Older adults with cancer are amongst the most vulnerable population to be negatively impacted by COVID-19 due to their likelihood of comorbidities and compromised immune status. Considering the longevity of the pandemic, understanding the subjective perceptions and psychosocial concerns of this population may help ameliorate the psychological aftermath. This review intended to analyse the literature surrounding the psychosocial impact and coping strategies among older adults with cancer within the context of COVID-19
- cancer
- older adults
- mixed methods
- COVID-19
- quality of life
- patient experience
- qualitative methods
1. Older adults with cancer and COVID-19
Older adults with cancer and COVID-19
Nearly two years into the COVID-19 pandemic, it continues to impact individuals’ lives and health systems globally. This is particularly true of older adults with cancer, who may be among the most vulnerable to the effects of COVID-19 due to their immunocompromised status and increased presence of comorbidities[1][2][3][4][5]. Older adults diagnosed with both cancer and COVID-19 face increased mortality, hospitalization, and ICU admission [3][4][5]. In addition, the COVID-19 pandemic has caused significant disruption to the cancer care system, including a shift to virtual appointments, alternative treatment offerings, postponement of surveillance scans and surgeries, and diminished supportive care and survivorship services[6][7]. Older adult cancer survivors have described barriers to cancer treatment across the pandemic, including restricted attendance of caregivers at appointments, diminished access to healthcare services, and feeling less connected to their healthcare team[8][9]. Understanding the impact of these changes on the experiences of older adults with cancer is essential to learning how best to support older adults during this time.
2. Need for Understanding the Impact of COVID-19
Need for Understanding the Impact of COVID-19
Public health measures meant to diminish the spread of COVID-19, such as social distancing and stay-at-home mandates, have resulted in older adults spending more time alone, which may enhance feelings of isolation and loneliness. Recent reviews suggest that COVID-19 has created considerable anxiety, irritability, feelings of paranoia, and depression amongst community-dwelling older adults and people with serious comorbidities[10]. In the face of the COVID-19 pandemic, older adults with cancer face intersecting vulnerabilities related to the physical effects of the virus, cancer-system changes, and the potentially isolating impacts of public health measures. These factors may be experienced differently by older adults with cancer, potentially exacerbating the impact of the COVID-19 pandemic on this patient population. With no clear ending of the COVID-19 pandemic in sight, understanding the psychosocial impact of the COVID-19 pandemic on older adults with cancer is crucial to provide patient- and family-centred care to this patient population.
3. Psychosocial Impact of COVID- 19 in Older Adults with Cancer
Psychosocial Impact of COVID- 19 in Older Adults with Cancer
The purpose of this review was to synthesize the literature surrounding the psychosocial impact and coping strategies of older adults with cancer during the COVID-19 pandemic. Understanding how the pandemic has impacted older adults with cancer will help clinicians support them during subsequent waves of this pandemic, as well as plan for future pandemics. The results from the included studies were consolidated under four domains: (1) Impact of COVID-19 on Quality of Life, (2) Concerns related to COVID-19, (3) Coping with the impact of COVID-19, and (4) Recommendations for future care. The following figure illustrate the finings. Numerous factors such as, being younger than 60 years of age [11]; being a woman[12]; having several co-morbidities[11][13]; receiving active treatment, especially oral therapies [11][14]; and living in city apartments[11][12] were associated with poorer psychosocial wellbeing and increased fears and concerns towards COVID-19. Based on the results of the review, older adults were concerned by changes in their cancer care, loneliness, their disease progression, and contracting the coronavirus. Coping strategies included leaning on personal relationships, maintaining spirituality, accepting the changes associated with the pandemic, engaging in positive interpretation, and drawing on previous experience.
Figure 1 contains a visual presentation of the psychosocial impact of COVID-19 on older adults with cancer, including the factors associated with reduced QoL, major concerns amongst the population, and the adopted coping strategies.
