Indirect structural muscle injuries (commonly referred as “muscle tears”) are the more commonly found in everyday clinical practice and represent the biggest challenge in rehabilitation, since these lack a precise therapeutic strategy. Structural muscle injuries classification is shown in.
- muscle injury
- rehabilitation
- sport medicine
1. Introduction
Even though several scientific studies have tried to propose different rehabilitation protocols, to design a particular rehabilitation pathway for each muscular injury based on its grade and/or location is a difficult task; moreover, several commercial physical or instrumental therapies are becoming increasingly used for muscle injury treatment and rehabilitation, even if scientific evidence about their use are discordant [9,14][1][2].
In subjects affected by muscle injuries, the diagnostic and rehabilitative approach relies on several factors, such as age, gender, athletic demands, muscular groups involved and type of injury. To this scope, several classifications have been proposed over the years. All these classifications are based on some common criteria such as mechanism of injury (direct or indirect) and degree of lesion of muscle tissue (structural or non structural).
In a real-life scenario, the indirect structural muscle injuries represent the most common type of muscle injuries, and some muscle groups of lower limb are affected predominantly.
Therefore, the aim of the present paper is to review proposed therapeutic algorithms for indirect structural muscle injuries of the lower limb, with a particular insight on hamstrings, adductors, rectus femoris and calf muscles rehabilitation.
2. Muscle Injuries Rehabilitation
There are several classifications of muscle injuries, such as the Munich Muscle Injury Classification, the ISMuLT (Italian Society of Muscles, Ligaments and Tendons) classification, and the British Athletic Classification, that, if used extensively, could improve diagnosis, prognosis and management of muscle injuries [15][3]. Depending on the mechanism of trauma, according to ISMuLT classification [9][1], muscle injuries may be distinguished as direct and indirect; indirect ones are in turn classified as non-structural and structural. While direct muscle injuries are often the result of external forces, indirect muscle injuries are stretch-induced injuries caused by a sudden forced lengthening over the viscoelastic limits of muscles occurring during a powerful contraction [9,15][1][3]. Indirect structural muscle injuries (commonly referred as “muscle tears”) are the more commonly found in everyday clinical practice and represent the biggest challenge in rehabilitation, since these lack a precise therapeutic strategy. Structural muscle injuries classification is shown in Table 1 .
| Severity | Site | Tissue | Relapse |
|---|---|---|---|
| 3A: minor partial lesion | P: proximal | MF: myofascial | R0: first lesion |
| 3B: moderate partial lesion | M: medium | MT: muscular belly and myotendinous junction | R1: first relapse |
| 4: subtotal or total lesion and tendon avulsion | D: distal | T: central tendon or free | R2: second relapse |
| R3: third relapse |
Severity [16][4], site [17][5], tissue [3][6], and relapse [18][7] are important features to consider when a muscle injury has been diagnosed. Proximal hamstring and quadricep lesions have a worse prognosis, as well as distal calf injuries; moreover, myotendinous junction lesions seem to have a longer recovery period [19][8]. Therefore, type and location of muscular injuries can influence recovery strategies [3][6] and proposed exercises should respect the principles of specificity, progression, and individualization, respecting painful symptomatology [14,20,21][2][9][10]. Moreover, location of injury, properly marked, could be useful for a focused therapy. Minor or moderate partial lesions (3A and 3B) are prevalent in sport rehabilitation and their conservative management is more controversial, since (sub)total lesions (4) are generally intended for surgery.
Ultrasonography (US) offers dynamic muscle assessment and is fast and relatively inexpensive, allowing serial evaluation of the healing process [9][1]. However, it should be noted that ultrasonography of skeletal muscles requires a high level of skill on the part of the sports physician. It is recommended to use a 7.5- to 10.0-MHz transducer, starting with a transversal section. A complete scan through the muscle should be performed for the purposes of anatomical orientation. Any apparent abnormalities should be compared with the contralateral side. The transducer pressure should be as light as possible, since compressing the muscle may obscure smaller injuries. The longitudinal section is added in locations where a disturbance of the muscle structure or a gap is suspected. In addition, the use of novel US technique could help in this difficult diagnostic process, such as echo intensity [24][11]. When clinical and ultrasonography evaluation are discordant, or for muscles not accessible to US examination, in elite athletes, Magnetic Resonance Imaging (MRI) may be required to confirm or exclude minor structural injuries, since this technique is often used as a second-line investigation in musculoskeletal diseases [25,26][12][13]. MRI plays only a marginal role in the follow-up and monitoring of structural injuries because the images do not correlate well enough with the clinical evaluation, causing a potential late return to play (RTP) for the athlete.
