Hepatic artery infusion chemotherapy (HAIC) is a well-established and common treatment for advanced hepatocellular carcinoma (HCC), particularly in East Asia. However, HAIC is not recognized internationally. Although several trials have demonstrated the safety and efficacy of HAIC, evidence corroborating its overall survival (OS) benefits compared with standard treatments is insufficient. Nevertheless, HAIC may provide prominent benefits in selected patients such as patients with portal vein thrombosis or high intrahepatic tumor burden. Moreover, HAIC has been combined with several therapeutic agents and modalities, including interferon-alpha, multikinase inhibitors, radiation therapy, and immunotherapy, to augment its treatment efficacy. Most of these combinations appeared to increase overall response rates compared with HAIC alone, but results regarding OS are inconclusive. Two prospective randomized controlled trials comparing HAIC plus sorafenib with sorafenib alone have reported conflicting results, necessitating further research. As immunotherapy-based combinations became the mainstream treatments for advanced HCC, HAIC plus immunotherapy-based treatments also showed encouraging preliminary results. The trials of HAIC were heterogeneous in terms of patient selection, chemotherapy regimens and doses, HAIC combination agent selections, and HAIC technical protocols. These heterogeneities may contribute to differences in treatment efficacy, thus increasing the difficulty of interpreting trial results.
- hepatocellular carcinoma
- intra-arterial chemotherapy
- targeted therapy
- immunotherapy
1. Introduction
2. HAIC Monotherapy
| Group | Study Type/Characteristics | Patient Number | Regimen | CP-B (%) | HBV (%) | PVT (%) | EHS (%) | ORR (%) | OS (Months) |
p-Value (OS) |
|---|---|---|---|---|---|---|---|---|---|---|
| Song et al. [13] | Retrospective PVT |
50 | Cisplatin 60 mg/m2, Day 2 5-FU 500 mg/m |
3. HAIC-Based Combination Therapy
| Group | Study Design | Patient Number (N) | Regimen | CP-B (%) | HBV (%) | PVT (%) | EHS (%) | ORR (%) | OS (Months) |
p-Value (OS) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2 | , Days 1–3 | +/− Epirubicin 35 mg/m2, Day 1 (every 3–4 weeks) |
10.0 | 88.0 | 100 | 13.0 | 24.0 | 7.1 | 0.011 | |||||||||||
| INF-α | 60 | Sorafenib | 21.7 | 68.3 | 100 | 35.0 | 13.3 | 5.5 | ||||||||||||
| Sakon et al. | ||||||||||||||||||||
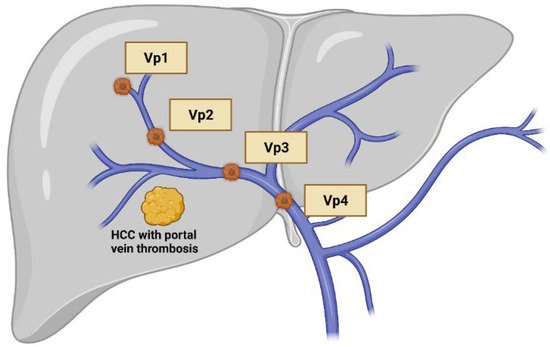
| [36] | Phase 2 single arm VP3–4, no EHS |
11 | 5-FU 450–500 mg/m2, Days 1–5 INF-α5MU qW1,3,5 |
54.5 | 36.4 | 100 | 0 | 72.7 | 8.0 | Hatooka et al. [14] | Retrospective Refractory to TACE |
|||||||||
| Eun et al. [37] | Retrospective65 | single armCisplatin 6 mg/m2, Days 1–5, 8–12 |
31 5-FU 300 mg/m2, Days 1–5, 8–12 * (every 4 weeks) |
