Linear IgA disease (LAD) is an autoimmune mucocutaneous disease characterized by linear deposits of IgA at the basement membrane zone on immunopathology. It is also known as linear IgA bullous dermatosis (LABD), but LAD is preferred because it is inclusive of patients without bullous lesions. In the pediatric population, it is known as chronic bullous disease of childhood (CBDC).
- linear IgA bullous dermatosis
- autoimmune diseases
- immunoglobulin A
- fluorescent antibody technique
- rituximab
- etanercept
- omalizumab
1. Introduction
Linear IgA disease (LAD) is an autoimmune mucocutaneous disease characterized by linear deposits of IgA at the basement membrane zone on immunopathology [1]. It is also known as linear IgA bullous dermatosis (LABD), but LAD is preferred because it is inclusive of patients without bullous lesions [2]. In the pediatric population, it is known as chronic bullous disease of childhood (CBDC). Direct immunofluorescence (DIF) remains the gold standard for diagnosis in both adult and pediatric populations, but there have been cases of false-negative results in drug-induced LAD [3][4]. Management of this relatively rare disease process varies throughout the literature. Dapsone is the most commonly used therapeutic agent, but its potential side effects such as hemolysis, agranulocytosis, and methemoglobinemia necessitate the use of other treatment modalities. Monitoring for dapsone adverse reactions can be cumbersome as well. Numerous other treatments have been reported to be effective in the treatment of LAD, including topical corticosteroids, tetracyclines, dicloxacillin, oxacillin, erythromycin, sulfonamides, nicotinamide, rituximab, omalizumab, methotrexate, cyclosporine, etanercept, and intravenous immunoglobulin (IVIg) [1][5][6][7][8][9][10][11][12][13][14][15][16][17][18][19][20][21].
2. Current Findings
2.1. Literature Search
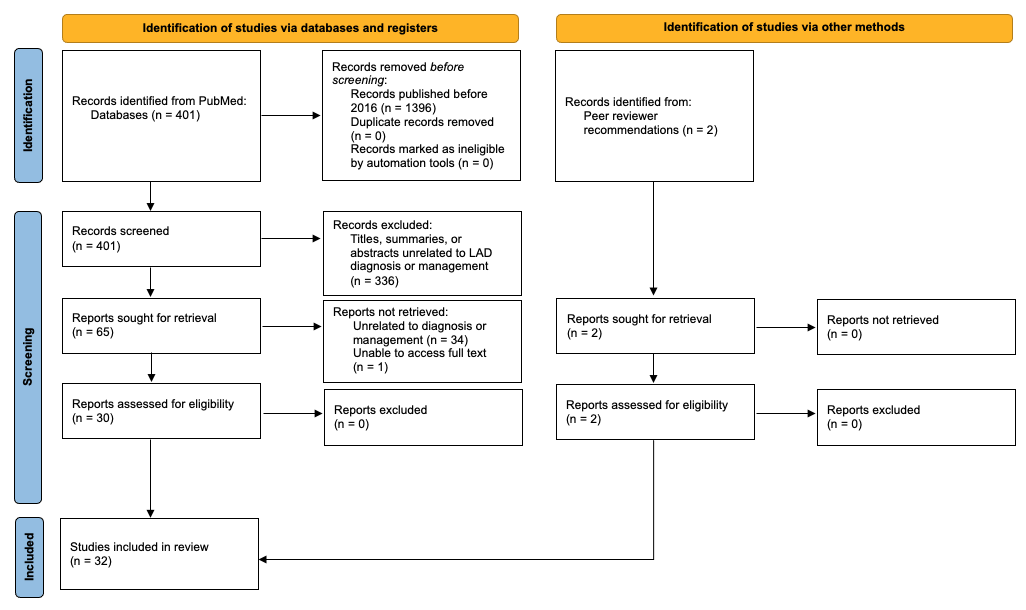
A preliminary search yielded 401 articles published between 2016 and 2021 that were related to “linear igA”. The titles, summaries, and abstracts were screened for relevance to the topic, leaving a total of 65 articles. These studies were assessed further by reading the abstract or full text. Articles without full-text access or those that were unrelated to diagnosis or management were not retrieved. This left 30 studies that met the inclusion criteria, in addition to 2 articles recommended by peer reviewers (Figure 1).
