Vaccine hesitancy is a prevalent and ongoing issue. However, due to the COVID-19 pandemic, additional attention has been brought to the topic of vaccine hesitancy. Vaccine hesitancy is a threat to the population’s health globally.
- vaccine uptake
- vaccine hesitancy
- COVID-19 vaccination
- conceptual model
1. Introduction
Vaccine hesitancy is defined as “the reluctance or refusal to vaccinate despite the availability of vaccines [1]”. The reasons for vaccine hesitancy vary and are multifaceted, ranging from behavioral, social, and political factors.
If and when the main causal factor to low vaccine uptake is access and availability, domestic and international partners must focus on supply chain issues. However, if the issue is hesitancy regardless of access, one must examine the demand-related factors contributing to low vaccine uptake. The global situation around the COVID-19 vaccine provides a perfect example. In the US, vaccine hesitancy is driven by a lack of demand linked to personal beliefs, stereotypes, and socio-cultural factors [2]. Yet, in much of the Global South, low vaccination rates are fueled by the lack of access to adequate doses of the vaccine to protect entire populations. For example, when COVID-19 vaccines were in development, high-income countries began making deals with pharmaceutical companies for pre-order [3]. Over 80% of the COVID-19 vaccine developed by Pfizer was claimed by the United States, United Kingdom, European Union, and Japan. Even if the vaccine was made available to countries in the Global South (such as Latin America, India, Southeast Asia, and South Africa), there are still costs associated with maintenance, storage, transportation, and distribution [3][4].
1.1. Childhood Vaccine Hesitancy
1.2. COVID-19 Vaccine Hesitancy
Currently, the focus of vaccinations has shifted towards COVID-19 vaccination efforts. As of November 2021, the COVID-19 pandemic has seen 248 million cases with over 5 million deaths [10]. In December 2020, based on concerted global efforts, scientists successfully developed vaccines to help control the spread of COVID-19. Unfortunately, vaccine hesitancy has proven to be a major hindrance to COVID-19 vaccination uptake. A recent systematic review of COVID-19 related to vaccine hesitancy globally found wide variation in vaccine hesitancy between countries, with the overall acceptance rate below 70% [11]. This systematic review also included results from eight separate studies with health care providers and reported vaccine acceptance rates among health care workers ranging from 28% in the Democratic Republic of the Congo to 78% in Israel. The review concludes that addressing the scope of COVID-19 vaccine hesitancy in various countries requires building trust in the vaccination efforts.2. Conceptual Model for Addressing Vaccine Hesitancy
The creation of theour conceptual model below is based on a review of 15 articles specifically relating to vaccine uptake and hesitancy. TheOur final model combines three existing vaccination models: WHO Increasing Vaccination Model (Figure 1), the SAGE Vaccine Hesitancy Determinants Matrix (Figure 2), and the Journey to Immunization–UNICEF (Figure 3). Each of these models has its strengths and weaknesses. The core strength of each of these models is that they illustrate causal factors associated with vaccine hesitancy.
2.1. WHO Increasing Vaccination Model
The 2017 Increasing Vaccination Model showcases the factors that increase vaccination uptake among individuals [12]. This model is set in a context where governments fund some of the cost of vaccinations, or private insurance covers the cost. These factors result from a variety of behaviors by a multitude of different factors [13]. The three main propositions in the model are that vaccination uptake results from what people think and feel and the social processes that lead to motivation and ultimately vaccination uptake (Figure 1).
The first proposition in this model is that an individual’s thoughts and feelings motivate vaccine uptake [13]. This includes perceived risk, hesitancy, confidence, and trust. Social processes come next, motivating the uptake of vaccines and consist of a recommendation from health providers, social and gender norms, information sharing, and rumors. Motivation, as shown in the middle, plays a vital role in predicting vaccine uptake. The practical issues box underscores the barriers to vaccination, but these issues are measurable and can be addressed through vaccination programs. In isolation, these factors might not always have a meaningful impact on vaccine uptake (i.e., individual thoughts and feelings) [13]. Still, their interactions, including the role of practical issues, make this a promising model. Overall, the Increasing Vaccination Model showcases the interrelated factors, resources, and behaviors that affect vaccination uptake.