HAIC: 5-FU 750 mg/m2, 0 | cisplatin 25 mg/m2, Days 1–4 INF-α 3MU Days 1–4, then QOD23.1 |
35.4 (Vp3–4) |
0 | 19.412.0 | 83.9 | 100 | NR | 19.48.0 | 0.021 | |||||||
| 4.0 | 0.353 | |||||||||||||||||||
| 58 | Sorafenib | 21 | HAIC alone: 5-FU 750 mg/m0 |
2, 22.4 |
cisplatin 25 mg/m2, Days 1–410.3 (Vp3–4) |
19.0 | 85.7 | 1000 | 6.0 | 15.0 | ||||||||||
| NR | 42.9 | 7.0 | Moriguchi et al. [15] | Retrospective Vp3–4 |
32 | Cisplatin 10 mg/m2, Day 1; 5-FU 250 mg/m2, Days 1–5 (weekly for 4 weeks, then only Day 1 per week) |
0 | 37.5 | 100 | 21.9 | 31.3 | 10.3 | ||||||||
| Sorafenib | 0.009 | |||||||||||||||||||
| 14 | Sorafenib | 0 | 28.6 | 100 | 35.7 | 0 | 4.0 | |||||||||||||
| Nakano et al. [16] | Retrospective With MVI, without EHS |
44 | Cisplatin 50 mg/m2 in 5–10 mL lipiodol, Day 1 5-FU 1500 mg/m2 for 5 day for 2 weeks then cisplatin 25–30 mg/m2 + 5FU 500–1000 mg/m2 (ever 2 weeks) |
0 | 14.0 | 100 | 0 | 71.0 | 30.4 | <0.001 | ||||||||||
| 20 | Sorafenib | 0 | 25.0 | 100 | 0 | 10.0 | 13.2 | |||||||||||||
| 8–12 (every 4 weeks) | Plus sorafenib | 11.7 | 25.5 | 56.9 | 26.5 | 36.0 (mRECIST) |
11.8 | 0.995 | Kodama et al. [17] | Retrospective No EHS |
150 | Cisplatin 6 mg/m2, Days 1–5, 8–12 5-FU 300 mg/m2, Days 1–5, 8–12 (every 4 weeks) |
0 | 25.3 | 73.3 | 0 | 32.0 | |||
| 10.0 | 103 | Sorafenib | 9.7 | 21.4 | 62.1 | 25.2 | 0.007 | |||||||||||||
| 18.0 | (mRECIST) | 11.5 | 134 | Sorafenib | 0 | 16.4 | 29.1 | 0 | 4.0 | 19.0 | ||||||||||
| Zhao et al. [40] | Retrospective CPS-A |
46 | Oxaliplatin 85 mg/m2, Day 1 (every 3 weeks) Plus sorafenib |
0 | 84.8 | 89.1 (VP3–4) |
19.6 | 34.8 | 9.4 | <0.01 | Lyu et al. [18] | Retrospective HAIC for patients who refused sorafenib |
180 | mFOLFOX 6 (HAIC) (every 3 weeks) |
0 | 86.7 | ||||
| 58 | 54.4 | 60 | 29.4 | 14.5 | <0.001 | |||||||||||||||
| Sorafenib | 0 | 89.7 | 84.5 | 27.6 | 1.7 | 4.8 | 232 | Sorafenib | 0 | 80.2 | 55.6 | 58.6 | 3.0 | 7.0 | ||||||
| He et al. [41] | Kondo et al. [19] | Randomized Phase 2 (CP-A to B7) |
35 | Cisplatin 65 mg/m2, Day 1 (every 4–6 weeks) |
11.4 | 8.6 | 60.0 | 28.6 | 14.3 | 10.0 | 0.780 | |||||||||
| 33 | Sorafenib | 12.1 | 12.1 | 66.7 | 24.2 | 9.1 | 15.2 | |||||||||||||
| Phase 3 | PVT CPS-A |
125 | mFOLFOX 6, Days 1–3 (every 3 weeks) Plus sorafenib |
0 | 80.0 | 100 | 30.4 | 40.8 | 13.4 | <0.01 | ||||||||||
| 122 | Sorafenib | 0 | 81.1 | 100 | 34.4 | 2.5 | 7.1 | |||||||||||||
| Lenvatinib | Ahn et al. [20] | Retrospective VP4 |
38 | Cisplatin 60 mg/m | ||||||||||||||||
| Mai et al. [42] | Retrospective Single arm | 2, Day 1 5-FU 500 mg/m2, Days 1–3 |
29.0 | 86.8 | 24 | mFOLFOX 6, Days 1–3 (every 3 weeks) | 100 | 5.3 | 5.2 | 10 | 0.150 | |||||||||
| plus lenvatinib | 16.7 | 10.3 | 35 | Sorafenib | 31.0 | 69.0 | 100 | 46 | 0 | 6.4 | ||||||||||
| Ueshima et al. [21] | Retrospective Cohort 1 with MVI, Without EHS |
