Avian orthoavulaviruses type-1 (AOaV-1) have transitioned from animal vaccine vector to a bona fide vaccine delivery vehicle in human. Owing to induction of robust innate and adaptive immune responses in mucus membranes in both birds and mammals, AOaVs offer an attractive vaccine against respiratory pathogens. The unique features of AOaVs include over 50 years of safety profile, stable expression of foreign genes, high infectivity rates in avian and mammalian hosts, broad host spectrum, limited possibility of recombination and lack of pre-existing immunity in humans. Additionally, AOaVs vectors allow the production of economical and high quantities of vaccine antigen in chicken embryonated eggs and several GMP-grade mammalian cell lines.
- avian orthoavulaviruses type-1
- human
- animal
- vaccines
1. Introduction
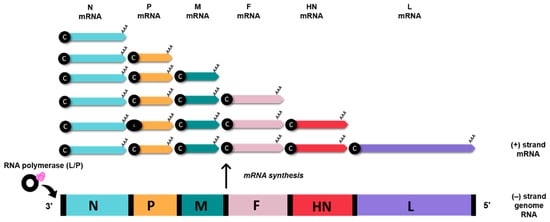
2. Genomic and Biological Features of Avian Orthoavulavirus Type-1
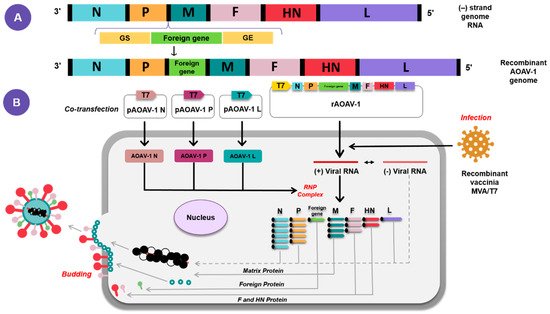
3. AOaV-1 as a Viral Vaccine Vector
4. Application of AOaV-1 as Vaccine Vector for Poultry and Animal Viruses
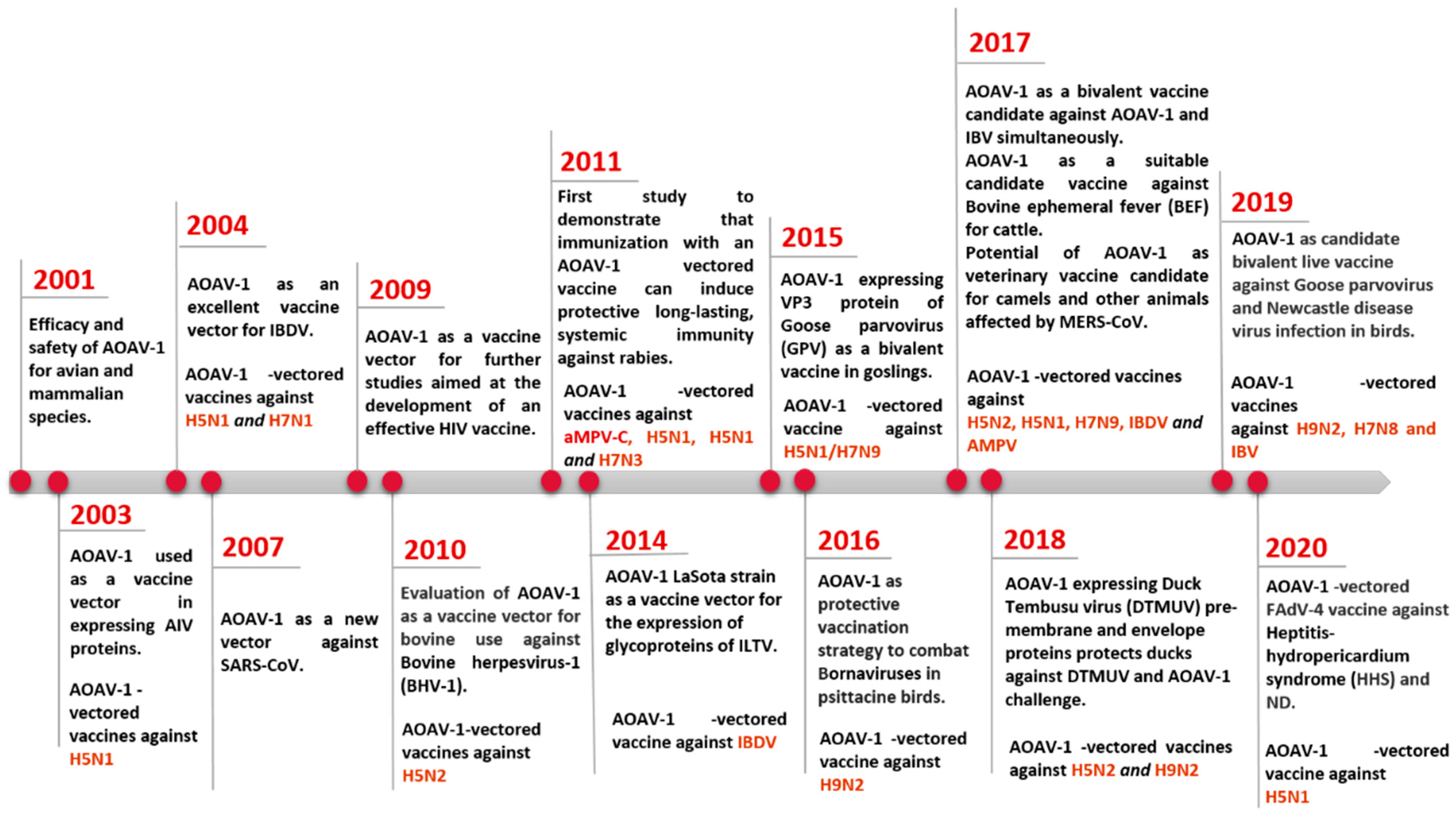
Efforts for studying the AOaV-1 as a viral vector have given rise to various vaccine candidates expressing antigens of various viral pathogens in poultry, animals, and humans [4][19]. Preclinical and clinical studies have been conducted to assess the safety, immunogenicity, and protective efficacy of these AOaV-1-vectored vaccines.5. Current Application of AOaV-1 as Vaccine Vector for Emerging and Remerging Human Viruses
Conventional vaccines have effectively reduced the burden for many infectious disease, i.e., small pox eradication and substantially controlling diseases such as polio, tetanus, diphtheria, and measles [25][84]. Live attenuated viruses, inactivated viruses, or recombinant subunit-based vaccines are traditional platforms for the development of vaccines, which often contribute to a long-term immunity of many infectious human and/or animal viruses. However, a majority of them are not suitable for human use due to safety concerns, poor efficacy, or easy impracticability, and are not always suitable or even feasible in outbreak situations [25][84]. Additionally, scenarios of outbreaks may limit the development and or productivity of conventional vaccines. A number of challenges need to be overcome to prove the efficacy of these conventional vaccines in the face of an emerging or future pandemic [25][84]. One of the key problems