Collagen is a good treatment candidate for OA among the different therapeutic options due to its safety and clinical evidence. Two different approaches for collagen include collagen hydrolysates and native collagen and both types of collagen nutraceuticals are effective in reducing OA pain, in animal models and human clinical trials. Native collagen, which may be poorly absorbed, could work through a mechanism of oral induction, and hydrolyzed collagen can reach the target site where collagen synthesis is needed.
- clinical studies
- collagen
- scaffold
- tissue engineering
- treatment
1. Introduction
Collagen, an important protein produced by the body, is the main structural protein found in the skin, tendon, and bone. The word collagen originates from a Greek word that “kola” means gum and “gen” means producing. Collagen is considered to be one of the most useful biomaterials. Due to its low immunogenicity and high biocompatibility, it has been extensively studied as a polymer for use in many biomedical goods such as cosmetic and pharmaceutical products [1,2][1][2]. It also has been used as a safe and effective biomaterial in tissue engineering and clinical applications. It is an ingredient in dental composites, skin regeneration templates, and biodegradable matrices, and it has been used in cardiovascular surgery, plastic surgery, orthopedics, urology, neurology, and ophthalmology. There is a large demand for collagen in the food industry because it has high protein content and good functional properties such as water absorption capacity and the ability to form emulsions [3,4][3][4].
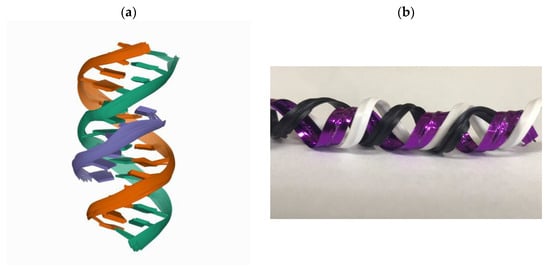
Collagen is one of the most abundant proteins in many living organisms because it plays a connective role in biological structures. It is also the most abundant protein in the extracellular matrix (ECM). ECM is a non-cellular component within all tissues and organs and is a structural scaffold that can direct cell adhesion and migration, and regulate cellular growth and metabolism [5]. In addition to blood cells, other cells in human tissues are residing in ECM. Collagen fibrils form the main tension-resisting element of a complicated fiber-composite system in the ECM [6]. There are four structural levels of a collagen protein including primary structure (amino acid triplet), secondary structure (the α-helix), tertiary structure (triple helix), and quaternary structure (fibrils) [7]. It is formed in a triplex helix by three α chains ( Figure 1 ). The chains are distorted around each other to form a tight and stable structure [8].
According to the α-chain composition, there are different types of collagens. About 28 types of collagen have been identified, but the dominant collagen is collagen type I. Over 90% of the collagen in the human body is collagen type I because of its wide prevalence in almost all connective tissues [9]. There are 5 most common types of collagen, type I–V [10,11][10][11]. Table 1 lists some functions of these five types of collagen. Collagen type I is the main component of the calcified tissue of teeth and bone and is present in skin, tendons, vasculature, lungs, and heart. It can be a ligand for receptor-mediated signalings such as integrins, OSCAR, GPVI, G6b-B, DDR1 and 2, and LAIR-1 of the leukocyte receptor complex [12]. Collagen type II is an abundant matrix molecule of cartilage and is associated with many diseases such as skeletal dysplasias, rheumatoid arthritis (RA) and osteoarthritis (OA) [13,14,15][13][14][15].
