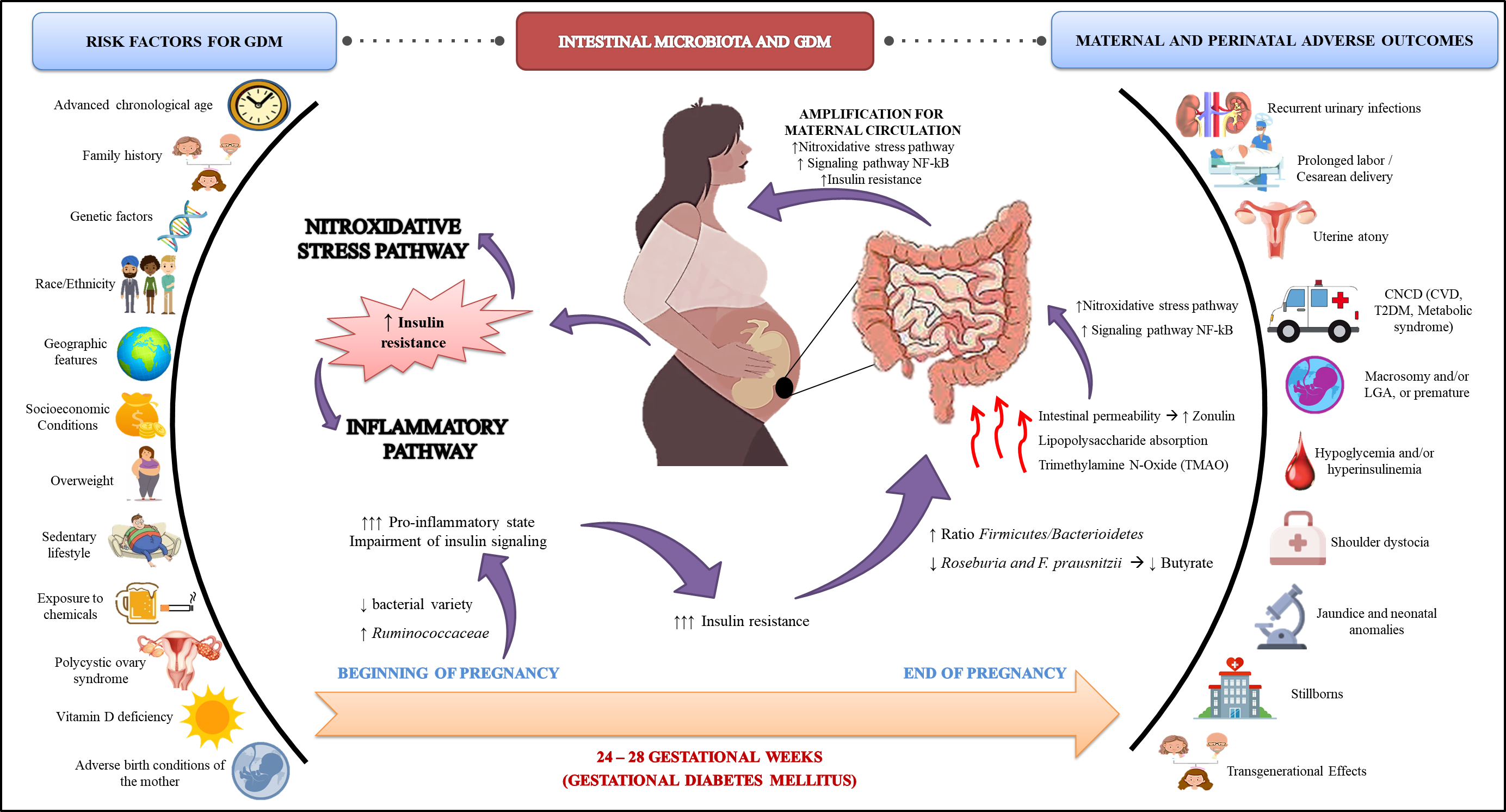
Gestational diabetes mellitus (GDM) is characterized by a set of metabolic complications arising from adaptive failures to the pregnancy period. Estimates point to a prevalence of 3 to 15% of pregnancies. Its etiology includes intrinsic and extrinsic aspects the progenitress, which may contribute to the pathophysiogenesis of GDM. Recently, researchers have identified that the intestinal microbiota participates in the development of the disease, both through its influence on insulin resistance, as well as on pro-oxidant and pro-inflammatory products, which are potentially harmful to the health of the maternal-fetal binomial, in the short and long term.In this context, our objective was to gather evidence on the modulation of the intestinal microbiota, through the use of probiotics and prebiotics, with antioxidant and anti-inflammatory properties, which can mitigate the endogenous processes of GDM, favoring the health of the mother and her children and , in a future perspective, to alleviate this critical public health problem.