In this phase, the myofibers intertwining is effectively completed by the interposition of a small amount of scar tissue. There should be proposed strength and extensibility exercises that induce remodeling of the repair tissue based on the sport played [9][1], depending also on the movement that caused the injury. The remodeling phase may last more than 60 days, depending on the anatomical extent of the injury [9][1].
3. Specific Exercise Rehabilitation
Even though there are so many rehabilitation exercises used, it is the authors’ opinion that each muscle injury should be treated differently, trying to individualize it as much as possible. They should follow a well-structured timetable that is appropriate for the specific injury or disorder: as we stated before, the correct progression should be isometric (1st phase), concentric (2nd phase) and eccentric (3rd phase) exercises; proprioceptive, neuromuscular and stretching exercises also have a major role in the rehabilitation process. Below we propose examples of exercises for hamstrings ( Table 2 ), rectus femoris ( Table 3 ), adductors ( Table 4 ), and calf injuries ( Table 5 ), along with their criteria for RTT and secondary prevention programs.
Hamstring
| Name | Image | Reference |
|---|---|---|
| Isometric exercises | ||
| (In case of proximal hamstring lesion) |  |
[23] |
| (In case of medial or distal hamstring lesion) |  |
[23] |
| Isometric exercise at different angles |  |
[23] |
| Dynamic exercises | ||
| The extender | 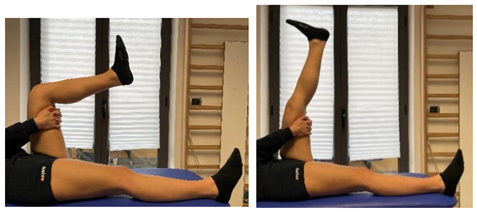 |
[88,97] |
| The glider |  |
[88,97] |
| Nordic hamstrings |   |
[97] |
| Proprioceptive, neuromuscular and stretching exercises | ||
| Pendulum |  |
[97] |
| Stretching Single Leg Raises | 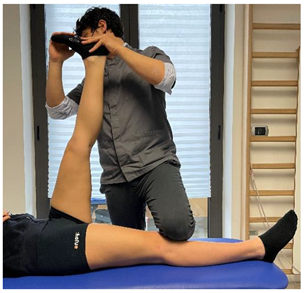 |
[97] |
| Secondary prevention exercises | ||
| Eccentric knee flexor stretch | 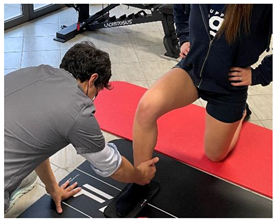 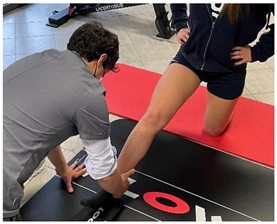 |
[98] |
| Eccentric hip extensor stretch |  |
[98] |
Hamstring rehabilitation exercises.
| Name | Image | Reference |
|---|---|---|
| Isometric exercises | ||
| (In case of proximal lesion) | 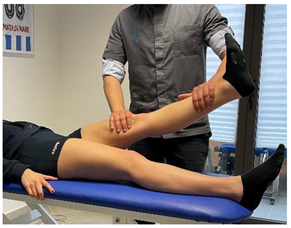 |
[23] |
| (In case of medial or distal lesion) |  |
[23] |
| Dynamic exercises | ||
| (In case of proximal lesion) | 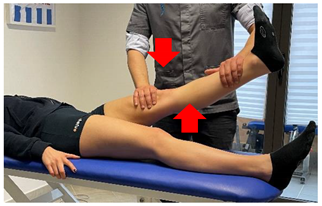 |
[23] |
| (In case of medial or distal lesion) | 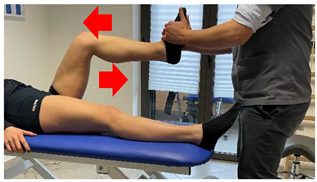 |
[23] |
| Secondary prevention exercises | ||
| Eccentric hip flexor and knee extensor stretch (eccentric load to rectus femoris) |
 |
[98] |
Quadriceps
| Name | Image | Reference |
|---|---|---|
| Isometric exercises | ||
| Isometric exercise with ball |  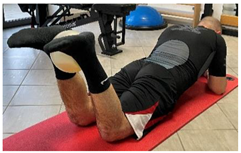 |
[23] |
| Dynamic exercises | ||
| Manual resisted adduction |  |
[23] |
| Adduction with elastic resistance | 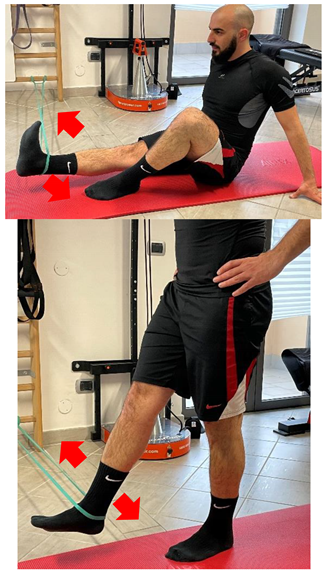 |
[23] |