270 | Cisplatin + 5FU or 5-FU or cisplatin (detail of regimens were not reported) |
36.9 | 23.0 | 100 | 0 | NR | 10.6 | 0.475 | ||||||||||
| 263 | Sorafenib | 16.0 | 21.3 | 100 | 0 | NR | 9.1 | |||||||||||||
| Zaizen et al. [22] | Retrospective Propensity score-matched |
83 | Cisplatin 65 mg/m2, Day 1 (every 8–12 weeks) |
36.1 | 7.2 | 14 (MVI) |
0 | NR | 15.6 | 0.016 | ||||||||||
| 83 | Sorafenib | 28.9 | 8.4 | 11(MVI) | 0 | NR | 11.0 | |||||||||||||
| Lyu et al. [23] | Randomized Phase 3 | 130 | mFOLFOX 6 (HAIC) every 3 weeks |
NR | NR | NR | NR | NR | 13.9 | <0.001 | ||||||||||
| 132 | Sorafenib | NR | NR | NR | MR | NR | 8.2 |
| Ikeda et al. | ||||||||||
| [ | ||||||||||
| 38 | ||||||||||
| ] | ||||||||||
| Randomized | Phase 2 CPS-A, B7 |
65 | Cisplatin 65 mg/m2, Day 1 Every 4–6 weeks plus sorafenib |
12.3 | 33.8 | 61.5 | 29.2 | 21.7 | 10.8 | 0.031 |
| 41 | Sorafenib | 4.9 | 22.0 | 41.5 | 31.7 | 7.3 | 8.7 | |||
| Kudo et al. [39] | Phase 3 CPS-A, B7 |
102 | Cisplatin 20 mg/m2, Day 1, 8 5-FU 330 mg/m2 Days 1–5, | |||||||
| NR | ||||||||||
| NR | ||||||||||
| 58.3 | 12 m OS 75% | |||||||||
| IO-based | ||||||||||
| Gu et al. [43] | Retrospective Single arm |
6 | mFOLFOX 6, Days 1–3 (every 3 weeks) Apatinib 250 mg QD (since D8) Toripalimab 240 mg D4, |
0 | NR | 100 | 33.3 | 100 | NR | |
| He et al. [44] | Retrospective | 71 | mFOLFOX 6, Days 1–3 Lenvatinib Toripalimab 240 mg per session |
0 | 87.3 | 77.5 | 22.5 | 59.2 | NR | <0.001 |
| 86 | Lenvatinib | 0 | 90.7 | 72.1 | 29.1 | 9.3 | 11 | |||
| RT | ||||||||||
| Han et al. [45] | Prospective Single arm PVT |
40 | 5-FU 500 mg/m2, Days 1–3 cisplatin 60 mg/m2, Day 2 plus RT |
0 | 92.5 | 100 | NR | 45 | 13.1 | |
| Katamura et al. [46] | Retrospective PVT |
16 | 5-FU 500 mg/m2, Days 1–5 plus RT |
25.0 | 25.0 | 100 | 37.5 | 75.0 | 7.5 | 0.871 |
| 16 | 5-FU 500 mg/m2, Days 1–5 | 18.8 | 31.3 | 100 | 25.0 | 25.0 | 7.9 | |||
| Fujino et al. [47] | Retrospective PVT, VP3–4 No EHS |
41 | cisplatin 20 mg/m2, Day 1, 8 5-FU 330 mg/m2 Days 1–5, 8–12 INF-α: recombinant 3MU or natural 5MU plus RT |
19.5 | 26.5 | 100 | 0 | 56.1 | 12.1 | 0.309 |
| 42 | HAIC plus INF-α as above | 23.8 | 23.8 | 100 | 0 | 33.3 | 7.2 | |||
| Kodama et al. [48] | Retrospective PVT and CPS-A, B7 |
68 | Cisplatin 20 mg/m2, day 1, 8 5-FU 330 mg/m2, Days 1–5, 8–12 (5-FU only in cycle 1–2) plus RT |
20.6 | 29.4 | 100 | 19.1 | 27.8 | 9.9 | 0.02 |
| 40 | Sorafenib | 12.5 | 42.5 | 100 | 40.0 | 6.7 | 5.3 |
3.1. HAIC Plus Subcutaneous Interferon-Alpha
3.2. HAIC Plus Multikinase Inhibitors
3.3. HAIC Plus Radiation Therapy
3.4. HAIC Plus Immunotherapy
References
- Shao, Y.Y.; Huang, C.C.; Liang, P.C.; Lin, Z.Z. Hepatic arterial infusion of chemotherapy for advanced hepatocellular carcinoma. Asia-Pac. J. Clin. Oncol. 2010, 6, 80–88.