- pregnancy
- dysbiosis
- Gestational diabetes mellitus
1. Gestational Diabetes Mellitus
1. Diabetes Mellitus Gestacional
| Global Prevalence | Prevalence by Region |
| Criteria | |||||
| Time Course | |||||
| Fasting Glucose (mg/dL) | |||||
| Glucose Overload | |||||
| Oral Glucose Tolerance Test (mg/dL) | |||||
| Hyperglycemia in pregnancy | 16.2% | Africa | |||
| 1 h | |||||
| 2 h | |||||
| 3 h | 10.4% | ||||
| Western Pacific | 12.6% | ||||
| O’Sullivan & Mahan (1964) | |||||
| [5] | |||||
| Detected at any time during pregnancy | 90 | 100 g of glucose | 165 | ||
| [15] | 24-28 gestational weeks |
92 | 75 g de glucose |
180 | 153 |
1.2. 1.2. Etiology
| Risk Factor | Mechanism of Action | Reference | |||||
| Advanced chronological age | (>35 years old) |
|
|
[23] | [25][26] | [24] | |
| Family history |
|
|
[2514][2615] | ||||
| 145 | 125 | ||||||
| South America and Central America | |||||||
| O’Sullivan & Mahan (1964) | |||||||
| 13.1% | |||||||
| [5] | |||||||
adapted by National Diabetes Data Group (NDDG) (1979) | |||||||
| [6] | |||||||
| 105 | 100 g of glucose | 190 | 165 | 145 | |||
| Genetic factors |
|
|
North America and Caribbean | 14.6% | |||
| Carpenter & Coustan (1982) | |||||||
| [7] | |||||||
| 95 | 100 g of glucose | 180 | 155 | ||||
| Europe | 16.2% | ||||||
| Middle East and North Africa | 21.8% | ||||||
| South East Asia | 24.2% | ||||||
| Source: Adapted from International Diabetes Federation [3]. | |||||||
1.1. Screening and Diagnosis
| 140 | |||||||||
|
|
|
[25][26] | [40 | [27] | ,41,42] | |||
|
|
[25][27][28] | |||||||
| World Health Organization (WHO) (1999) [10] | |||||||||
| Race/ | 126 | Ethnicity |
|
| 75 g of Glucose |
Not measured |
140 | Not measured |
|
| World Health Organization (WHO) (1999) [14] | 126 | ||||||||
| |||||||||
| 75 g de | glucose | Not measured |
140 | ||||||
| [ | 29 | ] | [31][32] | ||||||
| Not | measured | ||||||||
| [ | 30 | ] | International Association of Diabetes in Pregnancy Study Group (IADPSG (2010) [11] | 24–28 gestational weeks |
92 | 75 g of Glucose |
180 | 153 | |
| International Association of Diabetes in Pregnancy Study Group (IADPSG (2010) | |||||||||
| Geographic features |
| [12][16] | |||||||
| Socio-economic |
| [3033][3134] | |||||||
| Overweight |
| [2035][3236] | |||||||
| [3337][3438] | ||||||||
| Westernized diet |
| [2239][3519] | |||||||
| Sedentary lifestyle |
| [3640][3741] | |||||||
| Exposure to chemicals |
| [3842][3922][4043][4120][4221][4323] | |||||||
| [4424][4525][4626] | ||||||||
| Polycystic Ovary Syndrome (POS) |
| [4728][4844] | |||||||
| Vitamin D Deficiency |
| [4929][5030] | |||||||
| Adverse birth conditions of the mother | (Fetal program) |
|
| [5131][5232][5345][5446][5547] |
1.3. Maternal and Perinatal Outcomes in the Gestational Diabetes Mellitus
26. Intestinal Microbiota and GDM
| Source Sample | Population | Size * | Supplementation | Dose/Duration | Main Findings |
|---|---|---|---|---|---|
| Karamali et al. (2016) [94] | Iran | I: 30 C: 30 |
L. acidophilus + L. casei + B. bifidum | 2 × 109 CFU/ 6 weeks |
Supplementation with probiotics ↓FBG, serum insulin, TG, and VLDL-c, and improved insulin resistance indexes. |
| Hajifaraji et al. (2018) [91] | Iran | I: 27 C: 29 |