| Proprioceptive, neuromuscular, and stretching exercises | ||
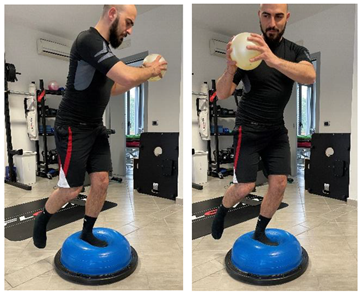 |
[23] | |
| Secondary prevention exercises | ||
| Eccentric side lunge stretch |   |
[98] |
| Copenhagen adductor prevention programs |  |
[99] |
Quadriceps rehabilitation exercises.
| Name | Image | Reference |
|---|---|---|
| Isometric exercises | ||
| Isometric contraction with manual resistance |  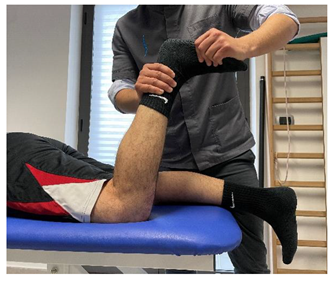 |
[23] |
| Dynamic exercises | ||
| Concentric/eccentric contraction with manual resistance |  |
[23] |
| Concentric/eccentric heel raise |  |
[23] |
| Proprioceptive, neuromuscular, and stretching exercises | ||
 |
[23] | |
Adductors
Adductors rehabilitation exercises.
Soleus-gastrocnemius
Soleus-gastrocnemius rehabilitation exercises.
4. Return to Training (RTT) and Return to Play (RTP)
US examination upon complete RTT and a few days after the RTP is recommended [100][14]. There are no validated imaging criteria to guide the decision of a safe RTP. To date, no study has suggested US to guide the RTP decision, but a few studies have focused on MRI following hamstring injury [101,102,103,104][15][16][17][18]. Normalization of increased signal intensities on MRI is therefore not required for a successful RTP, since the signal alterations also persist at different weeks after the clinical healing of the injury, suggesting that functional recovery advances structural recovery at imaging [9][1].
To define a set of tests to determine the correct timing of RTT is a difficult task. Specific assessment for each muscle group, laboratory tests aimed to assess muscle strength, and functional field tests could be adopted as criteria to define a safe RTT.
Based on the available literature, a list of tests has been defined to each muscle groups and are reported in Table 6 .
| Hamstring | |
| Specific assessment |
|
| Laboratory test |
|
| Field test |
|
| Quadriceps | |
| Specific assessment |
|
| Laboratory test |
|
| Field test |
|
| Adductors | |
| Specific assessment |
|
| Laboratory test |
|
| Field test |
|
| Soleus-gastrocnemius | |
| Specific assessment |
|
| Laboratory test |
|
| Field test |
|
The aim of these tests and their specific execution are out of the scope of the present paper, but the rationale behind each test is reported in the references and could be used to guide the RTT and RTP processes.
References
- Nanni, G.; Frizziero, A.; Oliva, F.; Maffulli, N. Gli Infortuni Muscolari-Linee Guida, I.S.Mu.L.T; Calzetti Mariucci Editore: Torgiano, Italy, 2020.
- Järvinen, T.A.; Järvinen, M.; Kalimo, H. Regeneration of injured skeletal muscle after the injury. Muscles Ligaments Tendons J. 2013, 3, 337–345.
- Maffulli, N.; Aicale, R.; Tarantino, D. Classification of Muscle Lesions. In Muscle and Tendon Injuries; Canata, G., d’Hooghe, P., Hunt, K., Eds.; Springer: Berlin/Heidelberg, Germany, 2017.
