Abnormal mosaicism is the coexistence of cells with at least two genotypes, by the time of birth, in an individual derived from a single zygote, which leads to a disease phenotype. Somatic mosaicism can be further categorized into segmental mosaicism and nonsegmental somatic mosaicism. Acne is a chronic illness characterized by inflammatory changes around and in the pilosebaceous units, commonly due to hormone- and inflammatory signaling-mediated factors. Several systemic disorders, such as congenital adrenal hyperplasia, polycystic ovarian syndrome, and seborrhoea-acne-hirsutism-androgenetic alopecia syndrome have classically been associated with acne. Autoinflammatory syndromes, including PAPA, PASH, PAPASH, PsAPASH, PsaPSASH, PASS, and SAPHO syndromes include acneiform lesions as a key manifestation. Mosaic germline mutations in the FGFR2 gene have been associated with Apert syndrome and nevus comedonicus, two illnesses that are accompanied by acneiform lesions.
- acne
- hormones
- syndromes
- mosaicism
- pilosebaceous unit
- hirsutism
- alopecia
1. Mosaicism
2. Acne
Acne is a chronic illness [28[13][14],29], leading to changes in sebum quantity and release of lipid fractions, altered keratinization, and resulting bacterial colonization, such as with Propionibacterium acnes (P. acnes) and Staphylococci [30,31][15][16]. It most often affects hair follicles on the face, neck, chest, and back [32,33][17][18].
Risk factors for the development of acne include a family history of severe acne, the polycystic ovary syndrome (PCOS), the metabolic syndrome, and rare genetic conditions (e.g., Apert syndrome) [38,39][19][20]. The increased risk of developing acne in the presence of a positive family history ranges from 2.30 to 4.69 [40][21]. Familial clustering was evident in a retrospective study of 1557 pairs of monozygotic and dizygotic twins living in the UK [41][22]. The severity of acne, magnitude of sebum production and inflammation, extension of the disease, regional variations, clinical course, and response to treatment are influenced by genetic factors, such as family history of acne, as well as early onset of comedonal acne [32,42][17][23].
Follicular hypercornification through direct and indirect modulation of the innate immune system has been connected with changes in sebum lipid composition [48][24]. Sebaceous glands and sebum lipids are optimal anaerobic grounds for P. acnes activation [49][25]. Lipases produced by P. acnes hydrolyze triglycerides into pro-inflammatory free fatty acids as sebum passes through the follicular duct [50,51,52][26][27][28]. The binding of TLR2 and TLR4 on sebaceous glands by P. acnes triggers sebocyte production of antimicrobial peptides (human β-defensin (hBD)1 and hBD2) and inflammatory cytokines (tumor necrosis factor (TNF)α, IL-1α and IL-8) [44,53][29][30]. Moreover, various mechanisms of insulin-like growth factor (IGF)-1 may aid the emergence of acne, such as through increased androgen stimulation and the disinhibition of the forkhead box (Fox)O1 transcription factor, leading to further activation of the androgen receptor (AR).