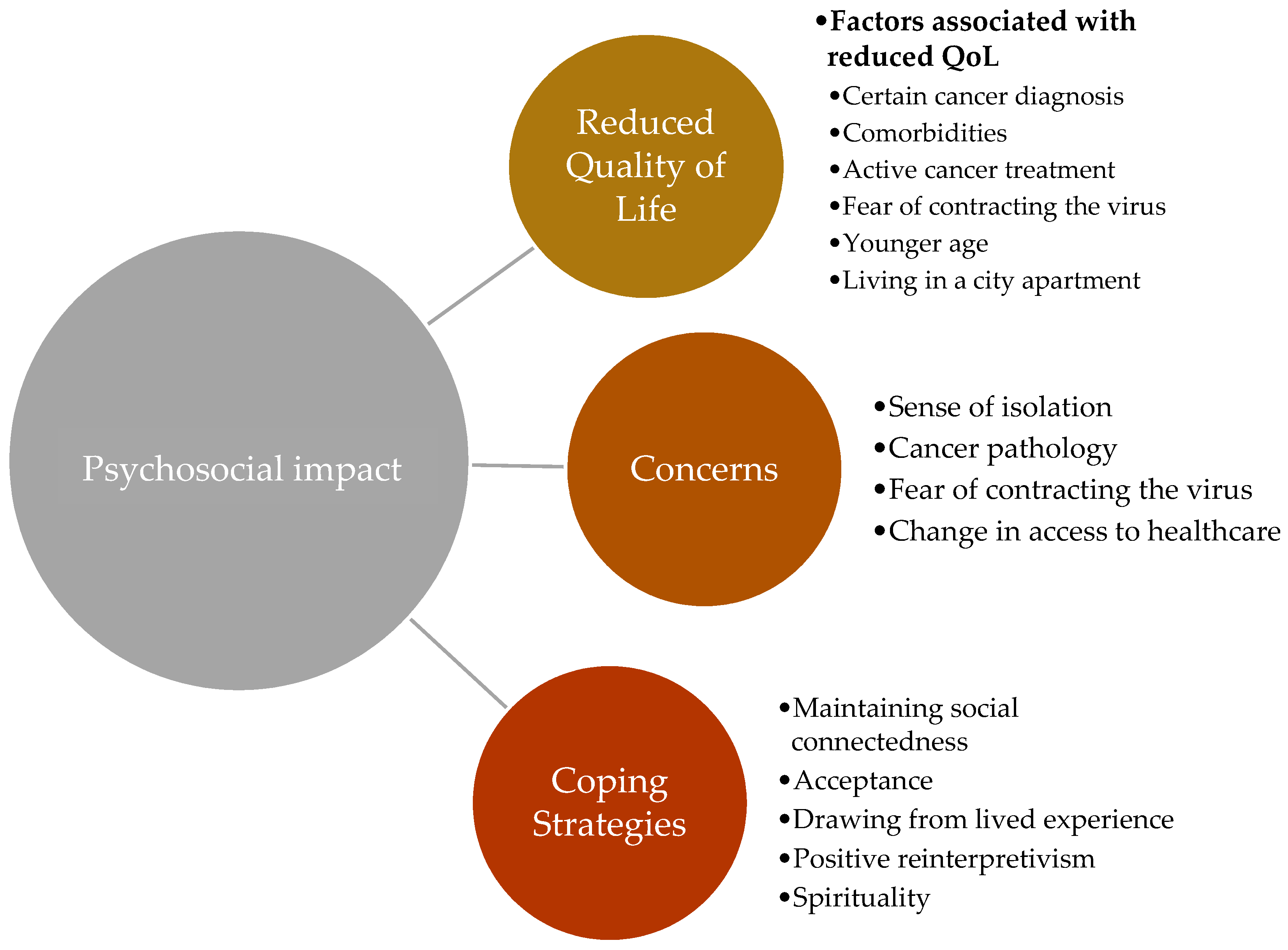
Figure 1. Psychosocial Impact of COVID-19 among older adults with cancer.
References
- Nicole M Kuderer; Toni K Choueiri; Dimpy P Shah; Yu Shyr; Samuel M Rubinstein; Donna R Rivera; Sanjay Shete; Chih-Yuan Hsu; Aakash Desai; Gilberto De Lima Lopes; et al.Petros GrivasCorrie A PainterSolange PetersMichael A ThompsonZiad BakounyGerald BatistTanios Bekaii-SaabMehmet A BilenNathaniel BouganimMateo Bover LarroyaDaniel CastellanoSalvatore A Del PreteDeborah B DoroshowPamela C EganArielle ElkriefDimitrios FarmakiotisDaniel FloraMatthew D GalskyMichael J GloverElizabeth A GriffithsAnthony P GulatiShilpa GuptaNavid HafezThorvardur R HalfdanarsonJessica E HawleyEmily HsuAnup KasiAli R KhakiChristopher A LemmonColleen LewisBarbara LoganTyler MastersRana R McKayRuben A MesaAlicia K MorgansMary F MulcahyOrestis A PanagiotouPrakash PeddiNathan A PennellKerry ReynoldsLane R RosenRachel RosovskyMary SalazarAndrew SchmidtSumit A ShahJustin A ShayaJohn SteinharterKeith E Stockerl-GoldsteinSuki SubbiahDonald C VinhFiras H WehbeLisa B WeissmannJulie Tsu-Yu WuElizabeth Wulff-BurchfieldZhuoer XieAlbert YehPeter P YuAlice Y ZhouLeyre ZubiriSanjay MishraGary H LymanBrian I RiniJeremy L WarnerMaheen AbidiJared D. AcobaNeeraj AgarwalSyed AhmadArchana AjmeraJessica AltmanAnne H. AngevineNilo AzadMichael H. BarAditya BardiaJill Barnholtz-SloanBriana BarrowBabar BashirRimma BelenkayaStephanie BergEric H. BernickerChristine BestvinaRohit BishnoiGenevieve BolandMark BonnenGabrielle BouchardDaniel W. BowlesFiona BusserAngelo CabalPaolo CaimiTheresa CarducciCarla CasuloJames L. ChenJessica M ClementDavid ChismErin CookCatherine CurranAhmad DaherMark DaileySaurabh DahiyaJohn DeekenGeorge D. DemetriSandy DiLulloNarjust DumaRawad EliasBryan FallerLeslie A. FecherLawrence E. FeldmanChristopher R. FriesePaul FuJulie FuAndy FutrealJustin GainorJorge GarciaDavid M. GillErin A. GillaspieAntonio Giordano(Mary) Grace GlaceAxel GrotheyShuchi GulatiMichael GurleyBalazs HalmosRoy HerbstDawn HershmanKent HoskinsRohit K. JainSalma JabbourAlokkumar JhaDouglas B. JohnsonMonika JoshiKaitlin KelleherJordan KharofaHina KhanJeanna KnobleVadim S. KoshkinAmit A. KulkarniPhilip