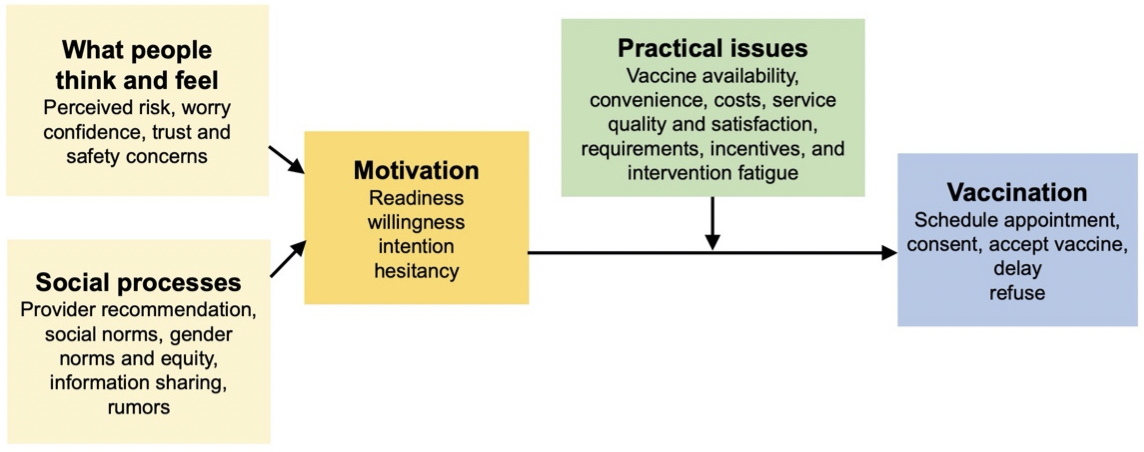
Figure 1.
The Increasing Vaccination Model (2017)
[13]
.
While very practical, the Increasing Vaccination Model is relatively simple and includes one-way relationships between individual and social processes that can increase vaccination coverage. These one-way relationships fail to consider other interactions that could take place. This model places vaccine hesitancy as part of the “motivation factors” followed by structural issues such as availability and affordability. However, vaccine hesitancy is a complex process that exists despite the availability of vaccines [5][13]. This distinction is important from an intervention perspective. In the model’s current state, it appears that if a provider recommends a vaccine, that will influence motivation, but motivational factors would not impact how a recommendation is perceived. It has been previously demonstrated that an individual who is motivated towards something is selective in how they perceive external factors [14]. In addition, this model does not indicate a relationship between individual thoughts and feelings and social processes. Lastly, as the creators of this model acknowledge, more research is needed to determine the role of social processes on vaccine uptake [13].
While providing ample information on the barriers to vaccination uptake at each level of the socio-ecological model (SEM), the Increasing Vaccination Model falls short of explicating the specific causal linkages between the barriers that cut across the different levels of SEM.
2.2. The Vaccine Hesitancy Determinants Model
The Vaccine Hesitancy Determinants Model, created in 2012, was adapted from the results of a discussion held with approximately 40 experts from relevant fields during the “Workshop on the Cultural and Religious Roots of Vaccine Hesitancy: Explanations and implications for the Canadian Healthcare” [7] (Figure 2). This model was based on the 3Cs, which postulates that vaccine hesitancy exists at the intersection of three factors: confidence, complexity, and complacency. The detailed matrix showcases the variety of factors that influence individual behavior regarding vaccine hesitancy [15]. The Vaccine Hesitancy Determinants Model consists of three interrelated areas addressing vaccine hesitancy, including the role of the individual decision-making process, the role of public health, and the role of health professionals. Individual reflection and their decision-making process are influenced by communication and media, religious and cultural characteristics, attitudes, risk perception and evaluation, knowledge, and beliefs. The role of public health influences vaccination programs and coverage. Public health also plays a large role in communicating with the population in an acceptable manner. The role of health professionals is influenced by knowledge, beliefs, and training, and influences counseling and vaccine delivery services [16]. Overall, the model stresses that individual decision-making regarding vaccination is multifaceted and involves emotional, cultural, social, religious, and political factors just as much as it involves cognitive factors.