3. Acne Mosaicism
Since family history of acne is a risk factor that predisposes an individual to develop the condition, genetics may play a pivotal role in the pathogenesis. Several theories have been proposed with regards to genetic causes, such as decreased CAG repeats in the AR, particularly in Asian individuals [61,62[31][32][33],63], polymorphisms in genes such as those for TNFA, TNFR2, TLR2, IL1, CYP1A1, CYP17–34T/C, CYP21, and somatic mutations in FGFR2 [64,65,66,67,68,69,70,71,72][34][35][36][37][38][39][40][41][42]. Of the four known fibroblast growth factor receptors (FGFRs), i.e., FGFR1–4, the epidermis expresses FGFR1 and FGFR2. FGFR2 is the gene encoding this family of related but individually distinct tyrosine kinase receptors. This receptor is alternatively spliced into two isoforms, FGFR2b and FGFR2c [73,74][43][44]. These have exquisite ligand specificity and are expressed in either epithelial (FGFR2b) or mesenchymal cells (FGFR2c) [74,75,76][44][45][46]. FGFR2b is an essential component in embryogenesis of the skin and is expressed by the epidermis, hair follicles, and sebaceous glands [77][47]. Its continued presence is necessary for the long-term survival of sebocytes, whereas its deletion leads to sebaceous gland atrophy [42][23]. FGFR2 mosaicisms, which may be associated with epithelial dysregulation resulting in cancers of the breast, uterus, and skin, have been identified in a localized acneiform naevus in a single individual [64,78][34][48]. The germline mutations of adjacent amino acid residues of FGFR2, either S252W or P253R, cause Apert syndrome, an autosomal dominant condition characterized by severe acne and stereotypical craniofacial and limb abnormalities [64,79,80,81,82][34][49][50][51][52]. These gain-of-function mutations are localized in the linker region between D2- and D3-immunoglobulin-like regions of the FGFR2-ligand-binding domain [82][52]. The resulting mutation causes inappropriate receptor activation due to loss of ligand specificity for both the FGFR2b and FGFR2c isoforms, leading to follicular keratinocyte proliferation, sebaceous lipogenesis, and inflammatory cytokine response [82,83,84,85,86][52][53][54][55][56]. FGFR2b is exclusively expressed on epithelial cells, whereas FGFR2c is only expressed on dermal and mesenchymal cells [87][57].4. Acne-Associated Endocrine/Immunological Syndromes
Systemic endocrine/immunological disorders and syndromes such as congenital adrenal hyperplasia (CAH), PCOS, seborrhea-acne-hirsutism-androgenetic alopecia (SAHA) syndrome, primary ovarian insufficiency, and many others have classically been associated with acne [87,94][57][58] (Table 1). These conditions should raise suspicion and considered as plausible diagnoses when patients present with sudden, severe, and/or treatment-resistant acne, both in childhood and adulthood. Moreover, acne that presents with other signs of hormonal imbalance, such as hirsutism, irregular menstruation, altered libido and insulin resistance, should raise clinical suspicion of an acne-associated syndrome [87,94][57][58].| Endocrinologic Syndromes | Autoinflammatory Syndromes |
|---|
| |||||
|
|
5. Acne in Autoinflammatory Syndromes
Autoinflammatory syndromes that involve acne include pyogenic arthritis-pyoderma gangrenosum-acne (PAPA) syndrome, pyoderma gangrenosum-acne-suppurative hidradenitis (PASH) syndrome, pyogenic arthritis-pyoderma gangrenosum-acne-suppurative hidradenitis (PAPASH) syndrome, psoriatic arthritis-pyoderma gangrenosum-acne-suppurative hidradenitis (PsAPASH) syndrome, pustular psoriasis-arthritis-pyoderma gangrenosum-synovitis-acne-suppurative hidradenitis (PsAPSASH) syndrome, pyoderma gangrenosum-acne-suppurative hidradenitis-ankylosing spondylitis (PASS) syndrome, and synovitis-acne-pustulosis-hyperostosis-osteitis (SAPHO) syndrome [87,109][57][59] (Table 1). The type of acne associated with autoinflammatory syndromes is usually a severe nodulocystic type, clinically presenting with large, inflamed nodules and cysts affecting the face, back, and chest [110][60]. The IL-1β pathway has been associated with many of the autoinflammatory disorder mutations [111][61]. The dysregulation of inflammasome function and the release of proinflammatory cytokines, such as TNFα and IFN-γ, and chemokines, particularly IL-8 and RANTES (regulated on activation, normal T cell expressed and secreted), which are responsible for the recruitment and activation of neutrophils that lead to neutrophil-mediated inflammation, is usually related to the over-expression of IL-1β [112,113][62][63]. Proinflammatory cytokines also induce the production of metalloproteinases (MMPs), notably MMP-2 and MMP-9, leading to tissue destruction by degrading the components of the extracellular matrix [114][64]. MMPs of epithelial origin have also been detected in facial sebum of patients with acne and they are regulated by isotretinoin treatment [115][65].6. Acneiform Eruptions
The manifestation of acne/acneiform lesions in numerous diseases/syndromes of varying etiology highlights the multifaceted nature of acne [28,29,87,94,102,124][13][14][57][58][66][67]. Since not all eruptions that resemble acne also represent acne vulgaris, awareness of diseases is essential, which can neither be classified under acne nor are part of a systemic disease or syndrome [7. Conclusions
Acne represents a cardinal skin manifestation in several groups of diseases. It is present in endocrine/immunological syndromes, autoinflammatory syndromes, and certain mosaicisms, indicating that it is an intriguing model for studying the interactions among hormones, innate immunity, inflammation, wound healing (scarring), and gene mutations (Figure 81). Exploring possible common mechanisms of acne induction in various acne-associated diseases and syndromes—including mosaicisms—might contribute to the development of novel therapeutic regimens.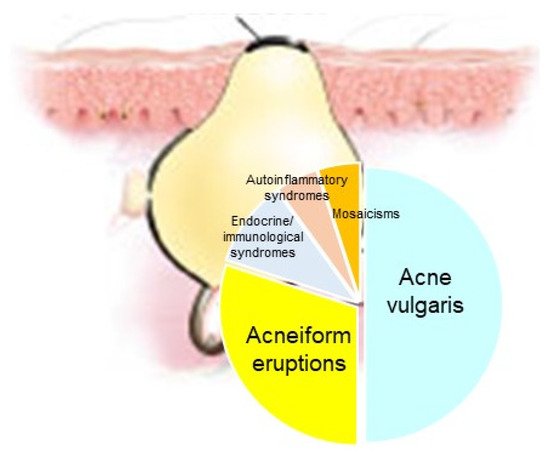
References
- Happle, R. Mosaicism as a Biological Concept. In Mosaicism in Human Skin; Springer: Berlin/Heidelberg, Germany, 2014; pp. 5–12.
- Rahbari, R.; Wuster, A.; Lindsay, S.J.; Hardwick, R.J.; Alexandrov, L.B.; Al Turki, S.; Dominiczak, A.; Morris, A.; Porteous, D.; Smith, B.; et al. Timing, rates and spectra of human germline mutation. Nat. Genet. 2015, 48, 126–133.
- Kinsler, V.A. An Introduction to Mosaicism. In Harper’s Textbook of Pediatric Dermatology, 4th ed.; Hoeger, P., Kinsler, V., Yan, A., Harper, J., Oranje, A., Bodemer, C., Larralde, M., Luk, D., Mendiratta, V., Purvis, D., Eds.; Wiley: Hoboken, NJ, USA, 2019; pp. 1229–1236.
- Happle, R. Dohi Memorisl Lecture. New aspects of cutaneous mosaicism. J. Dermatol. 2002, 29, 681–692.
- Happle, R. Mosaicism in human skin. Understanding the patterns and mechanisms. Arch. Dermatol. 1993, 129, 1460–1470.
- Keppler-Noreuil, K.M.; Sapp, J.C.; Lindhurst, M.J.; Parker, V.E.; Blumhorst, C.; Darling, T.; Tosi, L.L.; Huson, S.M.; Whitehouse, R.W.; Jakkula, E.; et al. Clinical delineation and natural history of the PIK3CA -related overgrowth spectrum. Am. J. Med. Genet. Part A 2014, 164, 1713–1733.
- Thomas, A.C.; Zeng, Z.; Rivière, J.-B.; O’Shaughnessy, R.; Al-Olabi, L.; St.-Onge, J.; Atherton, D.J.; Aubert, H.; Bagazgoitia, L.; Barbarot, S.; et al. Mosaic activating mutations in GNA11 and GNAQ are associated with phakomatosis pigmentovascularis and extensive dermal melanocytosis. J. Investig. Dermatol. 2016, 136, 770–778.
- Kinsler, V.; Boccara, O.; Fraitag, S.; Torrelo, A.; Vabres, P.; Diociaiuti, A. Mosaic abnormalities of the skin: Review and guidelines from the European Reference Network for rare skin diseases. Br. J. Dermatol. 2019, 182, 552–563.