- Mueller-Wohlfahrt, H.-W.; Haensel, L.; Mithoefer, K.; Ekstrand, J.; English, B.; McNally, S.; Orchard, J.; van Dijk, C.N.; Kerkhoffs, G.M.; Schamasch, P.; et al. Terminology and classification of muscle injuries in sport: The Munich consensus statement. Br. J. Sports Med. 2013, 47, 342–350.
- Chan, O.; Del Buono, A.; Best, T.M.; Maffulli, N. Acute muscle strain injuries: A proposed new classification system. Knee Surg Sports Traumatol. Arthrosc. 2012, 20, 2356–2362.
- Pollock, N.; James, S.L.J.; Lee, J.C.; Chakraverty, R. British athletics muscle injury classification: A new grading system. Br. J. Sports Med. 2014, 48, 1347–1351.
- Valle, X.; Alentorn-Geli, E.; Tol, J.L.; Hamilton, B.; Garrett, W.E., Jr.; Pruna, R.; Til, L.; Antoni Gutierrez, J.; Alomar, X.; Balius, R.; et al. Muscle Injuries in Sports: A New Evidence-Informed and Expert Consensus-Based Classification with Clinical Application. Sports Med. 2017, 47, 1241–1253.
- Ekstrand, J.; Askling, C.; Magnusson, H.; Mithoefer, K. Return to play after thigh muscle injury in elite football players: Implementation and validation of the Munich muscle injury classification. Br. J. Sports Med. 2013, 47, 769–774.
- Mendiguchia, J.; Martinez-Ruiz, E.; Edouard, P.; Morin, J.B.; Martinez-Martinez, F.; Idoate, F.; Mendez-Villanueva, A. A Multifactorial, Criteria-based Progressive Algorithm for Hamstring Injury Treatment. Med. Sci. Sports Exerc. 2017, 49, 1482–1492.
- Khan, K.M.; Scott, A. Mechanotherapy: How physical therapists’ prescription of exercise promotes tissue repair. Br. J. Sports Med. 2009, 43, 247–252.
- Wong, V.; Spitz, R.W.; Bell, Z.W.; Viana, R.B.; Chatakondi, R.N.; Abe, T.; Loenneke, J.P. Exercise induced changes in echo intensity within the muscle: A brief review. J. Ultrasound. 2020, 23, 457–472.
- Zappia, M.; Ascione, F.; Di Pietto, F.; Fischetti, M.; Romano, A.M.; Castagna, A.; Brunese, L. Long head biceps tendon instability: Diagnostic performance of known and new MRI diagnostic signs. Skelet. Radiol. 2021, 50, 1863–1871.
- Zappia, M.; Reginelli, A.; Chianca, V.; Carfora, M.; Di Pietto, F.; Iannella, G.; Mariani, P.P.; Di Salvatore, M.; Bartollino, S.; Maggialetti, N. MRI of popliteo-meniscal fasciculi of the knee: A pictorial review. Acta. Biomed. 2018, 19, 7–17.
- Di Prampero, P.E.; Botter, A.; Osgnach, C. The energy cost of sprint running and the role of metabolic power in setting top performances. Eur. J. Appl. Physiol. 2015, 115, 451–469.
- Bisciotti, G.N.; Volpi, P.; Alberti, G.; Aprato, A.; Artina, M.; Auci, A.; Bait, C.; Belli, A.; Bellistri, G.; Bettinsoli, P.; et al. Italian consensus statement (2020) on return to play after lower limb muscle injury in football (soccer). BMJ Open Sport Exerc. Med. 2019, 5, e000505.
- Silder, A.; Heiderscheit, B.C.; Thelen, D.G.; Enright, T.; Tuite, M.J. MR observations of long-term musculotendon remodeling following a hamstring strain injury. Skelet. Radiol. 2008, 37, 1101–1109.
- Reurink, G.; Almusa, E.; Goudswaard, G.J.; Tol, J.L.; Hamilton, B.; Moen, M.H.; Weir, A.; Verhaar, J.A.; Maas, M. No association between fibrosis on magnetic resonance imaging at return to play and hamstring reinjury risk. Am. J. Sports Med. 2015, 43, 1228–1234.
- Sanfilippo, J.L.; Silder, A.; Sherry, M.A.; Tuite, M.J.; Heiderscheit, B.C. Hamstring strength and morphology progression after return to sport from injury. Med. Sci. Sports Exerc. 2013, 45, 448–454.
