epidemiol. 2018, 39, 1347–1352.
- Nawab, T.; Mehnaz, S.; Abedi, A.J.; Safwi, S.R.; Khalique, N.; Ansari, M.A.; Khan, Z. KAP study of hand hygiene among medical and nursing students in a tertiary teaching hospital. IJSAR 2015, 2, 29–39.
- Huang, C.; Ma, W.; Stack, S. The hygienic efficacy of different hand-drying methods: A review of the evidence. Mayo Clin. Proc. 2012, 87, 791–798.
- Marcenac, P.; Kim, S.; Molinari, N.A. Knowledge, attitudes, and practices around hand drying in public bathrooms during the COVID-19 pandemic in the United States. Am. J. Infect. Control 2021, 49, 1186–1188.
- Kimmitt, P.T.; Redway, K.F. Evaluation of the potential for virus dispersal during hand drying: A comparison of three methods. J. Appl. Microbiol. 2016, 120, 478–486.
- Best, E.; Parnell, P.; Couturier, J. Environmental contamination by bacteria in hospital washrooms according to hand-drying method: A multi-centre study. J. Hosp. Infect. 2018, 100, 469–475.
- Suen, L.K.P.; Lung, V.Y.T.; Boost, M.V.; Au-Yeung, C.H.; Siu, G.K.H. Microbiological evaluation of different hand drying methods for removing bacteria from washed hands. Sci. Rep. 2019, 9, 13754.
More
