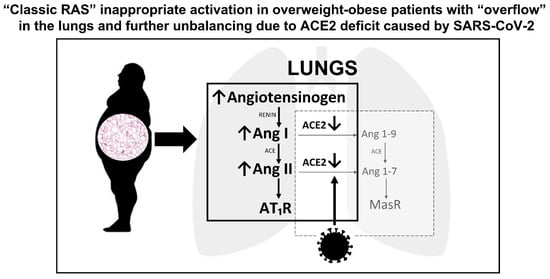
Since the first months of the coronavirus disease 2019 (COVID-19) pandemic, several specific physiologic traits, such as male sex and older age, or health conditions, such as overweight/obesity, arterial hypertension, metabolic syndrome, and type 2 diabetes mellitus, have been found to be highly prevalent and associated with increased risk of adverse outcomes in hospitalized patients. All these cardiovascular morbidities are widespread in the population and often coexist, thus identifying a common patient phenotype, characterized by a hyper-activation of the “classic” renin-angiotensin system (RAS) and mediated by the binding of angiotensin II (Ang II) to the type 1-receptor. At the same time, the RAS imbalance was proved to be crucial in the genesis of lung injury after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, where angiotensin-converting-enzyme-2 (ACE2) is not only the receptor for SARS-CoV-2, but its down-regulation through internalization and shedding, caused by the virus binding, leads to a further dysregulation of RAS by reducing angiotensin 1-7 (Ang 1-7) production.
- COVID-19
- SARS-CoV-2
- cardiovascular disease
- renin-angiotensin system
1. Introduction
2. Disequilibrium between ACE and ACE2 Activity as a Potential Causal Mechanism for Severe COVID-19
3. Overweight, Obesity, Visceral Adiposity and Metabolic Syndrome
4. Type 2 Diabetes Mellitus
New-onset hyperglycemia or acute decompensated diabetes mellitus have been frequently observed in COVID-19 patients [47,48][31][32]. Moreover, susceptibility to other overlapped secondary infections, together with the use of glucocorticoid therapy, can further precipitate acute hyperglycemia [49][33] with increased plasma osmolality, osmotic polyuria and dehydration, endothelial dysfunction, thrombophilia, and amplified pro-inflammatory cytokine secretion, all key factors in SARS-CoV-2-related multi-organ dysfunction. In addition, binding of SARS-CoV-2 to ACE2 in pancreatic cells can damage islets and reduce insulin release, leading to acute hyperglycemia and transient diabetes [50][34]. The evidence that diabetes mellitus causes a pro-inflammatory environment has been corroborated by serum levels of inflammation biomarkers, such as interleukin-6 (IL-6), C-reactive protein (CRP), and ferritin, and D-dimer that are markedly higher in COVID-19 patients with diabetes mellitus compared to controls without diabetes [51][35]. Generally, diabetes mellitus is associated with weakened immune response and enhanced susceptibility to infections, due to inherent neutrophil dysfunction, reduced T-cell responses, and disordered humoral immunity [52][36]. As other cardio-metabolic comorbidities, type 2 diabetes mellitus bears the fingerprint of RAS imbalance: indeed, chronic activation of “classic RAS” is typical in diabetes and insulin-resistance, despite high sodium intake and high blood pressure, and contributes to microvascular and macrovascular complications and is clearly involved in diabetic kidney disease [53][37]. Furthermore, chronic hyperglycemia also reduces the ACE2 expression, with a loss of its anti-inflammatory effects and protection of endothelial function, because of a decreased counter-regulation of Ang II [54,55][38][39].
In the context of ACE/Ang II/AT1R axis hyper-activation, the insulin receptor also uses mitogen-activated protein (MAP) kinase as a downstream mediator of its action [35][23], mediating growth-factor-like effects, such as vascular smooth muscle growth and cardiac hypertrophy [56][40]. Even AT1R can activate MAP kinase in its post-receptor cascade, so it can be postulated that these two receptors synergize to exacerbate and perpetuate inflammation, fibrosis, and tissue injury. These findings are in line with the hypothesis that RAS dysregulation could be the backbone in the pathogenesis of severe COVID-19 in patients with diabetes mellitus. This vulnerability may play a synergistic role with the underpinning inflammatory milieu and immune defects associated with diabetes, providing SARS-CoV-2 a pathway for causing prolonged lung injury.