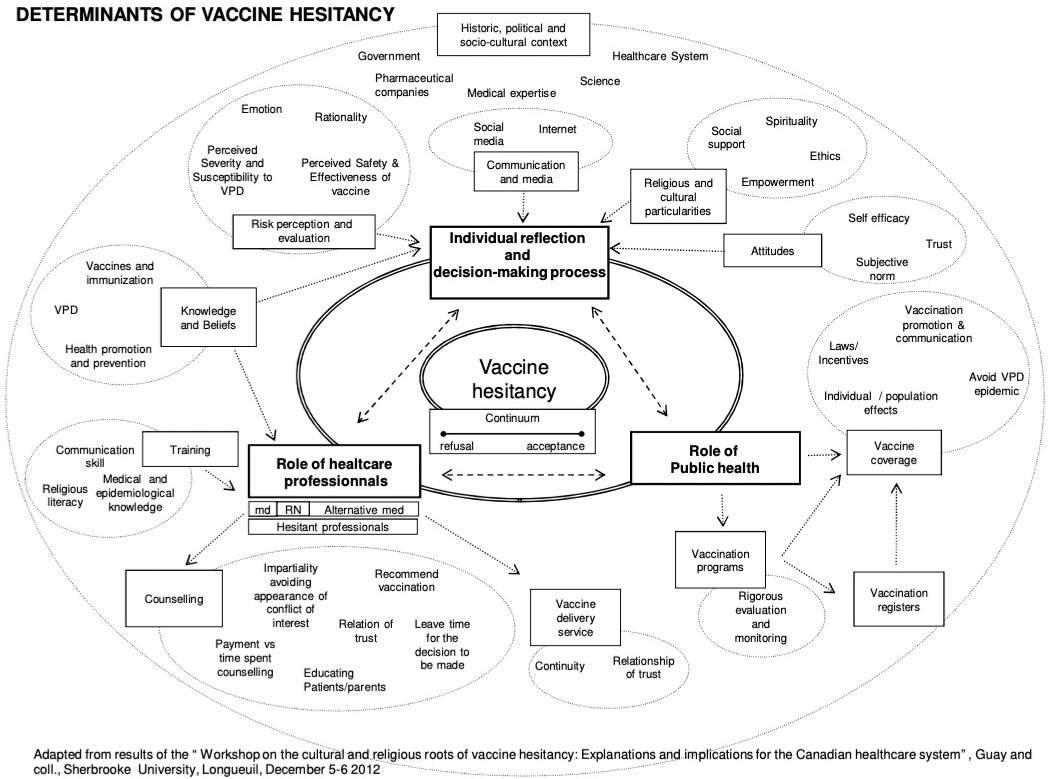
Figure 2.
The Vaccine Hesitancy Determinants Model (2011)
[7]
.
The Vaccine Hesitancy Determinants Model is a comprehensive approach to understanding multiple causal factors influencing vaccine hesitancy. It has been used widely in research to examine vaccine hesitancy in specific contexts as well as a global phenomenon. While this model has the potential for standardization of the determinants of vaccine hesitancy, there is still a lack of clarity in some of the constructs. For example, previous research has highlighted the challenges of determining vaccine hesitancy at the population level [17]. Additionally, it may be much too complex to understand and apply holistically to intervention research.