| Collagen | Function or Application | Tissue or Organ | Molecular Composition * |
|---|---|---|---|
| Type I | the organic part of the bone, membranes for guided tissue regeneration | Skin, bone, teeth, tendon, ligament, vascular ligature | [α1(I)]2α2(I) |
| Type II | the main constituent of cartilage, cartilage repair, and arthritis treatment | cartilage | [α1(II)]3 |
| Type III | the main constituent of reticular fibers, hemostats, and tissue sealants | muscle, blood vessels | [α1(III)]3 |
| Type IV | the major component of the basement membrane, attachment enhancer of cell culture, and diabetic nephropathy indicator | basal lamina, the epithelium-secreted layer of the basement membrane | [α1(IV)]2α2(IV) [α3(IV)]2α4(IV) [α5(IV)]2α6(IV) |
| Type V | feedstock for biomaterials in corneal treatments | Hair, cell surfaces, and placenta. | α1(V),α2(V),α3(V) |
Collagen type III, consisting of only one collagen α chain, belongs to the fibrillar collagen group. It is a homotrimer composed of three identical α1(III) chains supercoiled around each other in a right-handed triple helix. It also is an important component of blood vessels and muscle. It appears to function along with type I collagen in the skin, ligament, tendon, periodontal ligament, vascular walls, and synovial membranes [16]. Collagen type III is related to vascular deficiency, aortic and arterial aneurysms, and Ehlers Danlos syndrome (EDS) [17]. EDS comprises ten types. EDS IV is the most severe type that is caused by mutations in a collagen type III corresponding gene COL3A1 [18]. Collagen type IV is the predominant collagen of the basement membrane forming the backbone of the basement membrane. Mutations in collagen type IV can cause chronic kidney disease, Alport’s syndrome [19]. Collagen type V is present in the corneal stroma, bone matrix, and the interstitial matrix of muscles, lungs, liver, and placenta [20]. Collagen type V functioned along with collagen type I in skin and tendon, and mutations in collagen type V had been shown to underlie classical EDS [21].
2. Effects of Treatment
Asserin et al. investigated the efficacy of oral collagen peptide supplementation on skin hydration in a clinical study [49][22]. After several weeks of intake, the oral collagen peptide supplementation remarkably increased skin hydration, the collagen density in the dermis remarkably increased and the fragmentation of the dermal collagen network remarkably decreased. These effects persevered after 12 weeks. The results suggested that oral collagen peptide supplementation significantly improved skin aging.
Tanaka et al. examined the effect of daily intake of collagen peptides on the skin damage caused by repeated UV-B irradiation [54][23]. Intake of collagen peptide suppressed UV-B-induced skin hyperplasia of the epidermis, hydration decreases, and soluble type I collagen decreases. These results suggested that collagen peptides could suppress UV-B-induced skin damage.
A major challenge in clinical orthopedics is the regeneration of large segmental bone defects. The collagen scaffolds have been increasingly used as bone substitutes through tissue engineering approaches [60][24]. Preparation of collagen catecholamines and calcium composite structures was reported and the collagen composite scaffolds displayed outstanding mechanical properties [61][25]. These multifunctional scaffolds could be utilized to regenerate and repair bone defects. Nevertheless, the low mechanical strength of collagen limited its wider application in the field of bone regeneration. By combining different biological materials, the porosity, structural stability, osteoinduction and osteogenic properties of the collagen matrix can be greatly improved [40][26]. For example, a collagen scaffold loaded with human umbilical cord-derived mesenchymal stem cells was fabricated and applied for endometrium regeneration [62][27].
Collagen oral administration could be also an efficient treatment for wound healing. A study investigated the effect of oral administration of the collagen peptides derived from jellyfish in wound healing [82][28]. It was shown that collagen peptides from Jellyfish-Rhopilema esculentum might be beneficial to wound clinics in the future due to their good characteristic in accelerating the wound healing process. The wound healing potential of oral administering collagen peptides from chum salmon skin in wound rat models was investigated [83][29]. Oral administration of marine collagen peptides derived from chum salmon improves wound healing in rats [84][30]. The result showed the efficacy of oral administering collagen peptides treatment on wound healing in animals. The oral application of specific bioactive collagen peptides has also demonstrated positive effects on wound healing. A study showed that would patients treated with bioactive collagen peptides had a better outcome compared with the placebo groups [85][31]. A collagen-derived peptide, prolyl-hydroxyproline (Pro-Hyp), was a growth-initiating factor for specific fibroblasts involved in the wound healing process [86][32].
