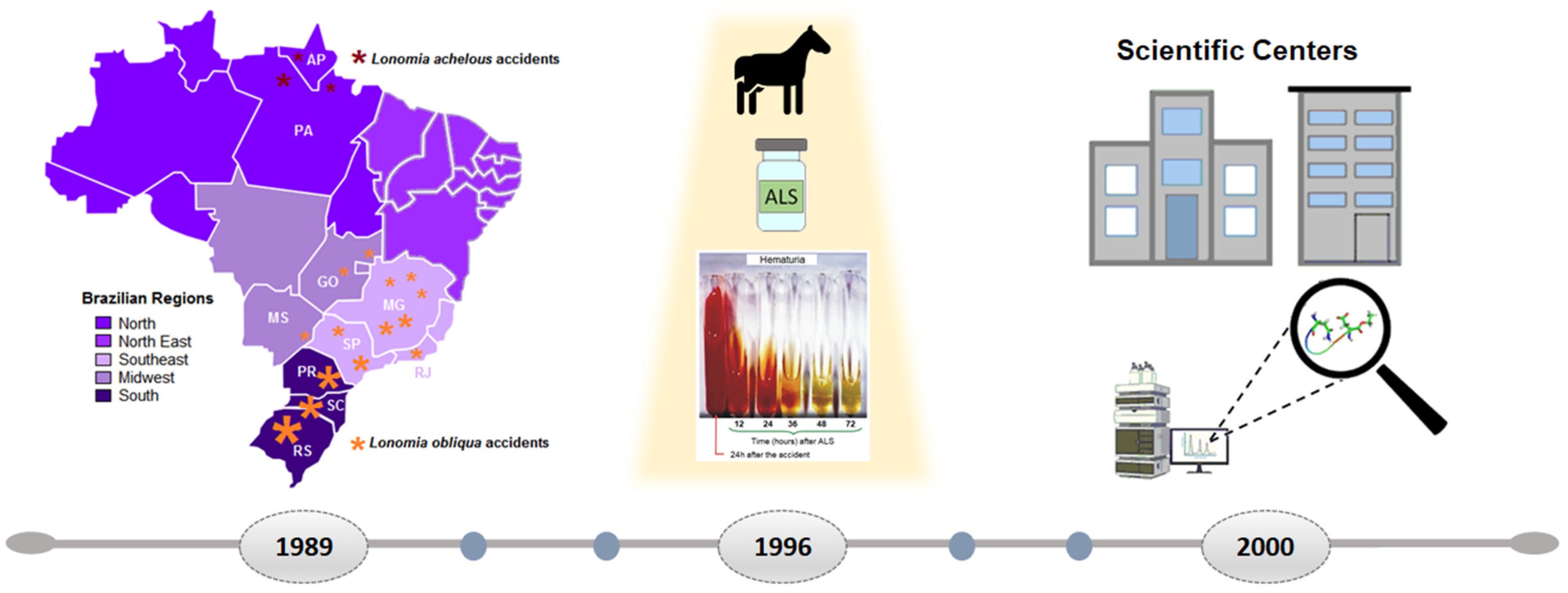
The hemorrhagic syndrome is one of the most serious complications in patients who have been in contact with the Lonomia caterpillar bristles. Although 26 species of the genus Lonomia (Saturniidae family) are distributed in the American continent, the most studied species are L. obliqua and L. achelous caterpillars; both are capable of inducing hemorrhagic effects in humans. Envenoming by L. obliqua caterpillars was considered a public health problem in southern Brazil. The hemostatic disturbances observed in the envenoming by L. obliqua caterpillars, result in a consumption coagulopathy, resembling a disseminated intravascular coagulation (DIC) and secondary fibrinolysis, which can lead to the hemorrhagic syndrome. The main complication of L. obliqua envenomation is acute renal failure, which can occur in up to 12% of the cases, being frequent in patients over 45 years old and in those with heavy bleeding. Besides that, some deaths related to hemorrhage and renal failure have been reported. However, the early diagnosis and proper treatment with antilonomic serum (ALS), produced by the Butantan Institute (SP/Brazil), within 12 h of contact can prevent severe coagulopathy and hemorrhage events.
- envenoming
- innovation
- Lonomia
1. Introduction
2. Effect of LOCBE and Toxins in the Inflammatory Response
3. Concluding Remarks
References
- Villas-Boas, I.M.; Alvarez-Flores, M.P.; Chudzinski-Tavassi, A.M.; Tambourgi, D.V. Envenomation by caterpillars. In Clinical Toxinology; Gopalakrishnakone, P., Faiz, S., Gnanathasan, C., Habib, A., Fernando, R., Yang, C.C., Eds.; Springer: Dordrecht, The Netherlands, 2016.
- Seldeslachts, A.; Peigneur, S.; Tytgat, J. Caterpillar Venom: A Health Hazard of the 21st Century. Biomedicines 2020, 8, 143.
