Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Jason Zhu and Version 1 by Steven Gudowski.
The telemedicine respiratory therapist (eRT) interventions were components of an evidence-based care bundle and included ventilator liberation protocols, low tidal volume protocols, tube patency, and an extubation checklist. In addition, the proactive rounding of patients, including ventilator checks, was included. An eRT service can support the bedside RT providers, effectively monitor best practice bundles, and carry out patient–ventilator assessments. It was effective in certain emergent situations and reduced the exposure of respiratory therapists (RTs) to COVID-19.
- PENN E-LERT®
- respiratory therapist
- telemedicine
- intensive care
1. Introduction
Respiratory distress and acute hypoxemic failure are the primary symptoms of COVID-19 pneumonia [1]. Patients often require frequent escalation and de-escalation of respiratory therapy as the disease trajectory is highly unpredictable and labor-intensive. Providers are at a high risk of exposure due to the high labor burden of COVID-19 patient care in combination with the aerosol-based spread of the illness [2,3,4,5][2][3][4][5]. The viral dose, virulence, and individual susceptibility determine the natural history of the disease [4]. The ideal way to limit exposure is by using appropriate personal protective equipment (PPE), but institutions have often faced shortages [4,6][4][6]. Furthermore, the pandemic nature of the growth of COVID-19 has further stressed the system by creating a bottleneck in the PPE supply and restricting available medical professionals due to SARS-CoV-2 exposure [7]. Respiratory therapists (RTs) are an integral part of the U.S. healthcare system that increases the capacity of the primary intensive care unit (ICU) teams [8]. COVID-19 presents unique challenges to this service [1,7,9][1][7][9]. Even under optimal conditions, COVID-19 generates time-consuming tasks due to the complexity of respiratory demise [1,10][1][10]. High demand for RT skills, coupled with frequent contact with patients in settings with suboptimal PPE, can lead to increased RT occupational exposure [4]. The latter increases the number of infected individuals and further stresses the system by removing much-needed experts from the care team. Moreover, the frequent movement of RTs in hospitals operating in a pandemic may lead to patient cross-infection via the RT [11].
Telemedicine experienced explosive growth during the COVID-19 pandemic [12,13][12][13]. Some of the key drivers have been flexible delivery of care, scalability, and protection of healthcare workers in one technologically mature solution [14]. While there is research on telemedicine extending the availability of critical care specialty physicians, there are limited data on how RTs using this technology could impact patient care [15]. Despite several studies and statements indicating that telemedicine is the most flexible tool to match demand and supply, no in-depth analysis has been performed on the real-time deployment of tele-ICU services.
2. eRT Service Healthcare Delivery Model
A total of 1548 interventions took place between 1 May 2020 and 31 May 2020, and 93.86% of the interventions were routinely related to the established workflows, 4.71% were urgent, and 0.26% were emergent. The majority of the interventions were related to RT deferring activities to eRT such as ventilator checks or compliance with best practice protocols (Figure 1A). Higher demand for eRT services occurred during weekends and nighttime hours (Figure 1B,C). The number of interventions somewhat trailed the demand from COVID-19 in the system.
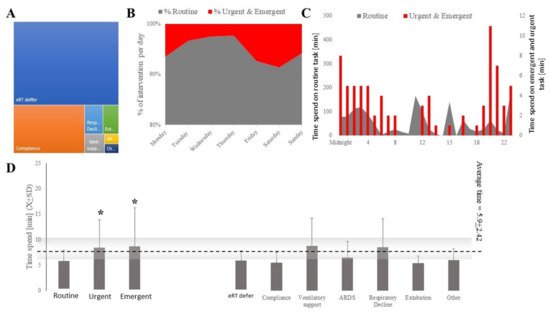
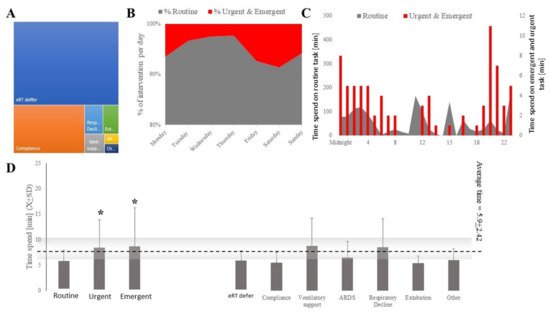
Figure 1. eRT interventions were mostly categorized as activities deferred from bedside or best practice compliance (A) and were more likely to occur during the weekend or at night (B,C). Less time was spent by eRT on routine tasks compared to those categorized as urgent or emergent (C,D). *, p < 0.0001.
