Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Dean Liu and Version 1 by Guowen Song.
Respiratory protective devices (RPDs) play a crucial role in controlling infection, particularly for viruses like SARS-CoV-2 that have a high transmission rate, strong viability, multiple infection routes and mechanisms, and emerging new variants that could reduce the efficacy of existing vaccines.
- respiratory protective device
- decontamination
- Respiratory Protection
1. Introduction
Respiratory protective devices (RPDs) play a crucial role in controlling infection, particularly for viruses like SARS-CoV-2 that have a high transmission rate, strong viability, multiple infection routes and mechanisms, and emerging new variants that could reduce the efficacy of existing vaccines.
2. RPD Performance, Issues, and Challenges
RPDs are designed to provide the wearer with a specific level of protection against a defined hazard [1]. Generally speaking, in the US, RPDs consist of various types of respirators that either require approval and certification by the National Institute for Occupational Safety and Health (NIOSH) [2] or medical/surgical masks that require clearance by the Food and Drug Administration (FDA) [3]. Face coverings such as homemade cloth masks, bandanas, and neck gaiters are not considered occupational PPE but fall into the RPD category during a pandemic [4][5].
Different types of RPDs provide different levels of preventive performance for different types of targeted hazards, such as dust and particulate matter (PM; e.g., asbestos or lead dust), fumes and smoke (e.g., metal fumes, soot), and mist or gas (e.g., chemical warfare gases, carbon monoxide) [1]. Atmosphere-supplying respirators supply clean air to the wearer when respirable air is absent or bio- or chemical hazards are present. In such cases, contaminated air is physically isolated from the human respiratory system [1]. By contrast, air-purifying respirators remove contaminants from ambient air by applying a filter. For example, FFRs are tightly fitting and utilize an integrated fibrous filtering piece to prevent the inhalation of contaminants [1]. FFRs are designed to prevent transmission of PM and aerosols to a certain extent (including droplets if they are surgical FFRs, e.g., surgical N95). Typically, they are designed to be used once only, as the filtering piece is embedded in a molded structure and cannot be replaced. FFRs are the most popular type of RPD due to their low cost, accessibility, quick production, and simple management [6][7].
Surgical masks are also designed to protect the wearer from droplets and particles and to maintain a sterile environment in a clinical setting. However, because surgical masks do not tightly fit the wearer’s face, potential leakage around the mask perimeter can reduce its protective performance against small particles [1]. Thus, surgical masks alone do not provide effective inward protection against bioaerosols [1]. However, they can significantly reduce outward leakage of droplets which makes them popular for source control as it reduces the spread of viruses [8][9].
Filtering media used in FFRs and surgical masks are typically made from polymeric materials with a fibrous structure [10], such as nonwoven substances with fine (µm) fiber sizes, high packing density, and electrostatically charged [10]. Polymers that can be processed using nonwoven procedures (e.g., spunbonding, melt-blowing, electrospinning) and those with high electrical resistance and stability are the best filter choices [10]. They include polypropylene, polyethylene, polyacrylonitrile, polycarbonate, polystyrene, polyester, polyamides, and polyphenylene oxide [10].
The most common structure for surgical masks is a three-ply spunbond-meltblown-spunbond (SMS) structure. The center meltblown polypropylene layer serves as the principal filtering media [6][7][10]. In contrast, FFRs have an SMS structure with an additional supportive layer, usually made of polyester or modacrylic, to give the mask its three-dimensional shape for optimal fit to the user’s face. Due to the low moisture absorbency of polypropylene microfiber and its nonwoven structure, the outer layer of surgical masks/FFRs is usually water-resistant and repels body fluids and droplets. The inner layer, with some treatment, can absorb some of the moisture released by the wearer to maintain comfort [6][7][10].
Unlike surgical masks or FFRs, face coverings used by the general public are made from various materials, designs, and structures. Currently, there are no specifications for face covering design or performance. Since the onset of the COVID-19 pandemic, efforts have gone into compiling guidelines on mask design and material selection for the general public that also include performance evaluation methods and requirements for manufacturers. For example, the American Association of Textile Chemists and Colorists (AATCC) developed a general guidance document for textile face coverings [11], and ASTM International is developing a standard specification for face coverings considering protection and comfort levels [12]. However, comfort level is loosely regulated by this ASTM standard, as only inhalation resistance, but no thermal comfort or moisture management properties are considered.