Figure 1. Flow diagram of the systematic review.
2.2. Diagnosis
2.3. Treatment
In recent years, rituximab, IVIg, and others have been increasingly utilized and reported due to the adverse effects, lack of access, and treatment failure of dapsone (Table 1). These agents were often used in combination with systemic corticosteroids. There are only a few published cases that used omalizumab and etanercept, therefore data are limited on the efficacy of these agents as a treatment for LAD. In the pediatric population, management tended to be more conservative with systemic and topical corticosteroids or nicotinamide. Dosing regimens, time to clearance, and relapse rates varied throughout this literature review.
Table 1. Review of alternative therapeutic agents documented in the literature from 2016 to 2021.
|
Drug |
Dose |
Age (Years) |
Drug-Induced LAD (Y/N) |
Time to Clearance (yrs/m/w/d) |
Relapse (Y/N) |
Side Effects of Treatment |
|
Rituximab + prednisone + MMF [11] |
Rituximab: 375 mg/m2 weekly ×4 w Prednisone: 0.5 mg/kg (80 mg) tapered over 1 m MMF: 500 mg |
43 |
N |
1 m |
Y, 9 m later |
NS |
|
Rituximab + dapsone + topical corticosteroids + MMF [8] |
Rituximab: 2 infusions of 1 g 2 w apart ×2 Dapsone: unspecified Topical corticosteroids: unspecified MMF: 3 g/d to 500 mg/d |
35 |
Unknown |
14 m |
Y, 6 m later |
NS |
|
Rituximab + dapsone + IVIg [9] |
Rituximab: 1 g ×2 cycles Dapsone: 100 mg to 50 mg IVIg: 2 g/kg/cycle |
33 |
N |
7 w |
N |
None |
|
Rituximab + dapsone + prednisone + doxycycline + MMF [8] |
Rituximab: 2 infusions of 1 g 2 w apart ×2 Dapsone: 200 mg/d Prednisone: 0.1 mg/kg/d Doxycycline: 200 mg/d MMF: 1 g/d |
30 |
Unknown |
20 m |
N |
NS |
|
Rituximab + IVIg [12] |
Rituximab: 2 infusions of 1 g 2 w apart IVIg: 2 g/kg/cycle divided over 3 d ×2 |
21 |
Unknown |
17 m follow-up showed improvement in visual acuity and less conjunctival cicatrization |
N |
None * |
|
Omalizumab |
Dose regimen 1: Subcutaneous 300 mg every m ×6 m [13] Dose regimen 2: Subcutaneous 300 mg every m ×3 m [14] |
55 40 |
N Unknown |
3 w 4.5 m |
Y, within 1 m of cessation N |
NS NS |
|
Etanercept [17] |
50 mg ×1 |
65 |
Y |
4 d |
NS |
None |
|
Methotrexate + mesalamine ** after high dose prednisone + IV methylprednisolone [15] |
Methotrexate: 22.5 mg/w Mesalamine: unspecified Prednisone: unspecified Methylprednisone: 3 d course |
58 |
N |
NS, but near clearance achieved |
NS |
NS |
|
Sulfasalazine [6] |
40–60 mg/kg daily |
17 |
N |
2 m |
N |
None |
|
Sulfamethoxypyridazine [30] |
250 mg–1 g/d |
7 |
N |
60 m |
N |
NS |
|
IVIg + prednisolone [19] |
IVIg: 2 g/kg or 0.4 g/kg for a median of 6 doses over 2–5 d + Prednisolone: 5–10 mg/d |
Unspecified, range of 64–84 |
Unknown |
NS |
N |
None *** |
|
IVIg + prednisolone [30] |
IVIg: 2 g/kg/cycle ×8 Prednisolone: 0.5–1 mg/kg/d |
13 |
N |
30 m |
N |
NS |
|
IVIg [30] |
2 g/kg/cycle ×8 cycles |
9, 1.7 |
N |
96 m, 7 m |
N |
NS |
|
IVIg + prednisolone + clarithromycin [30] |
IVIg: 2 g/kg/cycle monthly ×5 Prednisolone: 1 mg/kg/d Clarithromycin: 30 mg/kg/d over 3 doses |
1 |
N |
6 m |
N |
NS |
|
Dapsone + prednisone [29] |
Dapsone: 50 mg/d Prednisone: 0.6 mg/kg (60 mg/d) |