The bulk of the interventions were triggered during proactive rounding (59.7%), site-triggered (23.4%), or by the teleICU staff (eTriage; 4.9%), directing the attention of an eRT to clinical problems (Table 1). There were statistically significant differences (H(2;1523) = 39.36; p < 0.00001) in times devoted to the tasks depending on the task’s expediency. The time spent on routine tasks (troutine = 5.8 ± 2.15) was the shortest, while urgent (turgent = 8.5 ± 5.38) and emergent (temergent = 8.8 ± 7.5) tasks took about the same amount of time but longer than routine tasks (Figure 3C). The average intervention took 5.97 ± 2.49 min, but it varied statistically by the different natures of each task (H(6;1525) = 89.89; p < 0.0001; Figure 3C,D). There were significant differences between the amounts of time spent by different eRTs on the tasks (H(6;1530) = 491.35; p < 0.000).
Table 1. Frequency of different sources for eRT interventions.
| Intervention | Total Count | % of Total | % Cumulative |
|---|---|---|---|
| Proactive rounding | 1024 | 59.67 | 59.67 |
| Site-trigger | 405 | 23.6 | 83.9 |
| eTriage | 84 | 4.89 | 88.81 |
| Sniffer/Dashboard Tool (ARDS, sepsis, etc.) | 11 | 0.6% | 88.81 |
| Push Button | 3 | 0.17% | 88.81 |
| Virtual consult | 1 | 0.1 | 89.04 |
| Other (place a note in Clinical Comment) | 1 | 0.1 | 89.10 |
| Missing | 187 | 10.89 | 100.0 |
In 16% of all the interventions, no communication with the bedside took place. The communication between eRTs and ICU-based RTs took place in 66.6% of all the interventions, followed by communication with house staff (9.8%), advanced practice providers (APP; 2.8%), and nurses (2.6%). Most communication involved a single provider at the bedside, but, in 2.6%, several stakeholders were involved. Most of the interactions took place over the telephone (88%), followed by secure text message (16%), audio-video communication via the teleICU module platform (1.7%), and the remaining were negligible (The eRT’s recommendation was followed in 92% of the cases. In 4% of the cases, they were only received, with the remaining 4% being missing data. The majority of the interventions involved deferring a routine ventilator assessment or assuring compliance of orders with ongoing ventilator settings (Figure 2). The clinical tasks focused on worsening respiratory status, extubation screens, and advanced ventilator management. Of note, ventilatory management or respiratory deterioration were deemed urgent or emergent in over 50% of the cases (Figure 2).
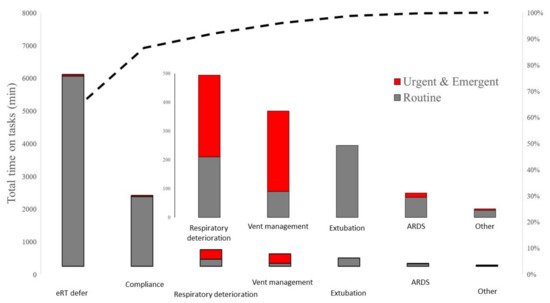
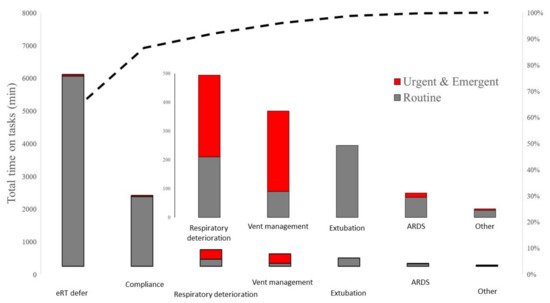
Figure 2. eRT spent the most time on activities that were deferred from RT, routine ventilator assessment and assuring compliance with best practice standards.
3. The Involvement of eRT Services with COVID-19 and Non-COVID-19 Patients
Seventy-four percent of the interventions were related to COVID (Figure 3A). The frequency of interventions was as expected, with a 54% vs. 46% ICU-bed type split between the COVID and non-COVID patients observed in this healthcare system. The average COVID-19-related burden was higher for all the eRT services in terms of time spent providing care to COVID-19 vs. non-COVID-19 patients (tCOVID-19 = 5.8 ± 2.25 vs. tCOVID-19 = 6.0 ± 3.05 U(166426) = −4.21; p < 0.0001). The time spent on different tasks was not different between the COVID and non-COVID-19 patients (Figure 3B).