- Kinsler, V.A.; Abu-Amero, S.; Budd, P.; Jackson, I.; Ring, S.M.; Northstone, K.; Atherton, D.J.; Bulstrode, N.; Stanier, P.; Hennekam, R.C.; et al. Germline melanocortin-1-receptor genotype is associated with severity of cutaneous phenotype in congenital melanocytic nevi: A role for MC1R in human fetal development. J. Investig. Dermatol. 2012, 132, 2026–2032.
- Lindhurst, M.J.; Sapp, J.; Teer, J.K.; Johnston, J.J.; Finn, E.M.; Peters, K.; Turner, J.; Cannons, J.L.; Bick, D.; Blakemore, L.; et al. A mosaic activating mutation in AKT1 associated with the Proteus syndrome. N. Engl. J. Med. 2011, 365, 611–619.
- Kinsler, V.A.; Krengel, S.; Riviere, J.-B.; Waelchli, R.; Chapusot, C.; Al-Olabi, L.; Faivre, L.; Haenssle, H.A.; Weibel, L.; Jeudy, G.; et al. Next-generation sequencing of nevus spilus–type congenital melanocytic nevus: Exquisite genotype–phenotype correlation in mosaic RASopathies. J. Investig. Dermatol. 2014, 134, 2658–2660.
- Groesser, L.; Herschberger, E.; Ruetten, A.; Ruivenkamp, C.; Lopriore, E.; Zutt, M.; Langmann, T.; Singer, S.; Klingseisen, L.; Schneider-Brachert, W.; et al. Postzygotic HRAS and KRAS mutations cause nevus sebaceous and Schimmelpenning syndrome. Nat. Genet. 2012, 44, 783–787.
- Zouboulis, C.C. Acne as a chronic systemic disease. Clin. Dermatol. 2013, 32, 389–396.
- Gollnick, H.P.; Zouboulis, C.C. Not all acne is acne vulgaris. Dtsch. Aerzteblatt Online 2014, 111, 301–312.
- Zouboulis, C.C. Endocrinology and immunology of acne: Two sides of the same coin. Exp. Dermatol. 2020, 29, 840–859.
- Lovászi, M.; Szegedi, A.; Zouboulis, C.C.; Törőcsik, D. Sebaceous-immunobiology is orchestrated by sebum lipids. Dermatoendocrinol. 2017, 9, e1375636.
- Williams, H.C.; Dellavalle, R.; Garner, S. Acne vulgaris. Lancet 2011, 379, 361–372.
- Tuchayi, S.M.; Makrantonaki, E.; Ganceviciene, R.; Dessinioti, C.; Feldman, S.R.; Zouboulis, C.C. Acne vulgaris. Nat. Rev. Dis. Prim. 2015, 1, 1–20.
- Ghodsi, S.Z.; Orawa, H.; Zouboulis, C.C. Prevalence, severity, and severity risk factors of acne in high school pupils: A community-based study. J. Investig. Dermatol. 2009, 129, 2136–2141.
- Zaenglein, A.L. Acne vulgaris. N. Engl. J. Med. 2018, 379, 1343–1352.
- Karciauskiene, J.; Valiukeviciene, S.; Gollnick, H.; Stang, A. The prevalence and risk factors of adolescent acne among schoolchildren in Lithuania: A cross-sectional study. J. Eur. Acad. Dermatol. Venereol. 2013, 28, 733–740.
- Bataille, V.; Snieder, H.; MacGregor, A.; Sasieni, P.; Spector, T. The influence of genetics and environmental factors in the pathogenesis of acne: A twin study of acne in women. J. Investig. Dermatol. 2002, 119, 1317–1322.
- Plewig, G.; Melnik, B.; Chen, W. Acne Epidemiology and Genetics. In Plewig and Kligman’s Acne and Rosacea; Springer: Cham, Switzerland, 2019; pp. 35–44.
- Zouboulis, C.C.; Jourdan, E.; Picardo, M. Acne is an inflammatory disease and alterations of sebum composition initiate acne lesions. J. Eur. Acad. Dermatol. Venereol. 2013, 28, 527–532.
- Ottaviani, M.; Camera, E.; Picardo, M. Lipid mediators in acne. Mediat. Inflamm. 2010, 2010, 1–6.