Evidence of pre-symptomatic and asymptomatic transmission of the SARS-CoV-2 virus [13][14][15][16][17] suggests that wearing face coverings can substantially reduce viral spread in a community. A recent simulation demonstrated that the spatial virus spread in an open, windy environment can considerably exceed the physical distancing requirements (currently 2 m) [18][19][20]. The use of face masks and coverings is encouraged and has been demonstrated to be effective for controlling disease transmission [21][22][23][24][25].
However, the effectiveness of RPDs can be affected by various factors. Filtration efficiency depends on the nature of the hazard, the environmental conditions, as well as the type of filter material and structure. Its protective performance also depends on the facepiece fit and seal while various user and usage factors affect comfort (Figure 2).
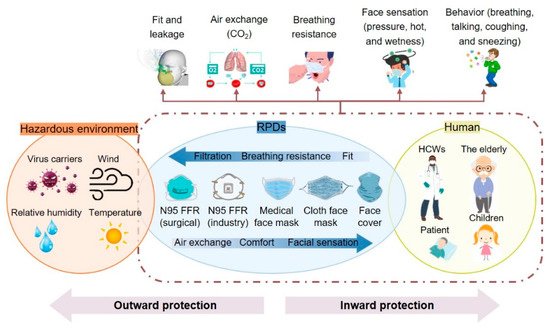
Figure 2. Interacting factors for different hazardous environments, respiratory protective devices (RPDs), and end users and their impact on protective performance and comfort.
3. Decontamination and Reuse of RPDs
Despite increased production, the shortage of PPE for healthcare workers and the general public remains an urgent issue in the US [26][27]. The demand for PPE is expected to remain high, with an estimated annual increase of 20% between 2020 and 2025 [28]. The COVID-19 pandemic has worsened the situation with substantially increased demand, leading to further concerns about the environmental impact of discarded RPDs.
Plastic and medical waste is an important environmental issue that has economic, social, and technological aspects [29][30]. Drastically increased demand and usage of medical PPE and supplies have transformed the dynamics of plastic waste generation. A recent study estimated that globally, 129 billion disposable masks and 65 billion disposable gloves are used every month [31][32]. Medical waste is expected to grow by 370% and packaging plastic by 40% in some areas compared to pre-pandemic consumption. (Figure 6) [27][32]. The Chinese city of Wuhan generated nearly 247 tons of medical waste per day at the peak of the COVID-19 pandemic, nearly six times more than before the pandemic [33]. Mixed plastics, like those in single-use masks and other medical supply materials, also pose a great threat to the environment due to their low recyclability [29].
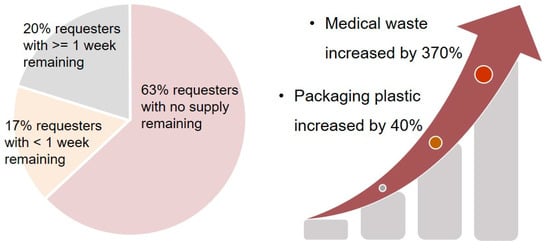
Figure 6. Respirator shortage and medical waste increase as a consequence of COVID-19.
Unsafe disposal of healthcare waste is not only a threat to the environment but also a potential source of disease spread, including hepatitis, HIV/AIDS, and SARS [34][35]. Reuse of disposable medical equipment may also cause respiratory disease [35]. Therefore, adopting advanced waste management, transitioning toward environmentally friendly materials such as bioplastics, and utilizing new sustainable technologies are crucial to fighting future pandemics. Presently, developing a generalizable approach to RPD decontamination and reuse appears promising to mitigate environmental issues in the long term.
References
- Racz, L.; Yamamoto, D.P.; Eninger, R.M. Handbook of Respiratory Protection: Safeguarding against Current and Emerging Hazards; CRC Press: Boca Raton, FL, USA, 2017.