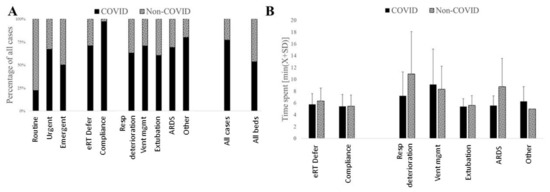
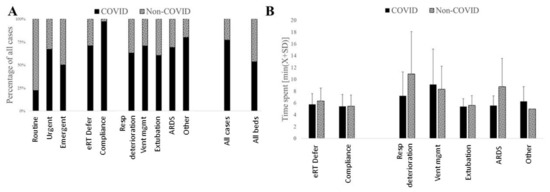
Figure 3. The majority of all eRT interventions were related to COVID-19 patients (A). Similarly, more time was spent by eRT when providing care to COVID-19 patients when compared to their non-COVID-19 counterparts. (B). Averting respiratory deterioration and supporting ventilator management in ARDS cases was the largest time spent in non-COVID-19 patients.
References
- Poston, J.T.; Patel, B.K.; Davis, A.M. Management of Critically Ill Adults With COVID-19. JAMA 2020, 323, 1839–1841.
- Barrett, E.S.; Horton, D.B.; Roy, J.; Gennaro, M.L.; Brooks, A.; Tischfield, J.; Greenberg, P.; Andrews, T.; Jagpal, S.; Reilly, N.; et al. Prevalence of SARS-CoV-2 infection in previously undiagnosed health care workers at the onset of the U.S. COVID-19 epidemic. BMC Infect. Dis. 2020, 20, 853.
- Lai, X.; Wang, M.; Qin, C.; Tan, L.; Ran, L.; Chen, D.; Zhang, H.; Shang, K.; Xia, C.; Wang, S.; et al. Coronavirus Disease 2019 (COVID-2019) Infection Among Health Care Workers and Implications for Prevention Measures in a Tertiary Hospital in Wuhan, China. JAMA Netw. Open 2020, 3, e209666.
- Chou, R.; Dana, T.; Buckley, D.I.; Selph, S.; Fu, R.; Totten, A.M. Epidemiology of and Risk Factors for Coronavirus Infection in Health Care Workers. Ann. Intern. Med. 2020, 173, 120–136.
- Benge, C.D.; Barwise, J.A. Aerosolization of COVID-19 and Contamination Risks During Respiratory Treatments. Fed. Pract. 2020, 37, 160–163.
- Petsonk, E.L.; Harber, P. Respiratory protection for health care workers: A 2020 COVID-19 perspective. Am. J. Ind. Med. 2020, 63, 655–658.
- Li, R.; Rivers, C.; Tan, Q.; Murray, M.B.; Toner, E.; Lipsitch, M. Estimated Demand for US Hospital Inpatient and Intensive Care Unit Beds for Patients with COVID-19 Based on Comparisons With Wuhan and Guangzhou, China. JAMA Netw. Open 2020, 3, e208297.
- Armaghan, R.; Geesey, B.; Juby, J.; Amador-Castaneda, J.; Bollinger, A.; Roberts, K.J.; Newberry, R.; Harshberger, M.; Radabaugh, N.; Pierce, M.; et al. Practice of Respiratory Therapists in Pennsylvania: A Statewide Survey. Respir. Care 2020, 65, 972–976.
- Registered Respiratory Therapist (RRT). 2020. Available online: https://www.nbrc.org/examinations/rrt/ (accessed on 1 June 2020).
- Higny, J.; Feye, F.; Foret, F. COVID-19 pandemic: Overview of protective-ventilation strategy in ARDS patients. Acta Clin. Belg. 2020, 76, 509–511.
- Kapoor, I.; Prabhakar, H.; Mahajan, C. Transference of COVID-19 patient in hospitals—A crucial phase. J. Clin. Anesth. 2020, 65, 109931.
- Srinivasan, S.R. Editorial: Tele-ICU in the Age of COVID-19: Built for This Challenge. J. Nutr. Health Aging 2020, 24, 536–537.
- Hollander, J.E.; Carr, B.G. Virtually Perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020, 382, 1679–1681.
- Lilly, C.M.; Greenberg, B. The Evolution of Tele-ICU to Tele-Critical Care. Crit. Care Med. 2020, 48, 610–611.
- Khunlertkit, A.; Carayon, P. Contributions of tele-intensive care unit (Tele-ICU) technology to quality of care and patient safety. J. Crit. Care 2013, 28, e311–e312.
More