- Pinter, M.; Hucke, F.; Graziadei, I.; Vogel, W.; Maieron, A.; Königsberg, R.; Stauber, R.; Grünberger, B.; Müller, C.; Kölblinger, C.; et al. Advanced-stage hepatocellular carcinoma: Transarterial chemoembolization versus sorafenib. Radiology 2012, 263, 590–599.
- Vilgrain, V.; Pereira, H.; Assenat, E.; Guiu, B.; Ilonca, A.D.; Pageaux, G.P.; Sibert, A.; Bouattour, M.; Lebtahi, R.; Allaham, W.; et al. Efficacy and safety of selective internal radiotherapy with yttrium-90 resin microspheres compared with sorafenib in locally advanced and inoperable hepatocellular carcinoma (SARAH): An open-label randomised controlled phase 3 trial. Lancet Oncol. 2017, 18, 1624–1636.
- Chow, P.K.; Gandhi, M.; Tan, S.B.; Khin, M.W.; Khasbazar, A.; Ong, J.; Choo, S.P.; Cheow, P.C.; Chotipanich, C.; Lim, K.; et al. SIRveNIB: Selective Internal Radiation Therapy Versus Sorafenib in Asia-Pacific Patients With Hepatocellular Carcinoma. J. Clin. Oncol. 2018, 36, 1913–1921.
- Ando, E.; Yamashita, F.; Tanaka, M.; Tanikawa, K. A novel chemotherapy for advanced hepatocellular carcinoma with tumor thrombosis of the main trunk of the portal vein. Cancer 1997, 79, 1890–1896.
- Hsu, C.; Chen, C.N.; Chen, L.T.; Wu, C.Y.; Yang, P.M.; Lai, M.Y.; Lee, P.H.; Cheng, A.L. Low-dose thalidomide treatment for advanced hepatocellular carcinoma. Oncology 2003, 65, 242–249.
- Lai, C.L.; Wu, P.C.; Chan, G.C.; Lok, A.S.; Lin, H.J. Doxorubicin versus no antitumor therapy in inoperable hepatocellular carcinoma. A prospective randomized trial. Cancer 1988, 62, 479–483.
- Yeo, W.; Mok, T.S.; Zee, B.; Leung, T.W.; Lai, P.B.; Lau, W.Y.; Koh, J.; Mo, F.K.; Yu, S.C.; Chan, A.T.; et al. A randomized phase III study of doxorubicin versus cisplatin/interferon alpha-2b/doxorubicin/fluorouracil (PIAF) combination chemotherapy for unresectable hepatocellular carcinoma. J. Natl. Cancer Inst. 2005, 97, 1532–1538.
- Qin, S.; Bai, Y.; Lim, H.Y.; Thongprasert, S.; Chao, Y.; Fan, J.; Yang, T.S.; Bhudhisawasdi, V.; Kang, W.K.; Zhou, Y.; et al. Randomized, multicenter, open-label study of oxaliplatin plus fluorouracil/leucovorin versus doxorubicin as palliative chemotherapy in patients with advanced hepatocellular carcinoma from Asia. J. Clin. Oncol. 2013, 31, 3501–3508.
- Nouso, K.; Miyahara, K.; Uchida, D.; Kuwaki, K.; Izumi, N.; Omata, M.; Ichida, T.; Kudo, M.; Ku, Y.; Kokudo, N.; et al. Effect of hepatic arterial infusion chemotherapy of 5-fluorouracil and cisplatin for advanced hepatocellular carcinoma in the Nationwide Survey of Primary Liver Cancer in Japan. Br. J. Cancer 2013, 109, 1904–1907.
- Sumie, S.; Yamashita, F.; Ando, E.; Tanaka, M.; Yano, Y.; Fukumori, K.; Sata, M. Interventional radiology for advanced hepatocellular carcinoma: Comparison of hepatic artery infusion chemotherapy and transcatheter arterial lipiodol chemoembolization. AJR Am. J. Roentgenol. 2003, 181, 1327–1334.
- Kim, H.Y.; Kim, J.D.; Bae, S.H.; Park, J.Y.; Han, K.H.; Woo, H.Y.; Choi, J.Y.; Yoon, S.K.; Jang, B.K.; Hwang, J.S.; et al. A comparative study of high-dose hepatic arterial infusion chemotherapy and transarterial chemoembolization using doxorubicin for intractable, advanced hepatocellular carcinoma. Korean J. Hepatol. 2010, 16, 355–361.