2.3. The Journey to Immunization–UNICEF
The third model, the Journey to Immunization, created in 2017, follows a caregiver or vaccine recipient’s journey to immunization [18]. This model may also be used to follow the journey of a health care provider since the end goal is immunization (Figure 3). This model spans from the knowledge and awareness of vaccines to what happens after vaccination and allows interventions to focus on the area that needs the most attention. The elements of this model are situated within a socio-ecological framework and include individual, family, community, health care, and political systems. The model applies a steps approach by highlighting six core factors within a vaccination journey. These include knowledge and awareness, intent, preparation, cost and effort, point of service, and after service. Knowledge and awareness address the actual vaccine, disease, and service (such as when, where, and how to get the vaccine). Intent is overcoming the gap between intent to vaccinate and getting vaccinated. Willingness to vaccinate is contributed to attitudes towards the behavior, subjective norms, and perceived behavioral control. Preparation considers the disease, vaccination, and service and determines the logistics of acquiring the vaccination (for example, transportation, cost, and childcare). Cost and effort relate to opportunity, transportation, lost income, uncertainty of service, and social and security costs. Point of service involves all aspects of the vaccination experience (such as client satisfaction and interpersonal communication with health providers). Finally, after service includes some factors such as feedback, next steps, side effects, and reminders.
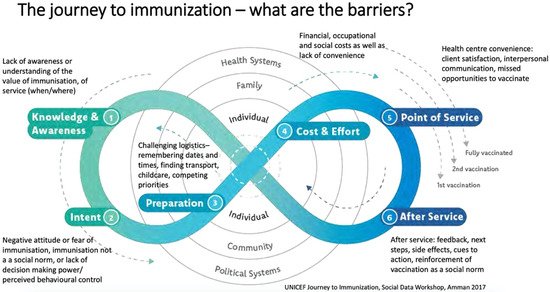
The Journey to Immunization Model is useful to understand barriers and provides a process-oriented framework for designing future interventions. Still, its cyclical nature makes it difficult to utilize as an evaluation framework.
2.4. Front Line Health Workers and Interpersonal Communication and Counselling
UNICEF has found that a key determinant leading to vaccine hesitancy is linked to the quality of communication between health workers and clients. Health workers can be perceived as either trusted sources of information or having insufficient knowledge [19]. Therefore, the final opportunity to be influenced lies in the skills of the FLW. Even though most caregivers support immunizations and immunize their children before entering school, questions and concerns are still customary. Questions and concerns regarding childhood vaccinations and COVID-19 vaccinations can relate to side effects, ingredients, and number of doses [20]. According to WHO, FLWs are seen as influencers and trusted sources of information on vaccines [5]. Therefore, FLWs must be trained and supported to provide accurate information and support to patients. Strengthening health workers’ interpersonal communication and counseling (IPC/C) capacities is one effort to deliver messages and promote vaccine uptake effectively. Interpersonal communication (IPC) specifically focuses on informing and educating caregivers, soon-to-be-caregivers, and vaccine recipients about vaccination. A recommendation from a health provider can move a caregiver or vaccine recipient from hesitant to accepting a vaccine [7][13][15][19][21][22]. Recommendations from a frontline worker may increase confidence, set a social norm, or showcase a direct behavior change method.
After studying these models and conducting an extensive literature review, the conceptual model below reflects important constructs to consider when addressing vaccine hesitancy (Figure 4). The overarching goal for this model is “To improve demand for and equitable delivery of immunization services with a focus on increased access to and demand for immunization services.” The impact of reducing vaccine hesitancy is measurable through improved vaccination uptake and subsequent declines in the incidence of vaccine-preventable diseases. This is the long-term view of the process. Several proximal factors contribute to the reduction in vaccine hesitancy. Background factors include age, gender, socioeconomic status, and geographic location, to name a few.
Furthermore, other factors can be classified into upstream factors and downstream factors. Upstream factors include facilities, supplies, policies and laws, and communication and media environment. Challenging upstream factors falls within the realm of governments, international organizations, non-governmental organizations (NGOs), and national and local governments. Successful vaccination uptake requires addressing upstream factors that are linked with vaccine uptake but not directly connected with the constructs in theour model. The purpose of this model is not to provide a holistic picture but to measure specific intermediate outcomes (indicators), which can then be directly linked to the intention to vaccinate.
The impact of vaccination programs can truly be verified by studying trends in vaccine uptake. This data takes time to collect, is collected at an aggregate level, and does not provide a nuanced look at the ground level. Therefore, one specific key measurable outcome for intervention evaluations can be identified as “intention to vaccinate” and/or “vaccination reported by vaccine recipients”.