5. Arterial Hypertension
Worldwide epidemiologic data provided evidence that hypertension is a pivotal comorbidity related to COVID-19 disease severity. In addition to the hypertensive condition, anti-hypertensive therapy is also likely to affect the course of COVID-19. A large meta-analysis enrolling 101,949 COVID-19 patients found a significant association between treatment with RAS inhibitors and mortality reduction among patients with hypertension [62][41].
The mechanisms by which hypertension leads to increased risk of worse outcome in COVID-19 are likely to be many. Hypertension is a major cardiovascular risk factor that promotes arteriosclerosis of large and small arteries and accelerates atherosclerosis, leading to cardiovascular disease and death. Left ventricular hypertrophy and myocardial fibrosis, with increased filling pressures and impaired coronary reserve, are key features that contribute to atrial fibrillation, myocardial ischemia, and heart failure with preserved ejection fraction [76][42]. Certainly, RAS hyper-activation or, at least, “inappropriately normal” renin activity and aldosterone levels are typical of overweight/obese hypertensive patients [33][21]. In these patients, normal or increased Ang II production results in a stimulation of the ACE/Ang II/AT1R pathway, leading to small arteries constriction, hypertrophy, fibrosis, and tissue injury [77][43]. It also leads to the activation of NADPH oxidases, with subsequent generation of reactive oxygen species, protein oxidation, and dysregulated cell signaling [78][44]. Moreover, animal models support a hypothetical link between hypertension and reduced ACE2 expression, corroborated by data showing lower expression of ACE2 mRNA and ACE2 protein expression in the kidneys of hypertensive rats [79][45].
6. Dyslipidemia
Another risk factor often associated with overweight/obesity and MetS is dyslipidemia. Although its influence may vary, according to age and the presence of other comorbidities, meta-analyses found that dyslipidemia was associated with higher mortality and disease severity [85,86][46][47]. Atherogenic dyslipidemia was more frequent in patients with critical COVID-19 and was significantly associated with intubation and death. High triglycerides levels were associated with high levels of inflammatory biomarkers and poor COVID-19 outcome during hospitalization [87][48].7. Male Sex
From the early phases of the pandemic, male sex has been found to be associated to a more severe course of COVID-19 and greater need for intensive care, compared with female sex [102][49]. Studies found how men had a 59% increased risk for severe outcomes compared to women [103][50]. Observational studies reported how the vast majority (82%) of patients that needed intensive care were males [104][51] and how the main determinants of ICU admission were male sex and obesity [105][52]. Several factors can explain this sex difference. Although the greatest evidence on RAS and sex comes from preclinical studies, both types of sex hormones, estrogens and androgens, likely affect the expression and activity of several RAS components, especially regarding the “classic RAS” pathway, while limited data are available on the interactions with the counter-regulatory RAS components [108][53]. Estradiol is likely to cause a protective shift in ACE/ACE2 ratio, by both increasing ACE2 and inhibiting ACE expression [109][54]. Estrogenic activity has been found to inhibit the hemodynamic effects of Ang II and promote the action of ACE2/Ang (1-7) axis in animal models [110][55]. Estrogen has also been found to decrease tissue AT1R expression and aldosterone production, while testosterone conversely increases ACE activity and tissue AT1R expression [108][53]. Furthermore, the gene for ACE2 is located in the X chromosome, which could make it susceptible to escaping X-inactivation in women [111][56]. In an animal model of obesity-associated hypertension, the increase in blood pressure after high-fat diet is attenuated in females compared to males, and this different behavior appears to be mediated by ACE2 activity [112][57]. In humans, men tend to have higher levels of aldosterone than females, regardless of other confounders, facilitated, at least in part, by higher levels of endogenous Ang II [113][58].8. Older Age
References
- Lu, R.; Zhao, X.; Li, J.; Niu, P.; Yang, B.; Wu, H.; Wang, W.; Song, H.; Huang, B.; Zhu, N.; et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 2020, 395, 565–574.
- Barison, A.; Aimo, A.; Castiglione, V.; Arzilli, C.; Lupón, J.; Codina, P.; Santiago-Vacas, E.; Cediel, G.; Emdin, M.; Bayes-Genis, A. Cardiovascular disease and COVID-19: Les liaisons dangereuses. Eur. J. Prev. Cardiol. 2020, 27, 1017–1025.