- Da Silva, W.D.; Campos, C.M.; Gonçalves, L.R.; Sousa-E-Silva, M.C.; Higashi, H.G.; Yamagushi, I.K.; Kelen, E.M. Development of an antivenom against toxins of Lonomia obliqua caterpillars. Toxicon 1996, 34, 1045–1049.
- Rocha-Campos, A.C.; Gonçalves, L.R.; Higashi, H.G.; Yamagushi, I.K.; Fernandes, I.; Oliveira, J.E.; Ribela, M.T.; Sousa-E-Silva, M.C.; da Silva, W.D. Specific heterologous F(ab’)2 antibodies revert blood incoagulability resulting from envenoming by Lonomia obliqua caterpillars. Am. J. Trop. Med. Hyg. 2001, 64, 283–289.
- Caovilla, J.J.; José Guardão Barros, E. Efficacy of two different doses of antilonomic serum in the resolution of hemorrhagic syndrome resulting from envenoming by Lonomia obliqua caterpillars: A randomized controlled trial. Toxicon 2004, 43, 811–818.
- Gonçalves, L.R.; Souza-E-Silva, M.C.; Tomy, S.C.; Sano-Martins, I.S. Efficacy of serum therapy on the treatment of rats experimentally envenomed by bristle extract of the caterpillar Lonomia obliqua: Comparison with epsilon-aminocaproic acid therapy. Toxicon 2007, 50, 349–356.
- Sano-Martins, I.S.; González, C.; Anjos, I.V.; Díaz, J.; Gonçalves, L.R.C. Effectiveness of Lonomia antivenom in recovery from the coagulopathy induced by Lonomia orientoandensis and Lonomia casanarensis caterpillars in rats. PLoS Negl. Trop. Dis. 2018, 12, e0006721.
- Zannin, M.; Lourenço, D.M.; Motta, G.; Dalla Costa, L.R.; Grando, M.; Gamborgi, G.P.; Noguti, M.A.; Chudzinski-Tavassi, A.M. Blood coagulation and fibrinolytic factors in 105 patients with hemorrhagic syndrome caused by accidental contact with Lonomia obliqua caterpillar in Santa Catarina, southern Brazil. Thromb. Haemost. 2003, 89, 355–364.
- Favalesso, M.M.; Cuervo, P.F.; Casafús, M.G.; Guimarães, A.T.B.; Peichoto, M.E. Lonomia envenomation in Brazil: An epidemiological overview for the period 2007–2018. Trans. R. Soc. Trop. Med. Hyg. 2021, 115, 9–19.
- Brazilian Ministry of Health. SINAN, Sistema de Informação de Agravos de Notificação (Information System for Notification of Diseases). Available online: http://tabnet.datasus.gov.br/cgi/menu_tabnet_php.htm (accessed on 31 August 2021).
- Alvarez Flores, M.P.; Zannin, M.; Chudzinski-Tavassi, A.M. New Insight into the Mechanism of Lonomia obliqua envenoming: Toxin involvement and molecular approach. Pathophysiol. Haemost. Thromb. 2010, 37, 1–16.
- Chudzinski-Tavassi, A.M.; Alvarez-Flores, M.P.; Carrijo-Carvalho, L.C.; Ricci-Silva, M.E. Toxins from Lonomia obliqua: Recombinant production and molecular approach. In An Integrated View of the Molecular Recognition and Toxinology—From Analytical Procedures to Biomedical Applications; Baptista, G.R., Ed.; InTech: Rijeka, Croatia, 2013; pp. 1–32.
- Chudzinski-Tavassi, A.M.; Alvarez Flores, M.P. Exploring new molecules and activities from Lonomia obliqua caterpillars. Pathophysiol. Haemost. Thromb. 2005, 34, 228–233.
- Sano-Martins, I.S.; Duarte, A.C.; Guerrero, B.; Moraes, R.H.P.; Barros, E.J.G.; Arocha-Piñango, C.L. Hemostatic disorders induced by skin contact with Lonomia obliqua (Lepidoptera, Saturniidae) caterpillars. Rev. Inst. Med. Trop. Sao Paulo 2017, 59.
- Chudzinski-Tavassi, A.M.; Zannin, M. Aspectos clínicos y epidemiológicos del envenenamiento por Lonomia obliqua. In Emergencias por Animales Ponzoñosos en las Américas; D’Suze, G., Corzo Burguete, G.A., Paniagua Solis, J.F., Eds.; Instituto Bioclon: Mexico City, Mexico, 2011; pp. 303–321.
- de Castro Bastos, L.; Veiga, A.B.; Guimarães, J.A.; Tonussi, C.R. Nociceptive and edematogenic responses elicited by a crude bristle extract of Lonomia obliqua caterpillars. Toxicon 2004, 43, 273–278.