51 |
N |
2.5 yrs |
N |
NS |
|
Dapsone + prednisone [29] |
Dapsone: 50 mg/d Prednisone: 1 mg/kg/d (60 mg/d) tapered to 10 mg/d |
44 |
N |
Clearance not achieved |
Clearance not achieved |
Glaucoma, arterial hypertension, osteoporosis, Cushingoid facies |
|
Prednisone [29] |
20 mg/d monthly dose tapering |
30 |
Unknown |
NS |
Y |
NS |
|
Dapsone + prednisolone [30] |
Dapsone: 1–2 mg/kg/d Prednisolone: 0.5–1 mg/kg/d in tapering doses |
13, 9, 7, 1 |
N |
60 m, 156 m, 108 m, 24 m |
N |
NS |
|
Oral corticosteroids [31] |
Unspecified |
8 |
NS |
4 m |
NS |
NS |
|
Oral prednisolone + corticosteroid eye drops [25] |
0.5 mg/kg/d |
7 |
NS |
NS, but had eyelid adhesion despite clinical control |
NS |
NS |
|
Dapsone + prednisolone + cyclosporine [16] |
Dapsone: 0.5–2 mg/kg; Prednisolone: 0.5–1 mg/kg Cyclosporine: dose unspecified |
5 |
N |
NS, but is well-controlled |
NS |
NS |
|
Topical triamcinolone + vancomycin cessation [3] |
Triamcinolone 0.1% ointment |
74 |
Y |
NS, but clearance was achieved |
NS |
NS |
|
Topical methylprednisolone + clobetasol shampoo [20] |
Methylprednisolone: 0.1% BID ×8 w |
6 |
N |
5–8 w |
N |
NS |
|
Topical corticosteroids + clarithromycin [30] |
Topical corticosteroids: mid-potency, unspecified Clarithromycin: 30 mg/kg/d over 3 doses ×1 m |
5 |
N |
2.5 m |
N |
NS |
|
Topical corticosteroids [30] |
Mid-potency, unspecified |
4 |
N |
2.5 m |
N |
NS |
|
Betamethasone valerate [21] |
0.05% |
4 d |
N |
21 d |
NS |
NS |
|
Nicotinamide [7] |
300 mg/d |
22 m |
N |
7 d |
N |
None |
|
Amoxicillin-clavulanate [28] |
Infusion ×7 d |
7 d |
N |
7 d |
N |
NS |
yrs, years; m, months; w, weeks; d, days; Y, Yes; N, No; NS, not stated. * While the patient with LAD did not experience side effects from Rituximab + IVIg, one patient diagnosed with MMP experienced pneumonia and life-threatening septicemia 3 weeks after RTX infusions, which was successfully treated with very aggressive intravenous antibiotic therapy. ** Patient was also being treated for chronic ulcerative proctitis. *** While the patient with LAD did not experience side effects from IVIg, patients in the study with pemphigus vulgaris, vasculitis, vasculopathy, and dermatomyositis experienced headache, abdominal pain, gastrointestinal upset, and chest pain.
2.2.1. Rituximab
2.2.2. Methotrexate
2.2.3. Sulfonamides
2.2.4. IVIg
2.2.5. Topical Corticosteroids
2.2.6. Systemic Corticosteroids
2.2.7. Nicotinamide
2.2.8. Amoxicillin-Clavulanate
3. Current Insights
4. Conclusions
LAD management has relied on DIF for diagnosis and on dapsone for treatment. A literature search for articles published in the last 5 years has shown that other modalities, including rituximab, omalizumab, etanercept, IVIg, topical corticosteroids, among others have been used successfully in adult and pediatric patients with varying severity of disease. Patient factors such as age, medical comorbidities, and disease severity play a role in therapeutic selection. As in most patient cases in Dermatology where preliminary biopsy results are negative but clinical suspicion is high, a repeat biopsy and additional diagnostic studies should be considered, especially in LAD.