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069.
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; Cohen, S.L.; et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059.
- Meng, M.; Zhao, Q.; Kumar, R.; Bai, C.; Deng, Y.; Wan, B. Impact of cardiovascular and metabolic diseases on the severity of COVID-19: A systematic review and meta-analysis. Aging 2020, 12, 23409–23421.
- Hernández-Garduño, E. Obesity is the comorbidity more strongly associated for Covid-19 in Mexico. A case-control study. Obes. Res. Clin. Pract. 2020, 14, 375–379.
- Wiener, R.S.; Cao, Y.X.; Hinds, A.; Ramirez, M.I.; Williams, M.C. Angiotensin converting enzyme 2 is primarily epithelial and is developmentally regulated in the mouse lung. J. Cell. Biochem. 2007, 101, 1278–1291.
- Santos, R.A.S.; Oudit, G.Y.; Verano-Braga, T.; Canta, G.; Steckelings, U.M.; Bader, M. The renin-angiotensin system: Going beyond the classical paradigms. Am. J. Physiol. Heart Circ. Physiol. 2019, 316, H958–H970.
- Voors, A.A.; Pinto, Y.M.; Buikema, H.; Urata, H.; Oosterga, M.; Rooks, G.; Grandjean, J.G.; Ganten, D.; van Gilst, W. Dual pathway for angiotensin II formation in human internal mammary arteries. Br. J. Pharmacol. 1998, 125, 1028–1032.
- Ferrario, C.M.; Trask, A.J.; Jessup, J.A. Advances in biochemical and functional roles of angiotensin-converting enzyme 2 and angiotensin-(1–7) in regulation of cardiovascular function. Am. J. Physiol. Circ. Physiol. 2005, 289, H2281–H2290.
- Santos, R.A.S.; Simoes e Silva, A.C.; Maric, C.; Silva, D.M.R.; Machado, R.P.; de Buhr, I.; Heringer-Walther, S.; Pinheiro, S.V.B.; Lopes, M.T.; Bader, M.; et al. Angiotensin-(1–7) is an endogenous ligand for the G protein-coupled receptor Mas. Proc. Natl. Acad. Sci. USA 2003, 100, 8258–8263.
- Sanchis-Gomar, F.; Lavie, C.J.; Perez-Quilis, C.; Henry, B.M.; Lippi, G. Angiotensin-Converting Enzyme 2 and Antihypertensives (Angiotensin Receptor Blockers and Angiotensin-Converting Enzyme Inhibitors) in Coronavirus Disease 2019. Mayo Clin. Proc. 2020, 95, 1222–1230.
- Arendse, L.B.; Danser, A.H.J.; Poglitsch, M.; Touyz, R.M.; Burnett, J.C., Jr.; Llorens-Cortes, C.; Ehlers, M.R.; Sturrock, E.D. Novel Therapeutic Approaches Targeting the Renin-Angiotensin System and Associated Peptides in Hypertension and Heart Failure. Pharmacol. Rev. 2019, 71, 539–570.
- Zambelli, V.; Bellani, G.; Borsa, R.; Pozzi, F.; Grassi, A.; Scanziani, M.; Castiglioni, V.; Masson, S.; Decio, A.; Laffey, J.G.; et al. Angiotensin-(1-7) improves oxygenation, while reducing cellular infiltrate and fibrosis in experimental Acute Respiratory Distress Syndrome. Intensiv. Care Med. Exp. 2015, 3, 44.
- Imai, Y.; Kuba, K.; Rao, S.; Huan, Y.; Guo, F.; Guan, B.; Yang, P.; Sarao, R.; Wada, T.; Leong-Poi, H.; et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature 2005, 436, 112–116.
- Paz Ocaranza, M.; Riquelme, J.A.; García, L.; Jalil, J.E.; Chiong, M.; Santos, R.A.S.; Lavandero, S. Counter-regulatory renin–angiotensin system in cardiovascular disease. Nat. Rev. Cardiol. 2020, 17, 116–129.
- Samavati, L.; Uhal, B.D. ACE2, Much More Than Just a Receptor for SARS-COV-2. Front. Cell. Infect. Microbiol. 2020, 10, 317.