for pandemic preparedness is the unpredictable nature of emerging pathogens and zoonosis that poses a permanent threat to the population, as with SARS-CoV-2. SARS-CoV-2 outbreaks revealed the possibility of the known pathogens for mutations and adaptation to a new host or environment with impermissible consequences for their immunogenic properties and the seriousness of the symptoms they produce. The risk of such events is high in RNA viruses, whose high mutation rates favour adaptability, as demonstrated by recent epidemics and pandemics. Since the goals of the vaccine remain undefined before an outbreak, time remains an important obstacle to effective development of the vaccine. The average development time currently exceeds 10 years for conventional preclinical vaccines [26][85], highlighting the dire need for new approaches which permit extremely rapid development and licencing to prevent the emerging outbreak from spreading worldwide. Another major problem is the cost of vaccine development and production; the development of a new vaccine candidate with established technologies is estimated to exceed USD 500 million with additional costs for setting up equipment and facilities between USD 50 million and 700 million [27][86]. Although some vaccine development costs cannot be avoided to meet the necessary safety standards, validation and production costs are high in every vaccine requirement for dedicated manufacturing processes and facilities in most conventional vaccine technologies. In addition, new technologies are required in order to support more cost-efficient vaccination production, particularly in light of resource limited environments and the fact that emergencies represent niche markets. The second problem is the manufacturing capacity of established methods, often inadequate for global vaccination. Although the potential threat is recognised, vaccine production technology, such as the COVID-19 vaccine, is still problematic in its production capacity to meet peak demands of a disease. An example is that the potential influenza pandemic vaccine production capacity could theatrically support vaccination of 43% of the population with two doses of the vaccine in 2015 through WHO efforts [28][87]. In 2015, only 5% of influenza vaccine doses were distributed to South-east Asia, the Eastern Mediterranean, and Africa in the WHO regions, which represent about half of the world’s population, but the distribution of vaccine products worldwide