References
- Bernett, C.N.; Fong, M.; Rosario-Collazo, J.A.; Linear, I.G.A. Dermatosis. [Updated 2021 Jan 15]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK526113/ (accessed on 29 June 2021).
- Hashimoto, T.; Yamagami, J.; Zone, J.J. History, Diagnosis, Pathogenesis, and Nomenclature in Sublamina Dense-Type Linear IgA Disease. JAMA Dermatol. 2021.
- Winn, A.E.; Spillane, E.L.; Peterson, D.J.; Sperling, L.C.; Meyerle, J.H. False-negative direct immunofluorescence testing in vancomycin-induced linear IgA bullous dermatosis: A diagnostic pitfall. J. Cutan. Pathol. 2016, 43, 802–804.
- Yamagami, J.; Nakamura, Y.; Nagao, K.; Funakoshi, T.; Takahashi, H.; Tanikawa, A.; Hachiya, T.; Yamamoto, T.; Ishida-Yamamoto, A.; Tanaka, T.; et al. Vancomycin Mediates IgA Autoreactivity in Drug-Induced Linear IgA Bullous Dermatosis. J. Investig. Dermatol. 2018, 138, 1473–1480.
- Vale, E.C.S.D.; Dimatos, O.C.; Porro, A.M.; Santi, C.G. Consensus on the treatment of autoimmune bullous dermatoses: Dermatitis herpetiformis and linear IgA bullous dermatosis—Brazilian Society of Dermatology. An. Bras. Dermatol. 2019, 94, 48–55.
- Yang, Z.; Liu, Z.; Sun, C.; Shen, H. Successful treatment of a case of idiopathic linear IgA bullous dermatosis with oral sulfasalazine. Dermatol. Ther. 2020, 33, e13210.
- Cui, Y.X.; Yang, B.Q.; Zhou, G.Z.; Zhang, F.R. Childhood linear IgA bullous dermatosis successfully treated with oral nicotinamide. Clin. Exp. Dermatol. 2016, 41, 816–818.
- Pinard, C.; Hebert, V.; Lecuyer, M.; Sacre, L.; Joly, P. Linear IgA bullous dermatosis treated with rituximab. JAAD Case Rep. 2019, 5, 124–126.
- Islamoğlu, Z.G.K.; Akyürek, F.T. A case of recalcitrant linear IgA bullous dermatosis: Successfully treated with rituximab. Dermatol. Ther. 2019, 32, e12911.
- Lamberts, A.; Euverman, H.I.; Terra, J.B.; Jonkman, M.F.; Horváth, B. Effectiveness and Safety of Rituximab in Recalcitrant Pemphigoid Diseases. Front. Immunol. 2018, 9, 248.
- Nedosekin, D.; Wilson, K.D.; Campbell, K.; Shalin, S.; Wong, H.K. Immunologic overlap in a case of linear IgG/IgA bullous dermatosis responsive to rituximab. JAAD Case Rep. 2021, 9, 57–60.
- Steger, B.; Madhusudan, S.; Kaye, S.B.; Stylianides, A.; Romano, V.; Maqsood, S.E.; Harper, J.; Ahmad, S. Combined Use of Rituximab and Intravenous Immunoglobulin for Severe Autoimmune Cicatricial Conjunctivitis—An Interventional Case Series. Cornea 2016, 35, 1611–1614.
- Maalouf, N.S.; Hanna, D. Linear IgA bullous dermatosis successfully treated with omalizumab: A case report. JAAD Case Rep. 2019, 5, 966–969.
- Patel, N.H.; Padhiyar, J.K.; Patel, T.D.; Trivedi, N.S.; Chandibhamar, V.S.; Raval, R. A case of linear IgA bullous dermatosis successfully treated with omalizumab. Indian J. Dermatol. 2020, 65, 543–545.
- Yetto, T.; Burns, C. Linear IgA bullous dermatosis associated with ulcerative proctitis: Treatment challenge. Derm. Online J. 2018, 24, 14.