- Glowacka, I.; Bertram, S.; Herzog, P.; Pfefferle, S.; Steffen, I.; Muench, M.O.; Simmons, G.; Hofmann, H.; Kuri, T.; Weber, F.; et al. Differential downregulation of ACE2 by the spike proteins of severe acute respiratory syndrome coronavirus and human coronavirus NL63. J. Virol. 2010, 84, 1198–1205.
- Sarzani, R.; Giulietti, F.; Di Pentima, C.; Giordano, P.; Spannella, F. Disequilibrium between the classic renin-angiotensin system and its opposing arm in SARS-CoV-2-related lung injury. Am. J. Physiol. Lung Cell. Mol. Physiol. 2020, 319, L325–L336.
- Uhal, B.D.; Li, X.; Piasecki, C.C.; Molina-Molina, M. Angiotensin signalling in pulmonary fibrosis. Int. J. Biochem. Cell Biol. 2012, 44, 465–468.
- Sarzani, R.; Salvi, F.; Dessì-Fulgheri, P.; Rappelli, A. Renin–angiotensin system, natriuretic peptides, obesity, metabolic syndrome, and hypertension: An integrated view in humans. J. Hypertens. 2008, 26, 831–843.
- Sarzani, R.; Spannella, F.; Giulietti, F.; Balietti, P.; Cocci, G.; Bordicchia, M. Cardiac Natriuretic Peptides, Hypertension and Cardiovascular Risk. High Blood Press. Cardiovasc. Prev. 2017, 24, 115–126.
- Zhou, M.-S.; Schulman, I.; Zeng, Q. Link between the renin–angiotensin system and insulin resistance: Implications for cardiovascular disease. Vasc. Med. 2012, 17, 330–341.
- Achard, V.; Boullu-Ciocca, S.; Desbriere, R.; Nguyen, G.; Grino, M. Renin receptor expression in human adipose tissue. Am. J. Physiol. Integr. Comp. Physiol. 2007, 292, R274–R282.
- de Leeuw, A.J.M.; Luttikhuis, M.A.M.O.; Wellen, A.C.; Müller, C.; Calkhoven, C.F. Obesity and its impact on COVID-19. J. Mol. Med. 2021, 99, 899–915.
- Papannarao, J.B.; Schwenke, D.O.; Manning, P.; Katare, R. Upregulated miR-200c is associated with downregulation of the functional receptor for severe acute respiratory syndrome coronavirus 2 ACE2 in individuals with obesity. Int. J. Obes. 2021, 1–4.
- Ibrahim, H.S.; Froemming, G.; Omar, E.; Singh, H.J. ACE2 activation by xanthenone prevents leptin-induced increases in blood pressure and proteinuria during pregnancy in Sprague-Dawley rats. Reprod. Toxicol. 2014, 49, 155–161.
- Sarzani, P.; Dessì-Fulgheri, P.; Paci, V.M.; Espinosa, E.; Rappelli, A. Expression of natriuretic peptide receptors in human adipose and other tissues. J. Endocrinol. Investig. 1996, 19, 581–585.
- Shah, A.; Gul, R.; Yuan, K.; Gao, S.; Oh, Y.-B.; Kim, U.-H.; Kim, S.H. Angiotensin-(1–7) stimulates high atrial pacing-induced ANP secretion via Mas/PI3-kinase/Akt axis and Na+/H+ exchanger. Am. J. Physiol. Circ. Physiol. 2010, 298, H1365–H1374.
- Rubattu, S.; Gallo, G.; Volpe, M. A Contemporary View of Natriuretic Peptides in the SARS-CoV-2 Era. Front. Physiol. 2021, 12, 643721.
- Montefusco, L.; Ben Nasr, M.; D’Addio, F.; Loretelli, C.; Rossi, A.; Pastore, I.; Daniele, G.; Abdelsalam, A.; Maestroni, A.; Dell’Acqua, M.; et al. Acute and long-term disruption of glycometabolic control after SARS-Cov-2 infection. Nat. Metab. 2021, 3, 774–785.
- Rubino, F.; Amiel, S.A.; Zimmet, P.; Alberti, G.; Bornstein, S.; Eckel, R.H.; Mingrone, G.; Boehm, B.; Cooper, M.E.; Chai, Z.; et al. New-Onset Diabetes in COVID-19. N. Engl. J. Med. 2020, 383, 789–790.