E. LammersJohn C. LeightonMark A. LewisXuanyi LiAng LiK.M. Steve LoArturo Loaiza-BonillaPatricia LoRussoClarke A. LowMaryam B. LustbergDaruka MahadevanAbdul-Hai MansoorMichelle MarcumMerry Jennifer MarkhamCatherine Handy MarshallSandeep H. MashruSara MatarChristopher McNairShannon McWeeneyJanice M. MehnertAlvaro MenendezHarry MenonMarcus MessmerRyan MonahanSarah MushtaqGayathri NagarajSarah NagleJarushka NaidooJohn M. NakayamaVikram NarayanHeather H. NelsonEneida R. NemecekRyan NguyenPier Vitale NuzzoPaul E. ObersteinAdam J. OlszewskiSusie OwenbyMary M. PasquinelliJohn PhilipSabitha PrabhakaranMatthew PucAmelie RamirezJoerg RathmannSanjay G. RevankarYoung Soo RhoTerence D. RhodesRobert L. RiceGregory J. RielyJonathan RiessCameron RinkElizabeth V. RobilottiLori RosensteinBertrand RoutyMarc A. RovitoM. Wasif SaifAmit SanyalLidia SchapiraCandice SchwartzOscar SerranoMansi ShahChintan ShahGrace ShawArdaman ShergillGeoffrey ShouseHeloisa P. SoaresCarmen C. SolorzanoPramod K. SrivastavaKaren StaufferDaniel StoverJamie StrattonCatherine StrattonVivek SubbiahRulla TamimiNizar M. TannirUmit TopalogluEli Van AllenSusan Van LoonKaren Vega-LunaNeeta VenepalliAmit K. VermaPraveen VikasSarah WallPaul L. WeinsteinMatthias WeissTrisha Wise-DraperWilliam A. WoodWenxin (Vincent) XuSusan YackzanRosemary ZacksTian ZhangAndrea ZimmerJack West Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. The Lancet 2020, 395, 1907-1918, 10.1016/s0140-6736(20)31187-9.
- Lennard Yw Lee; Jean-Baptiste Cazier; Vasileios Angelis; Roland Arnold; Vartika Bisht; Naomi A Campton; Julia Chackathayil; Vinton Wt Cheng; Helen M Curley; Matthew W Fittall; et al.Luke Freeman-MillsSpyridon GennatasAnshita GoelSimon HartleyDaniel J HughesDavid KerrAlvin Jx LeeRebecca J LeeSophie E McGrathChristopher P MiddletonNirupa MurugaesuThomas Newsom-DavisAlicia Fc OkinesAnna C Olsson-BrownClaire PallesYi PanRuth PettengellThomas PowlesEmily A ProtheroeKarin PurshouseArchana Sharma-OatesShivan SivakumarAshley J SmithThomas StarkeyChris D TurnbullCsilla VárnaiNadia YousafRachel KerrGary Middleton COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. The Lancet 2020, 395, 1919-1926, 10.1016/s0140-6736(20)31173-9.
