Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Paolo Cotogni and Version 2 by Bruce Ren.
Home parenteral nutrition (HPN) refers to the administration of nutritional support through a central venous access device (CVAD) at home
- oncology
- nutritional status
- nutritional support
- artificial nutrition
- home care
- guidelines
- clinical practice
1. Administration of HPN
PN can be total (TPN) when patients have no or negligible oral/enteral nutrition (<200 kcal/day) [1][22] or supplemental (SPN) when PN is added to oral/enteral nutrition to achieve protein and energy requirements [2][23].
Generally, SPN at home provides 1000–1250 kcal/day from three to six times per week in patients with residual—but insufficient—oral food intake. In comparison with TPN, SPN has a low risk of both overfeeding and refeeding syndrome (RS), as well as hyperglycemia, overhydration, and liver dysfunction.
Specifically, RS is defined as the potentially fatal shifts in fluids and electrolytes that may occur in severely malnourished patients at the start of artificial nutrition (either EN or PN). The risk of onset of RS increases with the degree of the patient’s malnutrition. Guidelines recommend, if oral food intake has been severely decreased for a long period, to increase nutrition slowly over several days to prevent RS [3][6].
SPN also offers benefits on the quality of life (QoL) because it reduces the number of nights potentially at risk of sleep disturbance. Finally, reducing the number of infusion days SPN lowers manipulation of the CVAD and therefore the risk of catheter-related complications. In recent studies, SPN was the preferred approach of provision of PN in oncology outpatients [4][5][24,25].
2. Why Is Monitoring Important?
The development and implementation of healthcare actions that are viable, affordable, and successful in the hospital setting is a challenge [6][26]. Nowadays, no strong recommendations are available to suggest the use of definite indicators or the timing of tools used to monitor the response to HPN in cancer patients [7][8]. Moreover, the monitoring process may be less easy to perform in outpatients than inpatients and this issue is to be faced in the set-up of the home nutritional service [3][6].
The HPN monitoring process aims at determining the appropriateness of nutritional therapy, ensuring the achievement of nutritional goals, and reducing the risk of complications [7][8]. Additionally, a consistent close monitoring for HPN-related complications is able in reducing unplanned hospital admissions and overall associated costs [8][20].
In 2011, a board of experts in the management of adult cancer patients on HPN developed a list of interventions related to quality of care. These experts indicated relevant differences in care practices regarding cancer patients compared with benign patients [9]. Specifically, the experts considered monitoring of liver function tests, vitamins, trace elements or metabolic bone diseases not essential in oncology patients due to their expectancy of survival. Additionally, teaching and training of HPN monitoring is transferred in part or completely in the home setting in the presence of caregivers/family members.
3. Monitoring Process
For many years, we have used the approach described hereinafter to monitor the response to HPN in cancer patients (Figure 1) [5][25]. However, the practical tips described in this review are mostly based on expert opinion.
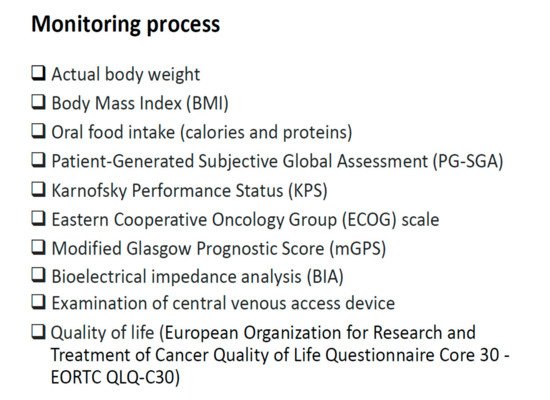
Figure 1. Parameters and indicators to monitor the response to Home Parenteral Nutrition in cancer patients.
The application of these suggestions could be facilitated by implementing dedicated services and pathways, and assigning duties to dedicated healthcare providers (i.e., physicians and dietitians expert in clinical nutrition in oncology) in each oncologic center. The evaluation of eligibility of a cancer patient for the HPN program is requested mainly by oncologists, but also by surgeons, internal medicine physicians, and general practitioners. Inpatients are assessed during the consultations carried out in the wards before discharge, while outpatients are assessed in dedicated hospital rooms in the Comprehensive Cancer Center. The criteria for accepting patients in the HPN program follow the European guideline recommendations for eligibility [10][4] and were already described [5][25].