- Bohrer, C.B.; Reck Junior, J.; Fernandes, D.; Sordi, R.; Guimarães, J.A.; Assreuy, J.; Termignoni, C. Kallikrein–kinin system activation by Lonomia obliqua caterpillar bristles: Involvement in edema and hypotension responses to envenomation. Toxicon 2007, 49, 663–669.
- Björkqvist, J.; Jämsä, A.; Renné, T. Plasma kallikrein: The bradykinin-producing enzyme. Thromb. Haemost. 2013, 110, 399–407.
- Zanon, P.; Pizzato, S.B.; da Rosa, R.L.; Terraciano, P.B.; Moraes, J.A.; Beys-da-Silva, W.O.; Santi, L.; Yates, J.R., 3rd; Passos, E.P.; Barja-Fidalgo, C.; et al. Urine proteomic analysis reveals alterations in heme/hemoglobin and aminopeptidase metabolism during Lonomia obliqua venom-induced acute kidney injury. Toxicol. Lett. 2021, 341, 11–22.
- Berger, M.; Santi, L.; Beys-da-Silva, W.O.; Oliveira, F.M.S.; Caliari, M.V.; Yates, J.R., 3rd; Vieira, M.A.; Guimarães, J.A. Mechanisms of acute kidney injury induced by experimental Lonomia obliqua envenomation. Arch. Toxicol. 2015, 89, 459–483.
- Berger, M.; de Moraes, J.A.; Beys-da-Silva, W.O.; Santi, L.; Terraciano, P.B.; Driemeier, D.; Cirne-Lima, E.O.; Passos, E.P.; Vieira, M.; Barja-Fidalgo, T.C.; et al. Renal and vascular effects of kallikrein inhibition in a model of Lonomia obliqua venom-induced acute kidney injury. PLoS Negl. Trop. Dis. 2019, 13, e0007197.
- Nourshargh, S.; Alon, R. Leukocyte Migration into Inflamed Tissues. Immunity 2014, 41, 694–707.
- Pinto, A.F.M.; Dragulev, B.; Guimarães, J.A.; Fox, J.W. Novel perspectives on the pathogenesis of Lonomia obliqua caterpillar envenomation based on assessment of host response by gene expression analysis. Toxicon 2008, 51, 1119–1128.
- Claesson-Welsh, L. Vascular permeability—The essentials. Upsala J. Med. Sci. 2015, 120, 135–143.
- Moraes, J.; Rodrigues, G.; Nascimento-Silva, V.; Renovato-Martins, M.; Berger, M.; Guimarães, J.; Barja-Fidalgo, C. Effects of Lonomia obliqua Venom on Vascular Smooth Muscle Cells: Contribution of NADPH Oxidase-Derived Reactive Oxygen Species. Toxins 2017, 9, 360.
- Berger, M.; Beys-da-Silva, W.O.; Santi, L.; de Oliveira, I.M.; Jorge, P.M.; Henriques, J.A.; Driemeier, D.; Vieira, M.A.; Guimarães, J.A. Acute Lonomia obliqua caterpillar envenomation-induced physiopathological alterations in rats: Evidence of new toxic venom activities and the efficacy of serum therapy to counteract systemic tissue damage. Toxicon 2013, 74, 179–192.
- Nascimento-Silva, V.; Rodrigues da Silva, G.; Moraes, J.A.; Cyrino, F.Z.; Seabra, S.H.; Bouskela, E.; Almeida Guimarães, J.; Barja-Fidalgo, C. A pro-inflammatory profile of endothelial cell in Lonomia obliqua envenomation. Toxicon 2012, 60, 50–60.
- Oliveira, D.S.; de Souza, J.G.; Alvarez-Flores, M.P.; Cunegundes, P.S.; DeOcesano-Pereira, C.; Lobba, A.M.; Gomes, R.N.; Chudzinski-Tavassi, A.M. Lonomia obliqua Venom Induces NF-κB Activation and a Pro-Inflammatory Profile in THP-1-Derived Macrophage. Toxins 2021, 13, 462.
- Chen, L.; Deng, H.; Cui, H.; Fang, J.; Zuo, Z.; Deng, J.; Li, Y.; Wang, X.; Zhao, L. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget 2018, 9, 7204–7218.
- Fritzen, M.; Flores, M.P.A.; Reis, C.V.; Chudzinski-Tavassi, A.M. A prothrombin activator (Lopap) modulating inflammation, coagulation and cell survival mechanisms. Biochem. Biophys. Res. Commun. 2005, 333, 517–523.
- Bernardi, L.; Pinto, A.F.M.; Mendes, E.; Yates, J.R.; Lamers, M.L. Lonomia obliqua bristle extract modulates Rac1 activation, membrane dynamics and cell adhesion properties. Toxicon 2019, 162, 32–39.