- Song, D.S.; Song, M.J.; Bae, S.H.; Chung, W.J.; Jang, J.Y.; Kim, Y.S.; Lee, S.H.; Park, J.Y.; Yim, H.J.; Cho, S.B.; et al. A comparative study between sorafenib and hepatic arterial infusion chemotherapy for advanced hepatocellular carcinoma with portal vein tumor thrombosis. J. Gastroenterol. 2015, 50, 445–454.
- Hatooka, M.; Kawaoka, T.; Aikata, H.; Morio, K.; Kobayashi, T.; Hiramatsu, A.; Imamura, M.; Kawakami, Y.; Murakami, E.; Waki, K.; et al. Comparison of Outcome of Hepatic Arterial Infusion Chemotherapy and Sorafenib in Patients with Hepatocellular Carcinoma Refractory to Transcatheter Arterial Chemoembolization. Anticancer Res. 2016, 36, 3523–3529.
- Moriguchi, M.; Aramaki, T.; Nishiofuku, H.; Sato, R.; Asakura, K.; Yamaguchi, K.; Tanaka, T.; Endo, M.; Itoh, Y. Sorafenib versus Hepatic Arterial Infusion Chemotherapy as Initial Treatment for Hepatocellular Carcinoma with Advanced Portal Vein Tumor Thrombosis. Liver Cancer 2017, 6, 275–286.
- Nakano, M.; Niizeki, T.; Nagamatsu, H.; Tanaka, M.; Kuromatsu, R.; Satani, M.; Okamura, S.; Iwamoto, H.; Shimose, S.; Shirono, T.; et al. Clinical effects and safety of intra-arterial infusion therapy of cisplatin suspension in lipiodol combined with 5-fluorouracil versus sorafenib, for advanced hepatocellular carcinoma with macroscopic vascular invasion without extra-hepatic spread: A prospective cohort study. Mol. Clin. Oncol. 2017, 7, 1013–1020.
- Kodama, K.; Kawaoka, T.; Aikata, H.; Uchikawa, S.; Inagaki, Y.; Hatooka, M.; Morio, K.; Nakahara, T.; Murakami, E.; Tsuge, M.; et al. Comparison of clinical outcome of hepatic arterial infusion chemotherapy and sorafenib for advanced hepatocellular carcinoma according to macrovascular invasion and transcatheter arterial chemoembolization refractory status. J. Gastroenterol. Hepatol. 2018, 33, 1780–1786.
- Lyu, N.; Kong, Y.; Mu, L.; Lin, Y.; Li, J.; Liu, Y.; Zhang, Z.; Zheng, L.; Deng, H.; Li, S.; et al. Hepatic arterial infusion of oxaliplatin plus fluorouracil/leucovorin vs. sorafenib for advanced hepatocellular carcinoma. J. Hepatol. 2018, 69, 60–69.
- Kondo, M.; Morimoto, M.; Kobayashi, S.; Ohkawa, S.; Hidaka, H.; Nakazawa, T.; Aikata, H.; Hatanaka, T.; Takizawa, D.; Matsunaga, K.; et al. Randomized, phase II trial of sequential hepatic arterial infusion chemotherapy and sorafenib versus sorafenib alone as initial therapy for advanced hepatocellular carcinoma: SCOOP-2 trial. BMC Cancer 2019, 19, 954.
- Ahn, Y.E.; Suh, S.J.; Yim, H.J.; Seo, Y.S.; Yoon, E.L.; Kim, T.H.; Lee, Y.S.; Yim, S.Y.; Kim, H.R.; Kang, S.H.; et al. Comparison of Sorafenib versus Hepatic Arterial Infusion Chemotherapy-Based Treatment for Advanced Hepatocellular Carcinoma with Portal Vein Tumor Thrombosis. Gut Liver 2020, 15, 284.
- Ueshima, K.; Ogasawara, S.; Ikeda, M.; Yasui, Y.; Terashima, T.; Yamashita, T.; Obi, S.; Sato, S.; Aikata, H.; Ohmura, T.; et al. Hepatic Arterial Infusion Chemotherapy versus Sorafenib in Patients with Advanced Hepatocellular Carcinoma. Liver Cancer 2020, 9, 583–595.