L. acidophilus LA-5 + B. BB-12 + S. thermophilus STY-31 + L. delbrueckii bulgaricus + LBY-27 | >4 × 109 CFU/ 8 weeks |
Supplementation with probiotics significantly ↓CRP and TNF-α. MDA, GPx and GR in women in the intervention group. |
| Kijmanawat et al. (2019) [95] | Thailand | I: 28 C: 29 |
Bifidobacterium + Lactobacillus | 2 × 109 CFU/ 4 weeks |
In women with diet-controlled GDM, supplementation with probiotics ↓FBG and insulin resistance compared with the control. |
| Babadi et al. (2018) [96] | Iran | I: 24 C: 24 |
L. casei + B. bifidum + L. fermentum + L. acidophilus | 2 × 109 CFU/ 6 weeks |
Probiotic supplementation improved the expression of genes related to insulin; glycemic control; inflammation; lipid profile, and oxidative stress markers, such as ↓MDA and ↑TAC, compared with the control. |
| Badehnoosh et al. (2018) [97] | Iran | I: 30 C: 30 |
L. acidophilus + L. casei + B. bifidum | 2 × 109 CFU/ 6 weeks |
Probiotic supplementation improved FBG, and CRP, ↑TAC, and ↓MDA, without affecting pregnancy outcomes. |
| Nabhani et al. (2018) [98] | Iran | I: 45 C: 45 |
L. acidophilus + L. plantarum + L. fermentum + L. gasseri + FOS | 1.5–7.0 × 109–10 CFU + 38.5 mg/ 6 weeks |
Symbiotics had no effect on FBG and insulin resistance/sensitivity indexes. However, an ↑ in HDL-c and TAC was seen, and a ↓ was seen in blood pressure in the intervention group. |
| Jamilian et al. (2019) [99] | Iran | I: 29 C: 28 |
L. acidophilus + B. bifidum + L. reuteri + L. fermentum + Vitamin D | 8 × 109 CFU/ 6 weeks +50.000 UI every 2 weeks |
↓FBG, serum insulin, CRP, and MDA; ↑TAC and GSH; and improved insulin resistance scores. |
| Karamali et al. (2018) [100] | Iran | I: 30 C: 30 |
L. acidophilus + L. casei + B. bifidum + Inulin | 2 × 109 CFU/ 6 weeks +800 mg |
Symbiotic supplementation ↓CRP and MDA; ↑TAC and GSH; and↓ the rates of cesarean section, hyperbilirubinemia and hospitalization in NB, without affecting other pregnancy outcomes. |
| Ahmadi et al. (2016) [101] | Iran | I: 35 C: 35 |
L. acidophilus + L. casei + B. bifidum + inulin | 2 × 109 CFU/ 6 weeks +800 mg |
Symbiotics ↑ insulin metabolism markers, and the insulin sensitivity index as well as ↓VLDL-c and TG. |
| Jafarnejad et al. (2016) [102] | Iran | I: 41 C: 41 |
S. thermophilus + B. breve + B. longum + B. infantis + L. acidophilus + L. plantarum + L. paracasei + L. delbrueckii subsp. Bulgaricus | 15 × 109 CFU/ 8 weeks |
No differences were observed in FBG, glycated hemoglobin, serum insulin, and insulin resistance indices. However, ↓CRP, IL-6, and TNF-α were observed, without changes in IL-10 and IFN-γ. |
| Dolatkhah et al. (2015) [103] | Turkey | I: 29 C: 27 |
L. acidophilus LA-5 + B. BB-12 + Streptococcus thermophilus + STY-31 + L. delbrueckii bulgaricus LBY-27 | >4 × 109 CFU/ 8 weeks |
↓FBG and insulin resistance index, and less weight gain in those in the intervention group. |
| Lindsay et al. (2015) [104] | Ireland | I: 74 C: 75 |
L. salivarius | 1 × 109 CFU/ 6 weeks |
No beneficial effect on glycemic control or pregnancy outcomes. ↓ in total and LDL-c in the supplemented group. |
| Source Sample | Population | Size * | Supplementation | Dose/Duration | Main Findings |
|---|---|---|---|---|---|
| Karamali et al. (2016) [86] | Iran | I: 30 C: 30 |
L. acidophilus + L. casei + B. bifidum | 2 × 109 CFU/ 6 weeks |
