Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Stefan Cristian Vesa and Version 2 by Catherine Yang.
Cardiovascular disease prevention in the general population, and especially in older adults, starts from lifestyle modification. To prevent cardiovascular disease not just in elderly patients, but in all age groups, it is recommended to avoid a sedentary lifestyle and to exercise within the limits of individual tolerance. It is common knowledge that physical exercise has a positive impact on improving health and quality of life. In the elderly, regular exercise can exert an important contribution in reducing falls, maintaining good physical function and maintaining a good quality of life.
- cardiovascular disease
- elderly
- prevention
1. Mechanisms and Effects
There are multiple studies that aimed to establish the mechanisms by which physical activity has a positive impact on health status of the elderly, the benefits being already reviewed since the early 2000s [1][104]. Besides improving of the physiologic cardiovascular parameters, physical exercise improves cardiovascular symptoms (especially related to heart failure) and blood pressure, and it decreases the risk of coronary artery disease, together with improving the lipid profile and insulin sensitivity [2][1][3][103,104,105]. In addition, physical exercise helps to reduce sympathetic activity, achieving better blood pressure and heart-rate control [3][4][5][105,106,107].
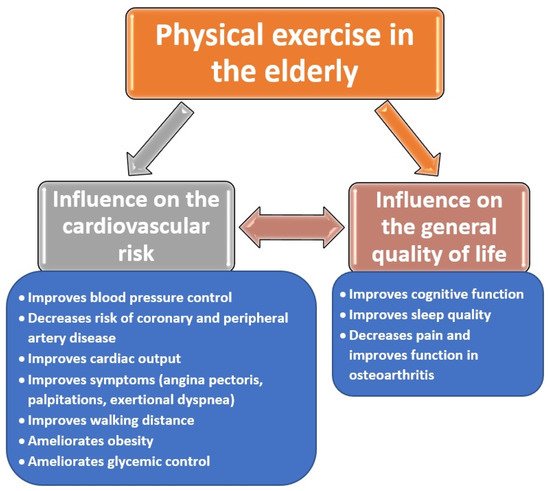
The cardiovascular benefits gained by the elderly due to regular physical exercise are also linked with an increased general quality of life, because it is proven at present that wellbeing and cognitive functioning are also improved in the elderly who exercise regularly [6][108].
The effects of physical exercise on cardiovascular risk factors and the quality of life of the elderly are highlighted in the following figure (Figure 12).
2. Types of Physical Activities Studied in the Elderly
The key principles of the recommended physical activity in older adults are the following: the preferred exercises are aerobic ones, which need to be supplemented by balance, strengthening and flexibility exercises [7][109]. Both the British National Health Service NHS and the American Center for Disease Control and Prevention CDC recommend that adults above the age of 65 should perform at least 150 min of moderate intensity physical activity each week (the best example being brisk walking at 30 min per day, 5 days a week) [8][9][110,111]. If the elderly are already active persons, the physical activity can be limited to 75 min of vigorous intensity activity per week (such as jogging and running). At least 2 days a week, the subjects must add to the previous examples some muscle-strengthening activities that work all major muscle groups (hips, legs, back, abdomen, shoulders, chest and arms) [8][9][110,111]. In a recently published nationwide cohort study on older adults, physical activity was inversely associated with long-term mortality risk, confirming that the maximum benefits in terms of survival were achieved at around 150 min of exercise per week [10][112].
Many studies emphasize that there should not exist an ideal exercise to be prescribed in a certain profile of the older adult, because it was shown that even modest levels of physical activity offer benefits in terms of cardiovascular risk, compared to being completely inactive [11][113]. To date, the most commonly recommended exercise is walking, and gait speed is proposed as a powerful marker of longevity in elderly and frail subjects [12][114]. Walking counts as a moderate-intensity activity, as are water aerobics, hiking (flat terrain), dancing, riding a bike or pushing a lawn mower [8][110]. Vigorous activities can include any of the following: running or swimming (non-professional level), aerobics, tennis, football or hiking uphill [8][110]. For muscle strengthening, it is recommended to work with resistance bands (such as Thera-Band® elastic bands), lifting weights (even carrying shopping bags) or yoga and Pilates exercises [8][13][110,115]. Older women are more predisposed to practice less physical exercise than men. In a recently published study, it was shown that general exercises and dancing improve balancing skills, and might reduce the risk of falls in elderly women [14][116].
Unfortunately, during the COVID-19 pandemic, older adults have suffered a further reduction of physical exercise, due to social distancing. At present, there is low to moderate evidence that mobile or internet-delivered (eHealth) interventions may be efficient in promoting and increasing the levels of physical activity in the elderly [15][117].
3. Physical Activity, Insulin Sensitivity and Glycemic Control
Regardless of the exercise performed, whether it is running or walking, many studies have reported that during the active contraction of striated muscles, there is an increase in the translocation of type 4 glucose transporter (GLUT4) from the cytoplasm of striated muscle cells, the result being the promotion of blood glucose absorption, thus improving insulin resistance; this mechanism is known to play a major role in the development of T2DM [16][17][118,119]. After glucose enters the cells, it will be transformed into glucose-6-phosphate (G-6-P) through the process of phosphorylation under the action of hexokinase. G-6-P is directly involved in the processes of glycolysis and glycogenesis, processes that increase the level of blood glucose absorption. A study performed on diabetic rats illustrated how physical activity leads to an increase in G-6-P levels in striated muscle cells but also to improved activity of GLUT4, hexokinase and glycogen-synthetase activity, thereby improving glucose tolerance and lowering blood glucose levels. Reduction of blood glucose levels is synonymous with an optimal control of diabetes, hence the risk of cardiovascular disease secondary to poorly controlled diabetes an unbalanced diabetes among elderly patients will be significantly lowered [18][120].
4. Physical Activity and Blood Pressure Values
As previously mentioned, high blood pressure predisposes a person to cardiovascular disease, as well as complications such as acute myocardial infarction, heart failure or stroke [19][121]. Following physical activity, a transient decrease in blood pressure was found, both among people diagnosed with hypertension and among normotensive people [20][122].
Studies which determined the beneficial effect of physical activity on blood pressure proved that physical activity maintained over a long period of time leads to a decrease in systolic blood pressure by about 5 mmHg, and a reduction in diastolic blood pressure by about 3.5 mmHg. It is well known that a reduction in systolic blood pressure values by 2–3 mmHg decreases the risk of death secondary to a stroke by about 5%, and secondary to an acute coronary episode by 3–4%. However, the decrease in blood pressure is a transient one, which is why performing physical exercises, such as walking, must be performed daily [21][22][123,124].
Nonetheless, when performing exercises of much higher intensity, and without these being adjusted to age and muscle mass, opposite effects occur, namely increased vasoconstrictor activity, an increase in oxidative stress and an increase in blood pressure. Because of these observations, light physical activity is recommended at present for the elderly, such as walking for 30 min daily [23][125].