- Sarzani, R.; Spannella, F.; Giulietti, F.; Di Pentima, C.; Giordano, P.; Giacometti, A. Possible harm from glucocorticoid drugs misuse in the early phase of SARS-CoV-2 infection: A narrative review of the evidence. Intern. Emerg. Med. 2021, 1–10.
- Yang, J.-K.; Lin, S.-S.; Ji, X.-J.; Guo, L.-M. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010, 47, 193–199.
- Guo, W.; Li, M.; Dong, Y.; Zhou, H.; Zhang, Z.; Tian, C.; Qin, R.; Wang, H.; Shen, Y.; Du, K.; et al. Diabetes is a risk factor for the progression and prognosis of COVID -19. Diabetes/Metabolism Res. Rev. 2020, 36, e3319.
- Katulanda, P.; Dissanayake, H.A.; Ranathunga, I.; Ratnasamy, V.; Wijewickrama, P.S.A.; Yogendranathan, N.; Gamage, K.K.K.; De Silva, N.L.; Sumanatilleke, M.; Somasundaram, N.P.; et al. Prevention and management of COVID-19 among patients with diabetes: An appraisal of the literature. Diabetologia 2020, 63, 1440–1452.
- Patel, V.; Parajuli, N.; Oudit, G.Y. Role of angiotensin-converting enzyme 2 (ACE2) in diabetic cardiovascular complications. Clin. Sci. 2014, 126, 471–482.
- Bornstein, S.R.; Dalan, R.; Hopkins, D.; Mingrone, G.; Boehm, B.O. Endocrine and metabolic link to coronavirus infection. Nat. Rev. Endocrinol. 2020, 16, 297–298.
- Santos, A.; Magro, D.O.; Evangelista-Poderoso, R.; Saad, M.J.A. Diabetes, obesity, and insulin resistance in COVID-19: Molecular interrelationship and therapeutic implications. Diabetol. Metab. Syndr. 2021, 13, 1–14.
- Hsueh, W.A.; Quiñones, M.J. Role of endothelial dysfunction in insulin resistance. Am. J. Cardiol. 2003, 92, 10J–17J.
- Baral, R.; Tsampasian, V.; Debski, M.; Moran, B.; Garg, P.; Clark, A.; Vassiliou, V.S. Association Between Renin-Angiotensin-Aldosterone System Inhibitors and Clinical Outcomes in Patients With COVID-19. JAMA Netw. Open 2021, 4, e213594.
- Sarzani, R.; Bordicchia, M.; Spannella, F.; Dessì-Fulgheri, P.; Fedecostante, M. Hypertensive heart disease and obesity: A complex interaction between hemodynamic and not hemodynamic factors. High Blood Press. Cardiovasc. Prev. 2014, 21, 81–87.
- Silva-Aguiar, R.P.; Peruchetti, D.B.; Rocco, P.R.M.; Schmaier, A.H.; e Silva, P.M.R.; Martins, M.A.; Carvalho, V.F.; Pinheiro, A.A.S.; Caruso-Neves, C. Role of the renin-angiotensin system in the development of severe COVID-19 in hypertensive patients. Am. J. Physiol. Lung Cell. Mol. Physiol. 2020, 319, L596–L602.
- Wingler, K.; Wünsch, S.; Kreutz, R.; Rothermund, L.; Paul, M.; Schmidt, H.H. Upregulation of the vascular NAD(P)H-oxidase isoforms Nox1 and Nox4 by the renin-angiotensin system in vitro and in vivo. Free Radic. Biol. Med. 2001, 31, 1456–1464.
- Crackower, M.A.; Sarao, R.; Oudit, G.Y.; Yagil, C.; Kozieradzki, I.; Scanga, S.E.; Oliveira-dos-Santos, A.J.; da Costa, J.; Zhang, L.; Pei, Y.; et al. Angiotensin-converting enzyme 2 is an essential regulator of heart function. Nature 2002, 417, 822–828.
- Liu, Y.; Pan, Y.; Yin, Y.; Chen, W.; Li, X. Association of dyslipidemia with the severity and mortality of coronavirus disease 2019 (COVID-19): A meta-analysis. Virol. J. 2021, 18, 157.