After the start of HPN, patients are monitored on a regular basis (at least every two weeks) through planned and structured telephone interviews by the clinician in charge of the HPN. Additionally, visits at home by the nurse and general practitioner are scheduled initially every day for two to three weeks and every week thereafter. Only after appropriate training can the patient’s caregiver self-manage PN. Telephone assistance by a physician is available for patients as well as their caregivers and healthcare providers at all times. HPN is delivered using standard nutritional bags, commercially manufactured and ready-to-use, containing glucose, amino acids, lipids, and electrolytes overnight for 10–14 h per day through a CVAD. The HPN program is personalized to meet calories, protein, and water requirements. Generally, HPN is prescribed to provide a range between 25 and 30 kcal per kg per day, depending on the patient’s activity of daily living, and an amino acid supply between 1 and 1.5 g per kg per day. After the start of HPN, approximately every month (±5 days), the patient undergoes a hospital re-evaluation by both the dietitian (including a 24-h food recall) and clinician. If the patient needs admission to hospital, he/she is referred to the HPN-teaching hospital.
4. Anthropometric Measures
Body weight is surely the most common indicator used to monitor cancer patients on HPN. However, handling nutritional requirements based only on actual body weight or weight changes is confusing. Indeed, when evaluating body weight misleading factors as ascites, edema, or pleural effusion should be taken into account.
Similarly, body mass index (BMI) may be a confounding measure. Indeed, patients may have same BMI, but markedly different lean mass. For instance, an obese patient may have an important loss of lean body mass that is hidden by a significant mass of fat. This issue is relevant because sarcopenic obesity is associated with an increase in incidence of dose-limiting toxicity [11][2].
5. Assessment of Oral Food Intake
A recurrent and scheduled quantification of oral food intake is also important in patients on HPN, especially in those on SPN. Indeed, patient’s nutrient balance is determined by oral intake plus SPN support minus expenditure. Additionally, the assessment of food intake can also evaluate whether the severity of patient’s nutrition-impact symptoms is likely to improve or increase. Therefore, this assessment is a key element for monitoring patients and may predict earlier than weight loss the need of a switch from SPN to TPN.
The evaluation of patient’s oral food intake is performed by skilled dietitians using a well-designed interview (24-h food recall). During this interview, the dietitian asks the patient to report which foods and drinks he/she has eaten during the previous 24 h. However, this tool has considerable limits and potential significant errors, even if it is performed by skilled personnel (Figure 2).
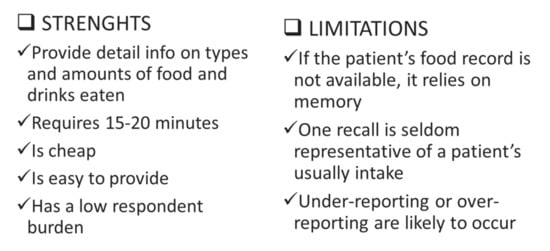
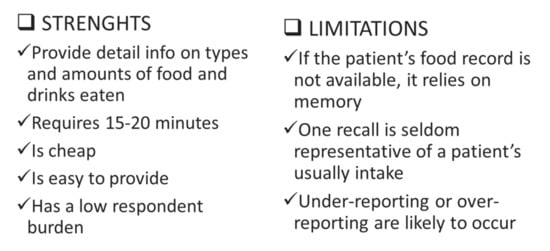
Figure 2. Oral food intake by 24-h food recall.
6. Assessment of Nutritional Status
Screening is a simple and rapid process to select patients who are at risk of malnutrition or malnourished. Conversely, assessment of nutritional status is a diagnostic process, which individualizes the degree of malnutrition, and it is obviously more complex and time-consuming than screening.
The analysis of nutritional status is useful to complete objective assessments with subjective evaluations. The Patient-Generated Subjective Global Assessment (PG-SGA) [12][27] has demonstrated to be effective in assessing nutritional status in cancer patients [13][14][28,29]. The PG-SGA uses semi-quantitative and qualitative indicators to classify patients in category A (well-nourished), category B (moderately malnourished), or category C (severely malnourished).
This tool has five items: weight, nutrient intake, nutrition-impact symptoms, functioning, and physical exam). It was designed so that the components of the medical history can be completed by the patient using a check box format while the physical exam is performed by a physician or dietitian. History weight loss is a more accurate predictive factor than actual body weight as well as severe deficit of oral food intake and the presence of nutrition impact symptoms. The fourth item of this tool is the patient’s functional capacity or energy level (bedridden to full capacity). Finally, the PG-SGA evaluates muscle wasting (quadriceps, deltoids) and loss of subcutaneous fat by a physical examination. Inspection and palpation for edema and ascites are important because cannot only be indicators of patient’s status, but also suggests that actual body weight or weight changes may be misleading elements.
Several studies showed the usefulness of PG-SGA to evaluate patient’s nutritional status, as well as its ability to predict mortality in oncology patients [15][30]. Specifically, patients who were ranked as severely malnourished or declined from category B to C had the shortest median survival, and those who improved to a rating of category A had the longest median survival [16][31]. Therefore, by monitoring response to HPN using PG-SGA we can assume that category C is a strong predictor of mortality and category A is a predictor of longer survival.