- Elias, P.M. The skin barrier as an innate immune element. Semin. Immunopathol. 2007, 29, 3–14.
- Elias, P.M. Stratum corneum defensive functions: An integrated view. J. Investig. Dermatol. 2005, 125, 183–200.
- Fluhr, J.W.; Kao, J.; Ahn, S.K.; Feingold, K.R.; Elias, P.M.; Jain, M. Generation of free fatty acids from phospholipids regulates stratum corneum acidification and integrity. J. Investig. Dermatol. 2001, 117, 44–51.
- Kim, J.; Ochoa, M.-T.; Krutzik, S.R.; Takeuchi, O.; Uematsu, S.; Legaspi, A.J.; Brightbill, H.D.; Holland, D.; Cunliffe, W.J.; Akira, S.; et al. Activation of Toll-like receptor 2 in acne triggers inflammatory cytokine responses. J. Immunol. 2002, 169, 1535–1541.
- Nagy, I.; Pivarcsi, A.; Koreck, A.; Széll, M.; Urbán, E.; Kemény, L. Distinct strains of Propionibacterium acnes induce selective human β-defensin-2 and interleukin-8 expression in human keratinocytes through Toll-like receptors. J. Investig. Dermatol. 2005, 124, 931–938.
- Sawaya, M.E.; Shalita, A.R. Androgen receptor polymorphisms (CAG repeat lengths) in androgenetic alopecia, hirsutism, and acne. J. Cutan. Med. Surg. 1998, 3, 9–15.
- Pang, Y.; He, C.; Liu, Y.; Wang, K.; Xiao, T.; Wang, Y.; Zhu, H.; Wei, B.; Zhao, N.; Jiang, Y.; et al. Combination of short CAG and GGN repeats in theandrogen receptorgene is associated with acne risk in North East China. J. Eur. Acad. Dermatol. Venereol. 2008, 22, 1445–1451.
- Yang, Z.; Yu, H.; Cheng, B.; Tang, W.; Dong, Y.; Xiao, C.; He, L. Relationship between the CAG repeat polymorphism in the androgen receptor gene and acne in the Han ethnic group. Dermatology 2009, 218, 302–306.
- Munro, C.S.; Wilkie, A. Epidermal mosaicism producing localised acne: Somatic mutation in FGFR2. Lancet 1998, 352, 704–705.
- Ostlere, L.S.; Rumsby, G.; Holownia, P.; Jacobs, H.S.; Rustin, M.H.A.; Honour, J.W. Carrier status for steroid 21-hydroxylase deficiency is only one factor in the variable phenotype of acne. Clin. Endocrinol. 1998, 48, 209–215.
- He, L.; Yang, Z.; Yu, H.; Cheng, B.; Tang, W.; Dong, Y.; Xiao, C. The Relationship between CYP17 –34T/C polymorphism and acne in Chinese subjects revealed by sequencing. Dermatology 2006, 212, 338–342.
- Paraskevaidis, A.; Drakoulis, N.; Roots, I.; Orfanos, C.; Zouboulis, C.C. Polymorphisms in the human cytochrome P-450 1A1 gene (CYP1A1) as a factor for developing acne. Dermatology 1998, 196, 171–175.
- Herane, M.I.; Ando, I. Acne in infancy and acne genetics. Dermatology 2003, 206, 24–28.
- Szabo, K.; Tax, G.; Kis, K.; Szegedi, K.D.; Diószegi, C.; Koreck, A.; Teodorescu-Brinzeu, D.G.; Széll, M.; Kemény, L. Interleukin-1A +4845(G> T) polymorphism is a factor predisposing to acne vulgaris. Tissue Antigens 2010, 76, 411–415.
- Tian, L.-M.; Xie, H.-F.; Yang, T.; Hu, Y.-H.; Li, J.; Wang, W.-Z. Association study of tumor necrosis factor receptor type 2 M196R and Toll-like receptor 2 Arg753Gln polymorphisms with acne vulgaris in a Chinese Han ethnic group. Dermatology 2010, 221, 276–284.