- Zaizen, Y.; Nakano, M.; Fukumori, K.; Yano, Y.; Takaki, K.; Niizeki, T.; Kuwaki, K.; Fukahori, M.; Sakaue, T.; Yoshimura, S.; et al. Hepatic Arterial Infusion Chemotherapy with Cisplatin versus Sorafenib for Intrahepatic Advanced Hepatocellular Carcinoma: A Propensity Score-Matched Analysis. Cancers 2021, 13, 5282.
- Lyu, N.; Zhao, M. Hepatic arterial infusion chemotherapy of oxaliplatin plus fluorouracil versus sorafenib in advanced hepatocellular carcinoma: A biomolecular exploratory, randomized, phase 3 trial (The FOHAIC-1 study). J. Clin. Oncol. 2021, 39, 4007.
- Llovet, J.M.; Ricci, S.; Mazzaferro, V.; Hilgard, P.; Gane, E.; Blanc, J.F.; de Oliveira, A.C.; Santoro, A.; Raoul, J.L.; Forner, A.; et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 2008, 359, 378–390.
- Cheng, A.L.; Kang, Y.K.; Chen, Z.; Tsao, C.J.; Qin, S.; Kim, J.S.; Luo, R.; Feng, J.; Ye, S.; Yang, T.S.; et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: A phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009, 10, 25–34.
- Terashima, T.; Yamashita, T.; Arai, K.; Sunagozaka, H.; Kitahara, M.; Nakagawa, H.; Kagaya, T.; Mizukoshi, E.; Honda, M.; Kaneko, S. Feasibility and efficacy of hepatic arterial infusion chemotherapy for advanced hepatocellular carcinoma after sorafenib. Hepatol. Res. 2014, 44, 1179–1185.
- Terashima, T.; Yamashita, T.; Takata, N.; Arai, K.; Mizukoshi, E.; Kaneko, S. Hepatic arterial infusion chemotherapy after sorafenib treatment in patients with advanced hepatocellular carcinoma who are unfit for regorafenib. J. Clin. Oncol. 2019, 37, 355.
- Shao, Y.Y.; Liang, P.C.; Wu, Y.M.; Huang, C.C.; Huang, K.W.; Cheng, J.C.; Hsu, C.H.; Hsu, C.; Cheng, A.L.; Lin, Z.Z. A pilot study of hepatic arterial infusion of chemotherapy for patients with advanced hepatocellular carcinoma who have failed anti-angiogenic therapy. Liver Int. 2013, 33, 1413–1419.
- Tsai, W.-L.; Sun, W.-C.; Chen, W.-C.; Chiang, C.-L.; Lin, H.-S.; Liang, H.-L.; Cheng, J.-S. Hepatic arterial infusion chemotherapy vs transcatheter arterial embolization for patients with huge unresectable hepatocellular carcinoma. Medicine 2020, 99, e21489.
- Yen, Y.-H.; Cheng, Y.-F.; Wang, J.-H.; Lin, C.-C.; Chen, Y.-Y.; Yong, C.-C.; Liu, Y.-W.; Cheng, J.-Y.; Chen, C.-H.; Hu, T.-H. Real world clinical practice in treating advanced hepatocellular carcinoma: When East meets West. PLoS ONE 2020, 15, e0230005.
- Li, Q.J.; He, M.K.; Chen, H.W.; Fang, W.Q.; Zhou, Y.M.; Xu, L.; Wei, W.; Zhang, Y.J.; Guo, Y.; Guo, R.P.; et al. Hepatic Arterial Infusion of Oxaliplatin, Fluorouracil, and Leucovorin Versus Transarterial Chemoembolization for Large Hepatocellular Carcinoma: A Randomized Phase III Trial. J. Clin. Oncol. 2021, JCO–21.
- Shao, Y.Y.; Wang, S.Y.; Lin, S.M. Management consensus guideline for hepatocellular carcinoma: 2020 update on surveillance, diagnosis, and systemic treatment by the Taiwan Liver Cancer Association and the Gastroenterological Society of Taiwan. J. Formos. Med. Assoc. 2020, 120, 1051–1060.
- Kudo, M.; Matilla, A.; Santoro, A.; Melero, I.; Gracian, A.C.; Acosta-Rivera, M.; Choo, S.P.; El-Khoueiry, A.B.; Kuromatsu, R.; El-Rayes, B.F.; et al. Checkmate-040: Nivolumab (NIVO) in patients (pts) with advanced hepatocellular carcinoma (aHCC) and Child-Pugh B (CPB) status. J. Clin. Oncol. 2019, 37, 327.
