You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 1 by Giulio Cocco and Version 2 by Beatrix Zheng.
Post-COVID-19 vaccine administration lymphadenopathies in an atypical location represent an intense immune response to antigenic stimuli and they may show alarming US traits superimposed on malignant pathologies, which may complicate the patient’s clinical and diagnostic pathway. Despite no distinctive US features between reactive post-COVID-19 vaccination and malignant lymph nodes being available, careful examination of atypical lymph node locations associated with accurate knowledge of patients’ clinical background and delay of US exam to four to six weeks after vaccine injection should be considered.
- lymphadenopathy
- atypical sites
- anti-COVID-19 vaccine
- ultrasound
1. Introduction
SARS-CoV-2, a virus of the family of Betacoronaviridae, is the etiological agent of COVID-19 disease, a severe illness with the first official case described in December 2019 in Wuhan, China, and currently verified as being responsible for about 4.8 million deaths [1][2][1,2]. Symptoms and clinical manifestations are common to systemic diseases and include cough, dyspnea, fever, anosmia, mild to severe pneumonitis with diffuse alveolar damage, and acute respiratory distress syndrome, potentially leading to death [3][4][3,4]. The progressive spread of SARS-CoV-2 all over the world, the related disease severity, and the impact on everyday life and economics have stimulated the development of vaccines with a high safety profile to limit the rising infection rates [5][6][5,6]. As it stands, different types of vaccines manufactured by pharmaceutical giants are now authorized for administration, including the best known BNT162b2, ChAdOx1, and RNA-1273 vaccines. Despite the rise of new SARS-CoV-2 variants, BNT162b2 seems to induce a powerful immune response comparable to that of the original virus [7]. The progressive increase in the number of people who have undergone vaccination has revealed common side effects associated with the procedure. Adverse events include fever, myalgias, pain at the injection site, hypercoagulability states, elevated risk of HSV infection, acute myocarditis, appendicitis, and a copious list of unconventional and usual reactions [5]. Post-COVID-19 vaccine lymphadenopathy is a common adverse event occurring in about 3–16% of patients regardless of the vaccine type administered [5]. Generally, lymph node enlargement involves axillary and/or supraclavicular nodal stations ipsilateral to the intramuscular injection site [8][9][10][11][12][13][14][8,9,10,11,12,13,14]. Ultrasound (US) examination is a first-line imaging modality for evaluating morphologic lymph nodes due to its common accessibility and clear depiction of soft tissues and superficial structures provided by high-frequency linear probes [12][13][12,13]. Ultrasound examination has already played a central role in the pandemic for the management of patients with pulmonary involvement and for the selection of those in need of chest computed tomography (CT) [14][15][16][14,15,16]. Sometimes, benign post-anti-COVID 19 vaccination lymphadenopathies may show “nonreactive” features and may mimic severe pathologies with poorer prognosis [12][13][12,13]. The diagnostic overlap between the US features of lymph node involvement in benign and malignant disease is extremely relevant in the follow-up of neoplastic patients [17][18][17,18]. In this setting, research into the peculiar characteristics associated with post-anti-COVID19 vaccine lymphadenopathy may allow the avoidance of worthless follow-up, expansive second-level diagnostic imaging, and invasive diagnostic procedures for selected patients. In this study, we describe the incidence and US features of post-anti-COVID-19 vaccine lymphadenopathies in atypical sites to clarify their potential role in patients’ diagnostic work-up and follow-up strategies.
2. Assessment After Anti-COVID-19 Vaccine
A total of 64 patients who had received at least the first dose of anti-COVID-19 vaccine were assessed (Table S1). The overall number of lymph nodes evaluated was 170 and 5/64 patients presented atypical lymphadenopathy locations (7.8%) along with common nodal involvement (axillary, supraclavicular) ipsilateral to vaccine injection (3 women and 2 men, 60% and 40%, respectively, among atypical sites). In detail, two patients presented an overall number of three lymph nodes (respectively 2 and 1) located in the infraclavicular station, one patient in the pectoralis major muscle (1 lymph node), one patient in the left arm (1 lymph node), and one patient in the nuchal site (1 lymph node). Atypical sites of post-anti-COVID-19 vaccine lymphadenopathy were mainly infraclavicular (2/6, 33.3%) and oval-shaped with a median size of 0.9 ± 0.2 cm. US features included a symmetric cortex with hilum evidence (4/6, 60%), vascular signal at SMI in both the hilar region and periphery of the lymph node (5/6, 83.3%), and a US elastography pattern resembling that of adjacent tissues (5/6, 83.3%). A single lymph node located in the nuchal site showed a prevalent hard pattern at US elastography (1/6, 16.7%) (Figure 1, Figure 2, Figure 3, Figure 4 and Figure 5). The median age of patients with lymphadenopathies in an atypical location was 23 years. The main type of vaccine associated with lymph node appearance in atypical sites was Moderna’s mRNA-1273 (60% of patients, 4/6 lymph nodes accounting for 66.7% among atypical locations), followed by the AstraZeneca ChAdOx1 vaccine and the Pfizer/BioNTech BNT162b2 mRNA vaccine at the same level (1 patient with 1 lymph node, respectively). The mean time of atypical lymph node appearance was 3 days after vaccine injection (±0.7 days), and the median time to lymphadenopathy resolution was 33.75 ± 6.6 days.