Supplementation with probiotics ↓FBG, serum insulin, TG, and VLDL-c, and improved insulin resistance indexes. |
| Hajifaraji et al. (2018) [83] | Iran | I: 27 C: 29 |
L. acidophilus LA-5 + B. BB-12 + S. thermophilus STY-31 + L. delbrueckii bulgaricus + LBY-27 | >4 × 109 CFU/ 8 weeks |
Supplementation with probiotics significantly ↓CRP and TNF-α. MDA, GPx and GR in women in the intervention group. |
| Kijmanawat et al. (2019) [87] | Thailand | I: 28 C: 29 |
Bifidobacterium + Lactobacillus | 2 × 109 CFU/ 4 weeks |
In women with diet-controlled GDM, supplementation with probiotics ↓FBG and insulin resistance compared with the control. |
| Babadi et al. (2018) [88] | Iran | I: 24 C: 24 |
L. casei + B. bifidum + L. fermentum + L. acidophilus | 2 × 109 CFU/ 6 weeks |
Probiotic supplementation improved the expression of genes related to insulin; glycemic control; inflammation; lipid profile, and oxidative stress markers, such as ↓MDA and ↑TAC, compared with the control. |
| Badehnoosh et al. (2018) [89] | Iran | I: 30 C: 30 |
L. acidophilus + L. casei + B. bifidum | 2 × 109 CFU/ 6 weeks |
Probiotic supplementation improved FBG, and CRP, ↑TAC, and ↓MDA, without affecting pregnancy outcomes. |
| Nabhani et al. (2018) [90] | Iran | I: 45 C: 45 |
L. acidophilus + L. plantarum + L. fermentum + L. gasseri + FOS | 1.5–7.0 × 109–10 CFU + 38.5 mg/ 6 weeks |
Symbiotics had no effect on FBG and insulin resistance/sensitivity indexes. However, an ↑ in HDL-c and TAC was seen, and a ↓ was seen in blood pressure in the intervention group. |
| Jamilian et al. (2019) [91] | Iran | I: 29 C: 28 |
L. acidophilus + B. bifidum + L. reuteri + L. fermentum + Vitamin D | 8 × 109 CFU/ 6 weeks +50.000 UI every 2 weeks |
↓FBG, serum insulin, CRP, and MDA; ↑TAC and GSH; and improved insulin resistance scores. |
| Karamali et al. (2018) [92] | Iran | I: 30 C: 30 |
L. acidophilus + L. casei + B. bifidum + Inulin | 2 × 109 CFU/ 6 weeks +800 mg |
Symbiotic supplementation ↓CRP and MDA; ↑TAC and GSH; and↓ the rates of cesarean section, hyperbilirubinemia and hospitalization in NB, without affecting other pregnancy outcomes. |
| Ahmadi et al. (2016) [93] | Iran | I: 35 C: 35 |
L. acidophilus + L. casei + B. bifidum + inulin | 2 × 109 CFU/ 6 weeks +800 mg |
Symbiotics ↑ insulin metabolism markers, and the insulin sensitivity index as well as ↓VLDL-c and TG. |
| Jafarnejad et al. (2016) [94] | Iran | I: 41 C: 41 |
S. thermophilus + B. breve + B. longum + B. infantis + L. acidophilus + L. plantarum + L. paracasei + L. delbrueckii subsp. Bulgaricus | 15 × 109 CFU/ 8 weeks |
No differences were observed in FBG, glycated hemoglobin, serum insulin, and insulin resistance indices. However, ↓CRP, IL-6, and TNF-α were observed, without changes in IL-10 and IFN-γ. |
| Dolatkhah et al. (2015) [95] | Turkey | I: 29 C: 27 |
L. acidophilus LA-5 + B. BB-12 + Streptococcus thermophilus + STY-31 + L. delbrueckii bulgaricus LBY-27 | >4 × 109 CFU/ 8 weeks |
↓FBG and insulin resistance index, and less weight gain in those in the intervention group. |
| Lindsay et al. (2015) [96] | Ireland | I: 74 C: 75 |
L. salivarius | 1 × 10 9 UFC/ 6 semanas |
Nenhum efeito benéfico no controle glicêmico ou resultados da gravidez. ↓ no total e LDL-c no grupo suplementado. |