- Terashima, T.; Yamashita, T.; Arai, K.; Kawaguchi, K.; Kitamura, K.; Yamashita, T.; Sakai, Y.; Mizukoshi, E.; Honda, M.; Kaneko, S. Beneficial Effect of Maintaining Hepatic Reserve during Chemotherapy on the Outcomes of Patients with Hepatocellular Carcinoma. Liver Cancer 2017, 6, 236–249.
- Liu, T.H.; Hsu, C.H.; Shao, Y.Y. Successful Hepatic Arterial Infusion of Chemotherapy in a Patient with Advanced Hepatocellular Carcinoma and Impending Liver Failure. Liver Cancer 2018, 7, 205–208.
- Sakon, M.; Nagano, H.; Dono, K.; Nakamori, S.; Umeshita, K.; Yamada, A.; Kawata, S.; Imai, Y.; Iijima, S.; Monden, M. Combined intraarterial 5-fluorouracil and subcutaneous interferon-alpha therapy for advanced hepatocellular carcinoma with tumor thrombi in the major portal branches. Cancer 2002, 94, 435–442.
- Eun, J.R.; Lee, H.J.; Moon, H.J.; Kim, T.N.; Kim, J.W.; Chang, J.C. Hepatic arterial infusion chemotherapy using high-dose 5-fluorouracil and cisplatin with or without interferon-alpha for the treatment of advanced hepatocellular carcinoma with portal vein tumor thrombosis. Scand. J. Gastroenterol. 2009, 44, 1477–1486.
- Ikeda, M.; Shimizu, S.; Sato, T.; Morimoto, M.; Kojima, Y.; Inaba, Y.; Hagihara, A.; Kudo, M.; Nakamori, S.; Kaneko, S.; et al. Sorafenib plus hepatic arterial infusion chemotherapy with cisplatin versus sorafenib for advanced hepatocellular carcinoma: Randomized phase II trial. Ann. Oncol. 2016, 27, 2090–2096.
- Kudo, M.; Ueshima, K.; Yokosuka, O.; Ogasawara, S.; Obi, S.; Izumi, N.; Aikata, H.; Nagano, H.; Hatano, E.; Sasaki, Y.; et al. Sorafenib plus low-dose cisplatin and fluorouracil hepatic arterial infusion chemotherapy versus sorafenib alone in patients with advanced hepatocellular carcinoma (SILIUS): A randomised, open label, phase 3 trial. Lancet Gastroenterol. Hepatol. 2018, 3, 424–432.
- Zhao, Y.; Lai, J.; Liang, R.; He, M.; Shi, M. Sorafenib plus hepatic arterial infusion chemotherapy with oxaliplatin versus sorafenib alone for advanced hepatocellular carcinoma. J. Interv. Med. 2019, 2, 78–83.
- He, M.; Li, Q.; Zou, R.; Shen, J.; Fang, W.; Tan, G.; Zhou, Y.; Wu, X.; Xu, L.; Wei, W.; et al. Sorafenib Plus Hepatic Arterial Infusion of Oxaliplatin, Fluorouracil, and Leucovorin vs. Sorafenib Alone for Hepatocellular Carcinoma With Portal Vein Invasion: A Randomized Clinical Trial. JAMA Oncol. 2019, 5, 953–960.
- Mai, Q.; Mo, Z.; Shi, F.; Chen, X. Lenvatinib plus hepatic arterial infusion of modified FOLFOX regime in patients with advanced hepatocellular carcinoma. J. Clin. Oncol. 2020, 38, e16603.
- Gu, Y.-K.; Zhang, T.-Q.; Huang, Z.-L.; Geng, Z.-J.; Chen, C.; Li, F.-G.; Xu, L.; Sun, J.; Li, J.; Huang, Z.-M.; et al. Hepatic artery infusion chemotherapy combined with apatinib and toripalimab in advanced hepatocellular carcinoma: Real-world data from a single center. J. Clin. Oncol. 2020, 38, e16602.
- He, M.K.; Liang, R.B.; Zhao, Y.; Xu, Y.J.; Chen, H.W.; Zhou, Y.M.; Lai, Z.C.; Xu, L.; Wei, W.; Zhang, Y.J.; et al. Lenvatinib, toripalimab, plus hepatic arterial infusion chemotherapy versus lenvatinib alone for advanced hepatocellular carcinoma. Ther Adv. Med. Oncol. 2021, 13, 17588359211002720.