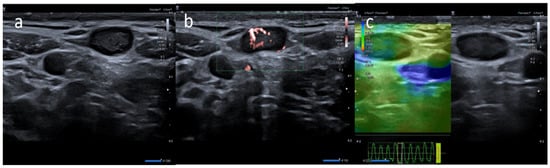

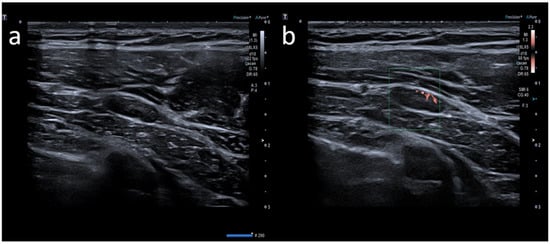
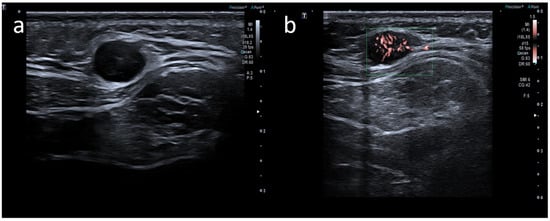
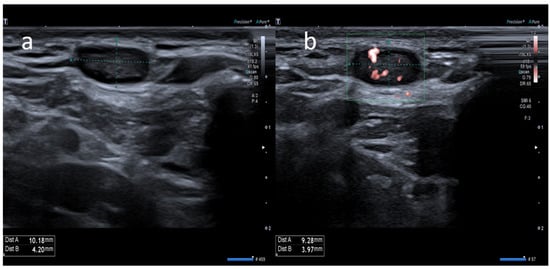
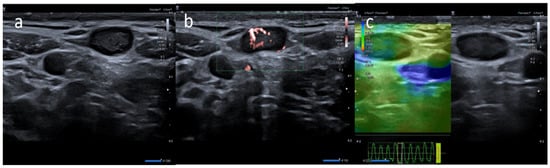
Figure 1. A 20-year-old male with palpable unilateral subclavicolar adenopathy noted three days after receiving the first dose of the Moderna COVID-19 vaccine in his left deltoid muscle. (a) B-mode sonogram image shows two ovalar hypoechoic lymph nodes with symmetric cortical thickening and hilum evidence. (b) SMI image shows central and peripheral vascularization. (c) Elastosonography strain shows a similar pattern of the node compared surrounding tissue.

Figure 2. (a) A 21-year-old male with unilateral left arm adenopathy (white arrow) noted four days after receiving the first dose of the Moderna COVID-19 vaccine in his left deltoid muscle. (b) B-mode sonogram image shows ovalar lymph node with asymmetric cortex and dislocate hilum. (c) SMI image shows central and peripheral vascularization.
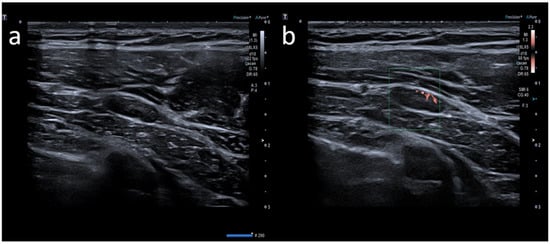
Figure 3. A 23-year-old female with pectoral swelling noted three days after receiving the first dose of the Pfizer COVID-19 vaccine in her left deltoid muscle. (a) B-mode sonogram image shows pectoral intramuscular ovalar hypoechoic lymph node with symmetric cortical thickening and hilum evidence. (b) SMI image shows central and peripheral vascularization.
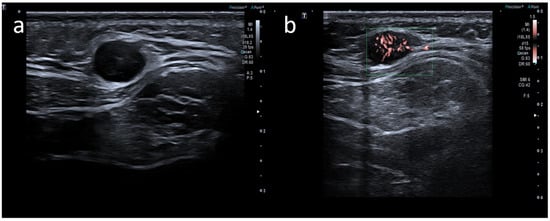
Figure 4. A 35-year-old male with palpable unilateral nuchal adenopathy noted three days after receiving the second dose of the Moderna COVID-19 vaccine in his left deltoid muscle. (a) B-mode sonogram image shows a lymph node ovalar hypoechoic with hilum absence. (b) SMI image shows central and peripheral vascularization.
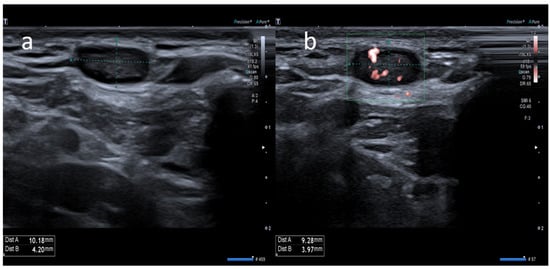
Figure 5. A 63-year-old female with palpable unilateral subclavicolar adenopathy noted four days after receiving the second dose of the AstraZeneca COVID-19 vaccine in her left deltoid muscle. (a) B-mode sonogram image shows ovalar hypoechoic lymph node with symmetric cortical thickening and hilum evidence. (b) SMI image shows central and peripheral vascularization.
3. Conclusions
Post-anti-COVID-19 lymphadenopathies may be in atypical locations ipsilateral to vaccine injection in association with the involvement of more common axillary and supraclavicular nodal stations. The atypical location, clinical appearance, and US features of post anti-COVID19 vaccine lymphadenopathies can sometimes simulate malignancy. Careful evaluation of the location of atypical lymphadenopathies should be considered in high-risk patients with a known history of neoplasia, to avoid misdiagnosis. A four- to six-week delay of US evaluation after anti-COVID-19 vaccine injection should be considered together with accurate knowledge of the patient’s clinical background.