- Karaca, N.; Ozturk, G.; Gerceker, B.; Turkmen, M.; Berdeli, A. TLR2 and TLR4 gene polymorphisms in Turkish vitiligo patients. J. Eur. Acad. Dermatol. Venereol. 2012, 27, e85–e90.
- Szabó, K.; Tax, G.; Teodorescu-Brinzeu, D.; Koreck, A.; Kemény, L. TNFα gene polymorphisms in the pathogenesis of acne vulgaris. Arch. Dermatol. Res. 2010, 303, 19–27.
- Bonano, V.I.; Oltean, S.; Brazas, R.M.; Garcia-Blanco, M.A. Imaging the alternative silencing of FGFR2 exon IIIb in vivo. RNA 2006, 12, 2073–2079.
- Oldridge, M.; Zackai, E.H.; McDonald-McGinn, D.M.; Iseki, S.; Morriss-Kay, G.M.; Twigg, S.; Johnson, D.; Wall, S.A.; Jiang, W.; Theda, C.; et al. De novo Alu-element insertions in FGFR2 identify a distinct pathological basis for Apert syndrome. Am. J. Hum. Genet. 1999, 64, 446–461.
- Housley, R.M.; Morris, C.F.; Boyle, W.; Ring, B.; Biltz, R.; E Tarpley, J.; Aukerman, S.L.; Devine, P.L.; Whitehead, R.H.; Pierce, G.F. Keratinocyte growth factor induces proliferation of hepatocytes and epithelial cells throughout the rat gastrointestinal tract. J. Clin. Investig. 1994, 94, 1764–1777.
- Orr-Urtreger, A.; Bedford, M.T.; Burakova, T.; Arman, E.; Zimmer, Y.; Yayon, A.; Givol, D.; Lonai, P. Developmental localization of the splicing alternatives of fibroblast growth factor receptor-2 (FGFR2). Dev. Biol. 1993, 158, 475–486.
- Danilenko, D.M.; Ring, B.D.; Yanagihara, D.; Benson, W.; Wiemann, B.; Starnes, C.O.; Pierce, G.F. Keratinocyte growth factor is an important endogenous mediator of hair follicle growth, development, and differentiation: Normalization of the nu/nu follicular differentiation defect amelioration of chemotherapy-induced alopecia. Am. J. Pathol. 1995, 147, 145–154.
- Katoh, M. FGFR2 abnormalities underlie a spectrum of bone, skin, and cancer pathologies. J. Investig. Dermatol. 2009, 129, 1861–1867.
- Solomon, L.M.; Fretzin, D.; Pruzansky, S. Pilosebaceous abnormalities in Apert’s syndrome. Arch. Dermatol. 1970, 102, 381–385.
- Atherton, D.J.; Rebello, T.; Wells, R.S. Apert’s Syndrome with severe acne vulgaris. Proc. R. Soc. Med. 1976, 69, 517–518.
- Higgins, R.; Pink, A.; Hunger, R.; Yawalkar, N.; Navarini, A.A. Generalized comedones, acne, and hidradenitis suppurativa in a patient with an FGFR2 missense mutation. Front. Med. 2017, 4, 16.
- Wilkie, A.; Slaney, S.F.; Oldridge, M.; Poole, M.D.; Ashworth, G.J.; Hockley, A.D.; Hayward, R.D.; David, D.J.; Pulleyn, L.J.; Rutland, P.; et al. Apert syndrome results from localized mutations of FGFR2 and is allelic with Crouzon syndrome. Nat. Genet. 1995, 9, 165–172.
- Goriely, A.; McVean, G.A.T.; Röjmyr, M.; Ingemarsson, B.; Wilkie, A.O.M. Evidence for selective advantage of pathogenic FGFR2 mutations in the male germ line. Science 2003, 301, 643–646.
- Ibrahimi, O.A.; Zhang, F.; Eliseenkova, A.V.; Itoh, N.; Linhardt, R.J.; Mohammadi, M. Biochemical analysis of pathogenic ligand-dependent FGFR2 mutations suggests distinct pathophysiological mechanisms for craniofacial and limb abnormalities. Hum. Mol. Genet. 2004, 13, 2313–2324.