3. Conclusions
Collagen is the most abundant protein in the human body that has many multi-functions. The loss or defect of collagen can cause skin aging and other diseases. The collage treatments have demonstrated effective improvements in skin hydration, skin elasticity, medical scaffold treatment, GERD, OA and RA in many clinical studies. In addition, the collagen treatment for GERD in COVID-19 patients is also discussed in this study. Collagen therapy can reach good improvement and does not cause any serious adverse reactions. Collagen-based materials and products are the potential to be used in more applications, and they are the one of most important supplements for aging people.
References
- Meena, C.; Mengi, S.A.; Deshpande, S.G. Biomedical and industrial applications of collagen. Proc. Indian Acad. Sci. Chem. Sci. 1999, 111, 319–329.
- Sionkowska, A.; Adamiak, K.; Musiał, K.; Gadomska, M. Collagen Based Materials in Cosmetic Applications: A Review. Materials 2020, 13, 2417.
- Lafarga, T.; Hayes, M. Bioactive peptides from meat muscle and by-products: Generation, functionality and application as functional ingredients. Meat Sci. 2014, 98, 227–239.
- Schmidt, M.M.; Dornelles, R.C.P.; Mello, R.O.; Kubota, E.H.; Mazutti, M.A.; Kempka, A.P.; Demiate, I.M. Collagen extraction process. Int. Food Res. J. 2016, 23, 913–922.
- Theocharis, A.D.; Skandalis, S.S.; Gialeli, C.; Karamanos, N.K. Extracellular matrix structure. Adv. Drug Deliv. Rev. 2016, 97, 4–27.
- Holmes, D.F.; Lu, Y.; Starborg, T.; Kadler, K.E. Collagen fibril assembly and function. Curr. Top. Dev. Biol. 2018, 130, 107–142.
- Gelse, K.; Poschl, E.; Aigner, T. Collagens--Structure, function, and biosynthesis. Adv. Drug Deliv. Rev. 2003, 55, 1531–1546.
- Leon-Lopez, A.; Morales-Penaloza, A.; Martinez-Juarez, V.M.; Vargas-Torres, A.; Zeugolis, D.I.; Aguirre-Alvarez, G. Hydrolyzed Collagen-Sources and Applications. Molecules 2019, 24, 4031.
- Cheah, K.S. Collagen genes and inherited connective tissue disease. Biochem. J. 1985, 229, 287–303.
- Silvipriya, K.; Kumar, K.K.; Bhat, A.; Kumar, B.D.; John, A.; Lakshmanan, P. Collagen: Animal sources and biomedical application. J. Appl. Pharm. Sci. 2015, 5, 123–127.
- Rodriguez, M.I.A.; Barroso, L.G.R.; Sanchez, M.L. Collagen: A review on its sources and potential cosmetic applications. J. Cosmet. Dermatol. 2018, 17, 20–26.
- Boraschi-Diaz, I.; Wang, J.; Mort, J.S.; Komarova, S.V. Collagen Type I as a Ligand for Receptor-Mediated Signaling. Front. Phys. 2017, 5, 12.
- Winterpacht, A.; Hilbert, M.; Schwarze, U.; Mundlos, S.; Spranger, J.; Zabel, B.U. Kniest and Stickler dysplasia phenotypes caused by collagen type II gene (COL2A1) defect. Nat. Genet. 1993, 3, 323–326.
- Juan, L.; Xiao, Z.; Song, Y.; Zhijian, Z.; Jing, J.; Kun, Y.; Yuna, H.; Dongfa, D.; Lili, D.; Liuxin, T.; et al. Safety and immunogenicity of a novel therapeutic DNA vaccine encoding chicken type II collagen for rheumatoid arthritis in normal rats. Hum. Vaccines Immunother. 2015, 11, 2777–2783.
- De Almagro, M.C. The Use of Collagen Hydrolysates and Native Collagen in Osteoarthritis. Am. J. Biomed. Sci. Res. 2020, 6, 530–532.
- Wu, J.J.; Weis, M.A.; Kim, L.S.; Eyre, D.R. Type III collagen, a fibril network modifier in articular cartilage. J. Biol. Chem. 2010, 285, 18537–18544.
- Gudmann, N.; Karsdal, M. Biochemistry of Collagens, Laminins and Elastin; Academic Press: Cambridge, MA, USA, 2016.