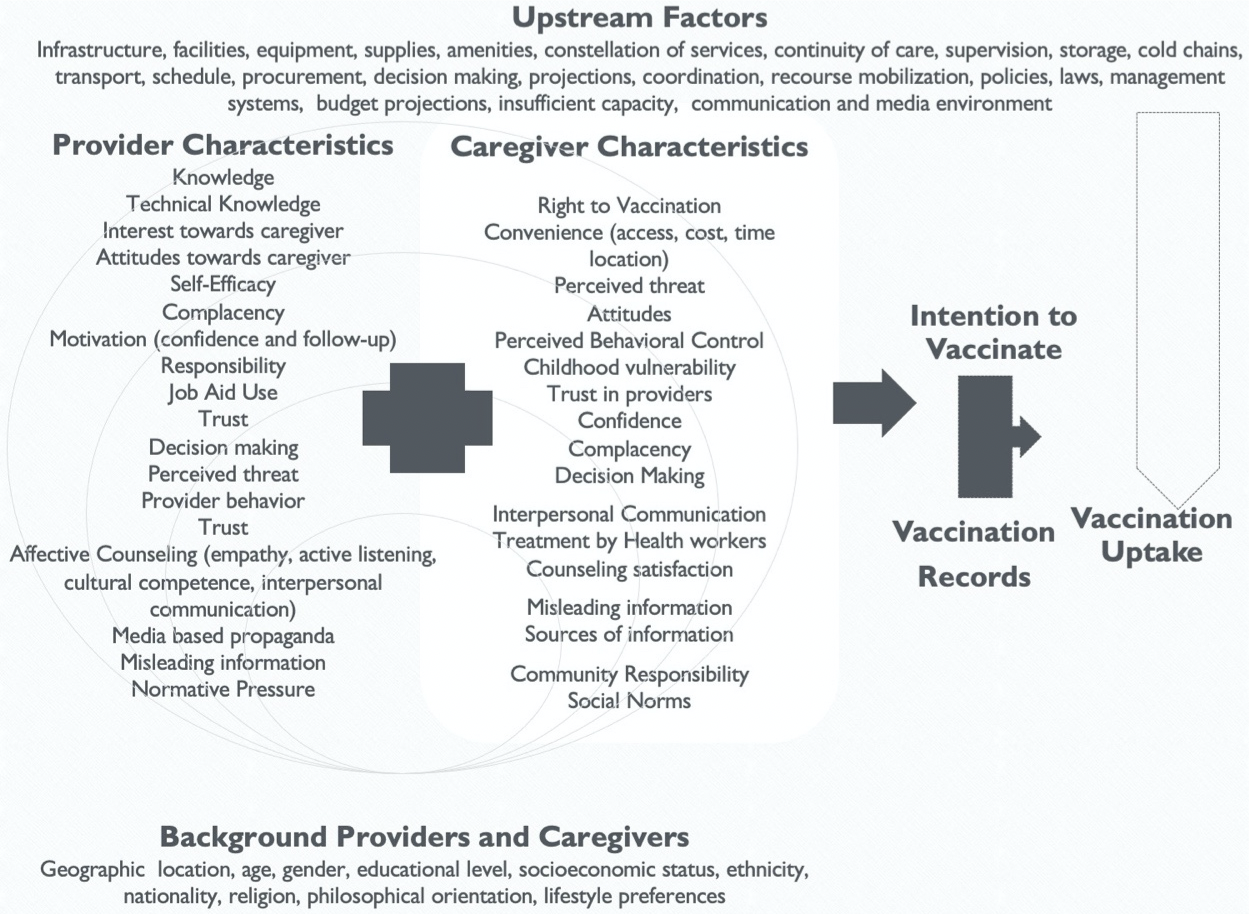
Figure 4.
Providers and Caregivers Conceptual Model.
This model specifically focuses on provider and caregiver/vaccine recipient factors that influence the intention to vaccinate. This outcome is achievable through a series of related steps. Although most constructs are standalone, some constructs for providers are multidimensional and cannot be directly measured. In these cases, broader topics were identified and subdomains created. For example, the broader topic of affective counseling by providers is measured through empathy, active listening, cultural competence, and interpersonal communication. Combining these questions can help create an affective counseling scale measure, which can then be correlated with other constructs. Additionally, motivation is a function of confidence, follow-up, and interest towards the caregiver.