- Moloney, D.M.; Slaney, S.R.; Oldridge, M.; Wall, S.A.; Sahlin, P.; Stenman, G.; Wilkie, A.O. Exclusive paternal origin of new mutations in Apert syndrome. Nat. Genet. 1996, 13, 48–53.
- Yu, K.; Herr, A.; Waksman, G.; Ornitz, D.M. Loss of fibroblast growth factor receptor 2 ligand-binding specificity in Apert syndrome. Proc. Natl. Acad. Sci. USA 2000, 97, 14536–14541.
- Chen, W.; Obermayer-Pietsch, B.; Hong, J.-B.; Melnik, B.C.; Yamasaki, O.; Dessinioti, C.; Ju, Q.; I Liakou, A.; Al-Khuzaei, S.; Katsambas, A.; et al. Acne-associated syndromes: Models for better understanding of acne pathogenesis. J. Eur. Acad. Dermatol. Venereol. 2010, 25, 637–646.
- Zouboulis, C.C.; Picardo, M.; Ju, Q.; Kurokawa, I.; Törőcsik, D.; Bíró, T.; Schneider, M.R. Beyond acne: Current aspects of sebaceous gland biology and function. Rev. Endocr. Metab. Disord. 2016, 17, 319–334.
- Nikolakis, G.; Kaleta, K.P.; Vaiopoulos, A.G.; Wolter, K.; Baroud, S.; Wojas-Pelc, A.; Zouboulis, C.C. Phenotypes and pathophysiology of syndromic hidradenitis suppurativa: Different faces of the same disease? A systematic review. Dermatology 2020, 237, 673–697.
- Marzano, A.V.; Ishak, R.S.; Colombo, A.; Caroli, F.; Crosti, C. Pyoderma Gangrenosum, Acne and suppurative hidradenitis syndrome following bowel bypass surgery. Dermatology 2012, 225, 215–219.
- Dinarello, C.A. Interleukin-1 in the pathogenesis and treatment of inflammatory diseases. Blood 2011, 117, 3720–3732.
- Dinarello, C.A. A clinical perspective of IL-1β as the gatekeeper of inflammation. Eur. J. Immunol. 2011, 41, 1203–1217.
- Marzano, A.V.; Cugno, M.; Trevisan, V.; Fanoni, D.; Venegoni, L.; Berti, E.; Crosti, C. Role of inflammatory cells, cytokines and matrix metalloproteinases in neutrophil-mediated skin diseases. Clin. Exp. Immunol. 2010, 162, 100–107.
- Marzano, A.V.; Fanoni, D.; Antiga, E.; Quaglino, P.; Caproni, M.; Crosti, C.; Meroni, P.L.; Cugno, M. Expression of cytokines, chemokines and other effector molecules in two prototypic autoinflammatory skin diseases, pyoderma gangrenosum and Sweet’s syndrome. Clin. Exp. Immunol. 2014, 178, 48–56.
- Papakonstantinou, E.; Aletras, A.J.; Glass, E.; Tsogas, P.; Dionyssopoulos, A.; Adjaye, J.; Fimmel, S.; Gouvousis, P.; Herwig, R.; Lehrach, H.; et al. Matrix metalloproteinases of epithelial origin in facial sebum of patients with acne and their regulation by isotretinoin. J. Investig. Dermatol. 2005, 125, 673–684.
- Zouboulis, C.C. Acne and sebaceous gland function. Clin. Dermatol. 2004, 22, 360–366.
- Kurokawa, I.; Danby, F.W.; Ju, Q.; Wang, X.; Xiang, L.F.; Xia, L.; Chen, W.; Nagy, I.; Picardo, M.; Suh, D.H.; et al. New developments in our understanding of acne pathogenesis and treatment. Exp. Dermatol. 2009, 18, 821–832.
- Plewig, G.; Jansen, T. Acneiform dermatoses. Dermatology 1998, 196, 102–107.
- Zeichner, J.A. Acneiform Eruptions in Dermatology; Springer: Berlin/Heidelberg, Germany, 2014.
- Dessinioti, C.; Antoniou, C.; Katsambas, A. Acneiform eruptions. Clin. Dermatol. 2014, 32, 24–34.