- CDC. 42 CFR Part 84 Respiratory Protective Devices. 1997. Available online: https://www.cdc.gov/niosh/npptl/topics/respirators/pt84abs2.html (accessed on 10 October 2021).
- FDA. Face Masks, Including Surgical Masks, and Respirators for COVID-19. 2020. Available online: https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/face-masks-including-surgical-masks-and-respirators-covid-19 (accessed on 12 October 2021).
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Sciences Policy; Committee on the Use of Elastomeric Respirators in Health Care. Reusable Elastomeric Respirators in Health Care: Considerations for Routine and Surge Use; Liverman, C.T., Yost, O.C., Rogers, B.M.E., Clever, L.H., Eds.; National Academies Press (US): Washington, DC, USA, 2018.
- National Academies of Sciences, Engineering, and Medicine. Current Issues in the Assessment of Respiratory Protective Devices for Occupational and Non-Occupational Uses: Proceedings of a Workshop; The National Academies Press: Washington, DC, USA, 2021.
- Karim, N.; Afroj, S.; Lloyd, K.; Oaten, L.C.; Andreeva, D.V.; Carr, C.; Farmery, A.D.; Kim, I.-D.; Novoselov, K.S. Sustainable personal protective clothing for healthcare applications: A review. ACS Nano 2020, 14, 12313–12340.
- Chua, M.H.; Cheng, W.; Goh, S.S.; Kong, J.; Li, B.; Lim, J.Y.C.; Mao, L.; Wang, S.; Xue, K.; Yang, L.; et al. Face masks in the new COVID-19 normal: Materials, testing, and perspectives. Research 2020, 2020, 7286735.
- Blachere, F.M.; Lemons, A.R.; Coyle, J.P.; Derk, R.C.; Lindsley, W.G.; Beezhold, D.H.; Woodfork, K.; Duling, M.G.; Boutin, B.; Boots, T. Face mask fit modifications that improve source control performance. medRxiv 2021.
- Patel, R.B.; Skaria, S.D.; Mansour, M.M.; Smaldone, G.C. Respiratory source control using a surgical mask: An in vitro study. J. Occup. Environ. Hyg. 2016, 13, 569–576.
- O’Dowd, K.; Nair, K.M.; Forouzandeh, P.; Mathew, S.; Grant, J.; Moran, R.; Bartlett, J.; Bird, J.; Pillai, S.C. Face masks and respirators in the fight against the COVID-19 pandemic: A review of current materials, advances and future perspectives. Materials 2020, 13, 3363.
- AATCC. AATCC M14-2020 Guidance and Considerations for General Purpose Textile Face Coverings: Adult; AATCC: Research Triangle, NC, USA, 2020.
- ASTM. ASTM F3502-21 Standard Specification for Barrier Face Coverings; ASTM International: West Conshohocken, PA, USA, 2021.
- Furukawa, N.W.; Brooks, J.T.; Sobel, J. Evidence supporting transmission of severe acute respiratory syndrome coronavirus 2 while presymptomatic or asymptomatic. Emerg. Infect. Dis. 2020, 26, e201595.
- Gómez-Ochoa, S.A.; Franco, O.H.; Rojas, L.Z.; Raguindin, P.F.; Roa-Díaz, Z.M.; Wyssmann, B.M.; Guevara, S.L.R.; Echeverría, L.E.; Glisic, M.; Muka, T. COVID-19 in health-care workers: A living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am. J. Epidemiol. 2021, 190, 161–175.
- He, D.; Zhao, S.; Lin, Q.; Zhuang, Z.; Cao, P.; Wang, M.H.; Yang, L. The relative transmissibility of asymptomatic COVID-19 infections among close contacts. Int. J. Infect. Dis. 2020, 94, 145–147.
- Gandhi, M.; Yokoe, D.S.; Havlir, D.V. Asymptomatic Transmission, the Achilles’ Heel of Current Strategies to Control COVID-19. In The COVID-19 Reader; Routledge: London, UK, 2020; pp. 36–39.