- Atmosudigdo, I.S.; Pranata, R.; Lim, M.A.; Henrina, J.; Yonas, E.; Vania, R.; Radi, B. Dyslipidemia Increases the Risk of Severe COVID-19: A Systematic Review, Meta-analysis, and Meta-regression. J. Clin. Exp. Hepatol. 2021, 14, 1179551421990675.
- Bellia, A.; Andreadi, A.; Giudice, L.; De Taddeo, S.; Maiorino, A.; D’Ippolito, I.; Giorgino, F.M.; Ruotolo, V.; Romano, M.; Magrini, A.; et al. Atherogenic Dyslipidemia on Admission Is Associated with Poorer Outcome in People With and Without Diabetes Hospitalized for COVID-19. Diabetes Care 2021, 44, 2149–2157.
- Mo, P.; Xing, Y.; Xiao, Y.; Deng, L.; Zhao, Q.; Wang, H.; Xiong, Y.; Cheng, Z.; Gao, S.; Liang, K.; et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin. Infect. Dis. 2021, 73, e4208–e4213.
- Williamson, E.J.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P.; et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020, 584, 430–436.
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574–1581.
- Iaccarino, G.; Grassi, G.; Borghi, C.; Carugo, S.; Fallo, F.; Ferri, C.; Giannattasio, C.; Grassi, D.; Letizia, C.; Mancusi, C.; et al. Gender differences in predictors of intensive care units admission among COVID-19 patients: The results of the SARS-RAS study of the Italian Society of Hypertension. PLoS ONE 2020, 15, e0237297.
- White, M.C.; Fleeman, R.; Arnold, A.C. Sex differences in the metabolic effects of the renin-angiotensin system. Biol. Sex Differ. 2019, 10, 31.
- Bukowska, A.; Spiller, L.; Wolke, C.; Lendeckel, U.; Weinert, S.; Hoffmann, J.; Bornfleth, P.; Kutschka, I.; Gardemann, A.; Isermann, B.; et al. Protective regulation of the ACE2/ACE gene expression by estrogen in human atrial tissue from elderly men. Exp. Biol. Med. 2017, 242, 1412–1423.
- Komukai, K.; Mochizuki, S.; Yoshimura, M. Gender and the renin-angiotensin-aldosterone system. Fundam. Clin. Pharmacol. 2010, 24, 687–698.
- Culebras, E.; Hernández, F. ACE2 is on the X chromosome: Could this explain COVID-19 gender differences? Eur. Heart J. 2020, 41, 3095.
- Gupte, M.; Thatcher, S.E.; Boustany-Kari, C.M.; Shoemaker, R.; Yiannikouris, F.; Zhang, X.; Karounos, M.; Cassis, L.A. Angiotensin converting enzyme 2 contributes to sex differences in the development of obesity hypertension in C57BL/6 mice. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 1392–1399.
- Toering, T.J.; Gant, C.M.; Visser, F.W.; van der Graaf, A.M.; Laverman, G.D.; Danser, A.H.J.; Faas, M.M.; Navis, G.; Lely, A.T. Sex differences in renin-angiotensin-aldosterone system affect extracellular volume in healthy subjects. Am. J. Physiol. Renal Physiol. 2018, 314, F873–F878.
- Polidori, M.C.; Sies, H.; Ferrucci, L.; Benzing, T. COVID-19 mortality as a fingerprint of biological age. Ageing Res. Rev. 2021, 67, 101308.
- Xie, X.; Chen, J.; Wang, X.; Zhang, F.; Liu, Y. Age- and gender-related difference of ACE2 expression in rat lung. Life Sci. 2006, 78, 2166–2171.
- AlGhatrif, M.; Cingolani, O.; Lakatta, E.G. The Dilemma of Coronavirus Disease 2019, Aging, and Cardiovascular Disease: Insights from Cardiovascular Aging Science. JAMA Cardiol. 2020, 5, 747–748.
- Spannella, F.; Di Pentima, C.; Giulietti, F.; Buscarini, S.; Ristori, L.; Giordano, P.; Sarzani, R. Prevalence of Subclinical Carotid Atherosclerosis and Role of Cardiovascular Risk Factors in Older Adults: Atherosclerosis and Aging are Not Synonyms. High blood Press. Cardiovasc. Prev. Off. J. Ital. Soc. Hypertens. 2020, 27, 231–238.