The constructs under the caregivers’ box in the conceptual model showcase the levels of the SEM. Individual-level constructs include attitudes, perceived threat, social norms, perceived behavioral control, decision-making, complacency, confidence, counseling satisfaction, and interpersonal communication; community-level constructs include trust in providers, caregiver vulnerability, sources of information, misleading information, and community responsibility; finally, at the societal level is convenience and the right to vaccination. This conceptual model is intended to be adaptable to local contexts, and sub-measures that are not relevant to specific contexts can be deleted.
3. Findings
Vaccine hesitancy is a global issue. Any model seeking to explain causal factors and their relationships must first define the indicators intended to be measured to avoid any misunderstanding. Overall, it is presumed that addressing the various indicators that impact caregiver behavior will help caregivers decide (intention) to vaccinate their child(ren) or take the vaccine, in the case of vaccine recipients. Positive improvements over time in the intermediate outputs/factors, combined with intent to act on the demand side and improvements in the supply side and upstream factors, will increase vaccination uptake (the impact indicator).
Instead of only deciding whether to vaccinate their child, individuals also decide for themselves. The reasons for vaccine hesitancy vary in each community or country, and now the public health community is tasked with promoting vaccine uptake among eligible adults, caregivers, and their children aged five years and older [23]. Currently, only 56.5% of the global population is partially vaccinated against COVID-19 [24]. The fewer vaccinated people, the more risk exists to spread disease. Therefore, addressing COVID-19 vaccine hesitancy for those five years old and above is crucial to mitigate the number of coronavirus cases and protect the population’s health.
Previous research has showcased the correlation between sociodemographic factors and vaccine hesitancy [2][25]. Specifically, this includes correlations between vaccine hesitancy and education, income, gender, race, and/or marital status [26][27][28][29][30]. However, some of these factors, including gender, are not consistently correlated with vaccine hesitancy and may be context- or vaccine-specific [26]. To address vaccine hesitancy, there needs to be an understanding of the psychological and social dimensions, with appropriate measures to monitor the shift in behavior accompanied by reliable and valid outcome measures [27][28][29]. The ability to understand these dimensions and contextual adaptation is especially important for COVID-19 vaccine hesitancy.
References
- World Health Organization. Top Ten Threats to Global Health in 2019. 2019. Available online: https://www.who.int/news-room/feature-stories/ten-threats-to-global-health-in-2019. (accessed on 10 November 2021).
- Shapiro, G.K.; Tatar, O.; Dube, E.; Amsel, R.; Knauper, B.; Naz, A.; Perez, S.; Rosberger, Z. The vaccine hesitancy scale: Psychometric properties and validation. Vaccine 2018, 36, 660–667.
- Amaya, A.B.; de Lombaerde, P. Regional cooperation is essential to combatting health emergencies in the Global South. Glob. Health 2021, 17, 9.
- Walker, P.G.; Whittaker, C.; Watson, O.J.; Baguelin, M.; Winskill, P.; Hamlet, A.; Djaafara, B.A.; Cucunubá, Z.; Mesa, D.O.; Green, W.; et al. The impact of COVID-19 and strategies for mitigation and suppression in low-and middle-income countries. Science 2020, 369, 413–422.
- World Health Organization. Vaccines: The Powerful Innovations Bringing WHO’s Mission to Life Every Day. 2018. Available online: https://www.who.int/news-room/commentaries/detail/vaccines-the-powerful-innovations-bringing-who-s-mission-to-life-every-day. (accessed on 8 November 2021).
- Edwards, K.M.; Hackell, J.M.; Byington, C.L.; Maldonado, Y.A.; Barnett, E.D.; Davies, H.; Lynfield, R.; Munoz, F.M.; Nolt, D.; Nyquist, A.C.; et al. Countering Vaccine Hesitancy. Pediatrics 2016, 138, e3.