- Gao, Z.; Xu, Y.; Sun, C.; Wang, X.; Guo, Y.; Qiu, S.; Ma, K. A systematic review of asymptomatic infections with COVID-19. J. Microbiol. Immunol. Infect. 2021, 54, 12–16.
- Feng, Y.; Marchal, T.; Sperry, T.; Yi, H. Influence of wind and relative humidity on the social distancing effectiveness to prevent COVID-19 airborne transmission: A numerical study. J. Aerosol Sci. 2020, 147, 105585.
- Dbouk, T.; Drikakis, D. On respiratory droplets and face masks. Phys. Fluids 2020, 32, 063303.
- Setti, L.; Passarini, F.; De Gennaro, G.; Barbieri, P.; Perrone, M.G.; Borelli, M.; Palmisani, J.; Di Gilio, A.; Piscitelli, P.; Miani, A. Airborne transmission route of COVID-19: Why 2 meters/6 feet of inter-personal distance could not be enough. Int. J. Environ. Res. Public Health 2020, 17, 2932.
- WHO. Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions. 2020. Available online: https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions (accessed on 15 October 2021).
- CDC. CDC Calls on Americans to Wear Masks to Prevent COVID-19 Spread. 2020. Available online: https://www.cdc.gov/media/releases/2020/p0714-americans-to-wear-masks.html (accessed on 2 October 2021).
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.-M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.-H.; et al. An evidence review of face masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118.
- Liang, M.; Gao, L.; Cheng, C.; Zhou, Q.; Uy, J.P.; Heiner, K.; Sun, C. Efficacy of face mask in preventing respiratory virus transmission: A systematic review and meta-analysis. Travel Med. Infect. Dis. 2020, 36, 101751.
- Cheng, Y.; Ma, N.; Witt, C.; Rapp, S.; Wild, P.S.; Andreae, M.O.; Pöschl, U.; Su, H. Face masks effectively limit the probability of SARS-CoV-2 transmission. Science 2021, eabg6296.
- O’Reilly, K.B. Amid PPE Shortage, AMA Collaboration Offers Supplier for Doctors. 2020. Available online: https://www.ama-assn.org/delivering-care/public-health/amid-ppe-shortage-ama-collaboration-offers-supplier-doctors (accessed on 10 October 2021).
- GUP. PPE Data on the Personal Protective Equipment Shortage across the U.S. 2021. Available online: https://getusppe.org/data/ (accessed on 19 November 2021).
- Dean, R. PPE: Polluting Planet Earth. Br. Dent. J. 2020, 229, 267.
- Vanapalli, K.R.; Sharma, H.B.; Ranjan, V.P.; Samal, B.; Bhattacharya, J.; Dubey, B.K.; Goel, S. Challenges and strategies for effective plastic waste management during and post COVID-19 pandemic. Sci. Total Environ. 2021, 750, 141514.
- Gorrasi, G.; Sorrentino, A.; Lichtfouse, E. Back to plastic pollution in COVID times. Environ. Chem. Lett. 2021, 19, 1–4.
- Prata, J.C.; Silva, A.L.; Walker, T.R.; Duarte, A.C.; Rocha-Santos, T. COVID-19 pandemic repercussions on the use and management of plastics. Environ. Sci. Technol. 2020, 54, 7760–7765.
- Silva, A.L.P.; Prata, J.C.; Walker, T.R.; Duarte, A.C.; Ouyang, W.; Barcelò, D.; Rocha-Santos, T. Increased plastic pollution due to COVID-19 pandemic: Challenges and recommendations. Chem. Eng. J. 2020, 405, 126683.
- Singh, N.; Tang, Y.; Zhang, Z.; Zheng, C. COVID-19 waste management: Effective and successful measures in Wuhan, China. Resour. Conserv. Recycl. 2020, 163, 105071.
- Harhay, M.O.; Halpern, S.D.; Harhay, J.S.; Olliaro, P.L. Health care waste management: A neglected and growing public health problem worldwide. Trop. Med. Int. Health 2009, 14, 1414–1417.
- WHO. Health-Care Waste. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/health-care-waste (accessed on 10 October 2021).
More