- Wenhua Liang; Weijie Guan; Ruchong Chen; Wei Wang; Jianfu Li; Ke Xu; Caichen Li; Qing Ai; Weixiang Lu; Hengrui Liang; et al.Shiyue LiJianxing He Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. The Lancet Oncology 2020, 21, 335-337, 10.1016/s1470-2045(20)30096-6.
- Yehong Tian; Xiaowei Qiu; Chengxiang Wang; Jianxin Zhao; Xin Jiang; Wenquan Niu; Jin-Chang Huang; Fengyu Zhang; Cancer Associates with Risk and Severe Events of COVID-19: A Systematic Review and Meta-Analysis. SSRN Electronic Journal 2020, 148, 363–374, 10.2139/ssrn.3612074.
- Anthony Harries; Kudakwashe C Takarinda; Faculty Opinions recommendation of Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention.. Faculty Opinions – Post-Publication Peer Review of the Biomedical Literature 2020, 323, 1239–1242, 10.3410/f.737420993.793572382.
- Debra Patt; Lucio Gordan; Michael Diaz; Ted Okon; Lance Grady; Merrill Harmison; Nathan Markward; Milena Sullivan; Jing Peng; Anan Zhou; et al. Impact of COVID-19 on Cancer Care: How the Pandemic Is Delaying Cancer Diagnosis and Treatment for American Seniors. JCO Clinical Cancer Informatics 2020, 4, 1059-1071, 10.1200/cci.20.00134.
- Gianluca Vanni; Giovanni Tazzioli; Marco Pellicciaro; Marco Materazzo; Orsaria Paolo; Francesca Cattadori; Francesca Combi; Simona Papi; Chiara Adriana Pistolese; Maria Cotesta; et al.Francesca SantoriJonathan CaspiAgostino ChiaravallotiSaverio MuscoliVittorio LombardoAntonella GrassoLorenza CaggiatiRoberta RaselliDante PalliVittorio AltomareRolando Maria D’AngelilloLeonardo PalombiOreste Claudio Buonomo Delay in Breast Cancer Treatments During the First COVID-19 Lockdown. A Multicentric Analysis of 432 Patients. Anticancer Research 2020, 40, 7119-7125, 10.21873/anticanres.14741.
- Larissa Nekhlyudov; Saskia Duijts; Shawna V Hudson; Jennifer M Jones; Justin Keogh; Brad Love; Maryam Lustberg; Katherine Clegg Smith; Amye Tevaarwerk; Xinhua Yu; et al.Michael Feuerstein Addressing the needs of cancer survivors during the COVID-19 pandemic.. null 2020, 14, 1–6.
- Jessica L. Krok-Schoen; Janell L. Pisegna; Karlynn BrintzenhofeSzoc; Amy R. MacKenzie; Beverly Canin; Elana Plotkin; Leigh M. Boehmer; Armin Shahrokni; Experiences of healthcare providers of older adults with cancer during the COVID-19 pandemic. Journal of Geriatric Oncology 2020, 12, 190-195, 10.1016/j.jgo.2020.09.021.
- Souvik Dubey; Payel Biswas; Ritwik Ghosh; Subhankar Chatterjee; Mahua Jana Dubey; Subham Chatterjee; Durjoy Lahiri; Carl J. Lavie; Psychosocial impact of COVID-19. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 2020, 14, 779-788, 10.1016/j.dsx.2020.05.035.
- M. M. T. J. Bartels; R. Gal; J. M. van der Velden; J. J. C. Verhoeff; J. J. Verlaan; H. M. Verkooijen; Impact of the COVID-19 pandemic on quality of life and emotional wellbeing in patients with bone metastases treated with radiotherapy: a prospective cohort study. Clinical & Experimental Metastasis 2021, 38, 209-217, 10.1007/s10585-021-10079-x.
- Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies . National Heart, Lung, and Blood Institute. Retrieved 2022-2-22
- Stefan S. Jeppesen; Kristian K. Bentsen; Trine L. Jørgensen; Hanne S. Holm; Linda Holst-Christensen; Line S. Tarpgaard; Rikke H. Dahlrot; Lise Eckhoff; Quality of life in patients with cancer during the COVID-19 pandemic – a Danish cross-sectional study (COPICADS). Acta Oncologica 2020, 60, 4-12, 10.1080/0284186x.2020.1830169.
- Arndt Büssing; Jutta Hübner; Stefanie Walter; Wolfgang Gießler; Jens Büntzel; Tumor Patients´ Perceived Changes of Specific Attitudes, Perceptions, and Behaviors Due to the COVID-19 Pandemic and Its Relation to Reduced Wellbeing. Frontiers in Psychiatry 2020, 11, 574314, 10.3389/fpsyt.2020.574314.