- Han, K.H.; Seong, J.; Kim, J.K.; Ahn, S.H.; Lee, D.Y.; Chon, C.Y. Pilot clinical trial of localized concurrent chemoradiation therapy for locally advanced hepatocellular carcinoma with portal vein thrombosis. Cancer 2008, 113, 995–1003.
- Katamura, Y.; Aikata, H.; Takaki, S.; Azakami, T.; Kawaoka, T.; Waki, K.; Hiramatsu, A.; Kawakami, Y.; Takahashi, S.; Kenjo, M.; et al. Intra-arterial 5-fluorouracil/interferon combination therapy for advanced hepatocellular carcinoma with or without three-dimensional conformal radiotherapy for portal vein tumor thrombosis. J. Gastroenterol. 2009, 44, 492–502.
- Fujino, H.; Kimura, T.; Aikata, H.; Miyaki, D.; Kawaoka, T.; Kan, H.; Fukuhara, T.; Kobayashi, T.; Naeshiro, N.; Honda, Y.; et al. Role of 3-D conformal radiotherapy for major portal vein tumor thrombosis combined with hepatic arterial infusion chemotherapy for advanced hepatocellular carcinoma. Hepatol. Res. 2015, 45, 607–617.
- Kodama, K.; Kawaoka, T.; Aikata, H.; Uchikawa, S.; Nishida, Y.; Inagaki, Y.; Hatooka, M.; Morio, K.; Nakahara, T.; Murakami, E.; et al. Comparison of Outcome of Hepatic Arterial Infusion Chemotherapy Combined with Radiotherapy and Sorafenib for Advanced Hepatocellular Carcinoma Patients with Major Portal Vein Tumor Thrombosis. Oncology 2018, 94, 215–222.
- Kardinal, C.G.; Moertel, C.G.; Wieand, H.S.; Schutt, A.J.; O’Connell, M.J.; Wright, K.; Wiesenfeld, M.; Tschetter, L.K.; Krook, J.E. Combined doxorubicin and alpha-interferon therapy of advanced hepatocellular carcinoma. Cancer 1993, 71, 2187–2190.
- Takaki-Hamabe, S.; Yamasaki, T.; Saeki, I.; Harima, Y.; Okita, K.; Terai, S.; Sakaida, I. Hepatic arterial infusion chemotherapy for advanced hepatocellular carcinoma: Is the addition of subcutaneous interferon-alpha-2b beneficial? Hepatol. Res. 2009, 39, 223–230.
- Okita, K.; Yamasaki, T.; Hamabe, S.; Saeki, I.; Harima, Y.; Terai, S.; Sakaida, I. Hepatic arterial infusion chemotherapy in combination with pegylated interferon-α-2b for advanced hepatocellular carcinoma. Hepatogastroenterology 2012, 59, 533–537.
- Faivre, S.; Chan, D.; Salinas, R.; Woynarowska, B.; Woynarowski, J.M. DNA strand breaks and apoptosis induced by oxaliplatin in cancer cells. Biochem. Pharmacol. 2003, 66, 225–237.
- Finn, R.S.; Ikeda, M.; Zhu, A.X.; Sung, M.W.; Baron, A.D.; Kudo, M.; Okusaka, T.; Kobayashi, M.; Kumada, H.; Kaneko, S.; et al. Phase Ib Study of Lenvatinib Plus Pembrolizumab in Patients With Unresectable Hepatocellular Carcinoma. J. Clin. Oncol. 2020, 38, 2960–2970.
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905.
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Lim, H.Y.; Kudo, M.; Breder, V.V.; Merle, P.; et al. IMbrave150: Updated overall survival (OS) data from a global, randomized, open-label phase III study of atezolizumab (atezo) + bevacizumab (bev) versus sorafenib (sor) in patients (pts) with unresectable hepatocellular carcinoma (HCC). J. Clin. Oncol. 2021, 39, 267.
- Gandhi, L.; Rodríguez-Abreu, D.; Gadgeel, S.; Esteban, E.; Felip, E.; De Angelis, F.; Domine, M.; Clingan, P.; Hochmair, M.J.; Powell, S.F.; et al. Pembrolizumab plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 378, 2078–2092.
- O’Sullivan, H.; Collins, D.; O’Reilly, S. Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. N. Engl. J. Med. 2019, 380, 986.