is far from equal between the developing and industrialised countries [29][88]. Moreover, most currently authorised vaccines would require 3–5 months from virus identification to the distribution of vaccines, providing the virus with ample time to spread globally. Therefore, in the event of pandemic risks, technology that allows quick manufacturing of a large number of vaccines is absolutely necessary. The use of recombinant vectors as a vaccination tool for human pathogens was therefore critical, due to their ability to express high-level foreign proteins in host cells, which leads to a strong, long-term immune response to the target protein. As AOaV-1 is an avian paramyxovirus, a major advantage of the vaccine platform is that the issue of anti-vector pre-existing immunity is not considered a major factor. Further, several AOaV-1 strains are licensed and readily available for use as veterinary vaccines. Although even small exogenous transgenes may significantly lower the yield of recombinant viruses, most recombinant AOaV-1 vectors can be propagated to high titers in chicken eggs and even some cell lines [17][7]. Recombinant AOaV-1 has also been used as a viral vector in the delivery of vaccine antigen for humans [30][89]. Currently, AOaV-1 vaccine candidates both respiratory and non-respiratory diseases include SARS-CoV-2 [24][31][14,90], SARS-CoV [32][91], EBOV [33][92], HIV-1 [6][34][15,30], HPAIV H5N1 [8][22], RSV [35][93], and HPIV-3 [3][18] (Table 13).| Pathogen | AOaV-1 Backbone | Antigen | Insert Site | Animal Model | Vaccination (Route) | References |
|---|---|---|---|---|---|---|
| HIV-1 | Hitchner B1 | Gag | P/M | Mouse | i.n. | [6][15] |
| HIV-1 | La Sota | Gag | P/M | Mouse | i.n. | [36][94] |
| HIV-1 | La Sota | Gag; Env; Gag + Env | Env- P/M and Gag- HN/L; Gag- O/M and Env- HN/L; Env + Gag- P/M; Env- P/M; Gag- P/M | Guinea pigs/Mouse | i.n. | [34][30] |
| SIV | La Sota | gp160 | P/M | Guinea pigs/Mouse | i.n. | [37][95] |
| EBOV | Beaudette C and La Sota | GP | P/M | Rhesus monkeys | i.n/i.t. | [33][92] |
| EBOV | Chimeric AOaV-1 | GP | N/P, P/M, and M/F | Guinea pigs | i.n. | [38][96] |
| HPIV-3 | Beaudette C and La Sota | HN | P/M | African green monkeys and rhesus monkeys | i.n./i.t. | [3][18] |
| RSV | Hitchner B1 | F | P/M | Mouse | i.n. | [35][93] |
| Poliovirus | La Sota | P1 and 3CD | P1- P/M and 3CD- HN/L | Guinea pigs | i.n. | [39][97] |
| Lyme | LaSota/VF | BmpA + OspC | P/M | Hamsters | i.n./i.m./i.p. | [40][98] |