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J.A. Vaccine hesitancy: An overview. Hum. Vaccines Immunother. 2013, 9, 1763–1773.
- Marshall, G.S. Vaccine Hesitancy, History, and Human Nature: The 2018 Stanley A. Plotkin Lecture. J. Pediatric Infect. Dis. Soc. 2018, 8, 1–8.
- UNICEF. Immunization Coverage. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage. (accessed on 10 November 2021).
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard 2021. Available online: https://covid19.who.int. (accessed on 11 November 2021).
- Sallam, M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines 2021, 9, 160.
- Noel T. Brewer; Gretchen B. Chapman; Alexander J. Rothman; Julie Leask; Allison Kempe; Increasing Vaccination: Putting Psychological Science Into Action. Psychological Science in the Public Interest 2017, 18, 149-207, 10.1177/1529100618760521.
- Noel T. Brewer; What Works to Increase Vaccination Uptake. Academic Pediatrics 2021, 21, S9-S16, 10.1016/j.acap.2021.01.017.
- Irwin M. Rosenstock; Why People Use Health Services. Milbank Quarterly 2005, 83, N/A, 10.1111/j.1468-0009.2005.00425.x.
- NONI E. MacDonald; Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161-4164, 10.1016/j.vaccine.2015.04.036.
- Report of the SAGE Working Group on Vaccine Hesitancy . World Health Organization. Retrieved 2022-1-21
- Determinants of vaccine hesitancy in Africa: a systematic review . OpenUCT. Retrieved 2022-1-21
- A Human-Centred Field Guide for Investigating and Responding to Challenges . UNICEF. Retrieved 2022-1-21
- Interpersonal Communication for Immunization Training for Front Line Workers . UNICEF. Retrieved 2022-1-21
- Allison Fisher; Sarah Mbaeyi; Amanda Cohn; Addressing Vaccine Hesitancy in the Age of COVID-19. Academic Pediatrics 2021, 21, S3-S4, 10.1016/j.acap.2021.03.013.
- Douglas J. Opel; John Heritage; James A. Taylor; Rita Mangione-Smith; Halle Showalter Salas; Victoria DeVere; Chuan Zhou; Jeffrey D. Robinson; The Architecture of Provider-Parent Vaccine Discussions at Health Supervision Visits. Pediatrics 2013, 132, 1037-1046, 10.1542/peds.2013-2037.
- Johanna E.R. Rutten; Ramona Backhaus; Jan Ph Hamers; Hilde Verbeek; Working in a Dutch nursing home during the COVID‐19 pandemic: Experiences and lessons learned. Nursing Open 2021, N/A, N/A, 10.1002/nop2.970.
- Interim Statement on COVID-19 Vaccination for Children and Adolescents . World Health Organization. Retrieved 2022-1-21
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 2021, 5, 947–953.
- Quinn, S.C.; Jamison, A.; An, J.; Freimuth, V.S.; Hancock, G.R.; Musa, D. Breaking down the monolith: Understanding flu vaccine uptake among African Americans. SSM-Popul. Health 2018, 4, 25–36.
- Rosenstock, I.M. Why People Use Health Services. Milbank Q. 2005, 83.
- Domek, G.J.; O’Leary, S.T.; Bull, S.; Bronsert, M.; Contreras-Roldan, I.L.; Ventura, G.A.B.; Kempe, A.; Asturias, E.J. Measuring vaccine hesitancy: Field testing the WHO SAGE Working Group on Vaccine Hesitancy survey tool in Guatemala. Vaccine 2018, 36, 5273–5281.
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Zhou, Y.; Dube, E.; Schuster, M.; MacDonald, N.E.; Wilson, R.; The SAGE Working Group on Vaccine Hesitancy. Measuring vaccine hesitancy: The development of a survey tool. Vaccine 2015, 33, 4165–4175.
- Leask, J.; Willaby, H.W.; Kaufman, J. The big picture in addressing vaccine hesitancy. Hum. Vaccines Immunother. 2014, 10, 2600–2602.
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779.
 Encyclopedia
Encyclopedia