- Hamel, B.C.; Pals, G.; Engels, C.H.; van den Akker, E.; Boers, G.H.; van Dongen, P.W.; Steijlen, P.M. Ehlers-Danlos syndrome and type III collagen abnormalities: A variable clinical spectrum. Clin. Genet. 1998, 53, 440–446.
- Sand, J.; Genovese, F.; Karsdal, M. Type IV collagen. In Biochemistry of Collagens, Laminins and Elastin; Elsevier: Amsterdam, The Netherlands, 2016; pp. 31–41.
- Karsdal, M. Biochemistry of Collagens, Laminins and Elastin: Structure, Function and Biomarkers; Academic Press: Cambridge, MA, USA, 2019.
- Nuytinck, L.; Freund, M.; Lagae, L.; Pierard, G.E.; Hermanns-Le, T.; De Paepe, A. Classical Ehlers-Danlos syndrome caused by a mutation in type I collagen. Am. J. Hum. Genet. 2000, 66, 1398–1402.
- Asserin, J.; Lati, E.; Shioya, T.; Prawitt, J. The effect of oral collagen peptide supplementation on skin moisture and the dermal collagen network: Evidence from an ex vivo model and randomized, placebo-controlled clinical trials. J. Cosmet. Dermatol. 2015, 14, 291–301.
- Tanaka, M.; Koyama, Y.; Nomura, Y. Effects of collagen peptide ingestion on UV-B-induced skin damage. Biosci. Biotechnol. Biochem. 2009, 73, 930–932.
- Li, Z.; Du, T.; Ruan, C.; Niu, X. Bioinspired mineralized collagen scaffolds for bone tissue engineering. Bioact. Mater. 2021, 6, 1491–1511.
- Dhand, C.; Ong, S.T.; Dwivedi, N.; Diaz, S.M.; Venugopal, J.R.; Navaneethan, B.; Fazil, M.H.; Liu, S.; Seitz, V.; Wintermantel, E.; et al. Bio-inspired in situ crosslinking and mineralization of electrospun collagen scaffolds for bone tissue engineering. Biomaterials 2016, 104, 323–338.
- Zhang, D.; Wu, X.; Chen, J.; Lin, K. The development of collagen based composite scaffolds for bone regeneration. Bioact. Mater. 2018, 3, 129–138.
- Xin, L.; Lin, X.; Pan, Y.; Zheng, X.; Shi, L.; Zhang, Y.; Ma, L.; Gao, C.; Zhang, S. A collagen scaffold loaded with human umbilical cord-derived mesenchymal stem cells facilitates endometrial regeneration and restores fertility. Acta Biomater. 2019, 92, 160–171.
- Felician, F.F.; Yu, R.H.; Li, M.Z.; Li, C.J.; Chen, H.Q.; Jiang, Y.; Tang, T.; Qi, W.Y.; Xu, H.M. The wound healing potential of collagen peptides derived from the jellyfish Rhopilema esculentum. Chin. J. Traumatol. 2019, 22, 12–20.
- Zhang, Z.; Wang, J.; Ding, Y.; Dai, X.; Li, Y. Oral administration of marine collagen peptides from Chum Salmon skin enhances cutaneous wound healing and angiogenesis in rats. J. Sci. Food Agric. 2011, 91, 2173–2179.
- Wang, J.; Xu, M.; Liang, R.; Zhao, M.; Zhang, Z.; Li, Y. Oral administration of marine collagen peptides prepared from chum salmon (Oncorhynchus keta) improves wound healing following cesarean section in rats. Food Nutr. Res. 2015, 59, 26411.
- Knefeli, H.-C.J. Improved bone healing after oral application of specific bioactive collagen peptides. Int. J. Nutraceuticals Funct. Foods Nov. Foods 2018, 17, 185–188.
- Sato, K.; Asai, T.T.; Jimi, S. Collagen-Derived Di-Peptide, Prolylhydroxyproline (Pro-Hyp): A New Low Molecular Weight Growth-Initiating Factor for Specific Fibroblasts Associated With Wound Healing. Front. Cell Dev. Biol. 2020, 8, 548975.