- Tate, C.; Christian, W.; Newell, L. Chronic Bullous Dermatosis of Childhood and the String of Pearls Sign. J. Pediatr. 2018, 202, 325–325.e1.
- Prieto-Barrios, M.; Velasco-Tamariz, V.; Tous-Romero, F.; Burillo-Martinez, S.; Zarco-Olivo, C.; Rodriguez-Peralto, J.; Ortiz-Romero, P. Linear immunoglobulin A dermatosis mimicking toxic epidermal necrolysis: A case report of etanercept treatment. Br. J. Dermatol. 2017, 178, 786–789.
- Patsatsi, A.; Lamprou, F.; Kokolios, M.; Stylianidou, D.; Trigoni, A.; Kalampalikis, D.; Sotiriadis, D. Spectrum of Autoimmune Bullous Diseases in Northern Greece. A 4-year Retrospective Study and Review of the Literature. Acta Dermatovenerol. Croat. 2017, 25, 195–201.
- Scarpone, R.; Meier, K.; Ghoreschi, K.; Worm, M. Intravenous Immunoglobulins in a Series of 32 Rare and Recalcitrant Immune Dermatoses. Acta Derm. Venereol. 2020, 100, adv00298.
- Gil Sáenz, F.J.; Urdániz, G.D.; Galar, M.F.; Ballester, J.G.; Varasa, A.H.; Bordege, R.G. Corticoides tópicos como alternativa terapéutica en la dermatosis ampollosa por inmunoglobulina A lineal de la infancia. Caso clínico. Arch. Argent. Pediatr. 2016, 114, e440–e443.
- Mazurek, M.T.; Banihani, R.; Wong, J.; Weinstein, M.; Alnutayfi, A.; Etoom, Y. Uncomplicated Neonatal Linear IgA Bullous Dermatosis: A Case Report. J. Cutan. Med. Surg. 2018, 22, 431–434.
- Fulton, E.; Jan, F.; Zimarowski, M.J. Flame figures in linear IgA bullous dermatosis: A novel histopathologic finding. Dermatol. Online J. 2017, 23, 17.
- Shetty, V.M.; Pai, S.B.; Rao, R. Linear IgA bullous dermatosis presenting as chronic prurigo: Unveiling of the diagnosis by serrated pattern analysis. Int. J. Dermatol. 2018, 57, e147–e149.
- Becker, M.; Schumacher, N.; Schmidt, E.; Zillikens, D.; Sadik, C.D. Evaluation and Comparison of Clinical and Laboratory Characterstics of Patients With IgA Epidermolysis Bullosa Acquisita, Linear IgA Bullous Dermatosis, and IgG Epidermolysis Bullosa Acquisita. JAMA Dermatol. 2021.
- Fernandes, K.D.A.P.; Galvis, K.H.; Gomes, A.C.D.M.S.; Nogueira, O.M.; Felix, P.A.O.; Vargas, T.J.D.S. Linear IgA and IgG bullous dermatosis. An. Bras. Dermatol. 2016, 91 (Suppl. 1), 32–34.
- Lim, G.H.; Cai, S.C.S.; Lee, J.S.S.; Chen, Q. Rare case of linear IgA bullous dermatosis showing IgA, IgG and IgM reactivity. Australas. J. Dermatol. 2021, 62, e361–e362.
- Ohata, C.; Ishii, N.; Koga, H.; Nakama, T. A clinical and serological study of linear IgA bullous dermatosis without linear immunoglobulin deposition other than IgA at the basement membrane zone using direct immunofluorescence. Br. J. Dermatol. 2016, 177, 152–157.
- Nanda, A.; Lazarevic, V.; Rajy, J.M.; Almasry, I.M.; AlSabah, H.; AlLafi, A. Spectrum of autoimmune bullous diseases among children in Kuwait. Pediatr. Dermatol. 2020, 38, 50–57.
- Varo, R.; Fernández-Luis, S.; Sitoe, A.; Bassat, Q. Suspected case of chronic bullous disease of childhood in a rural area of Southern Mozambique. BMJ Case Rep. 2017, 2017, bcr2016218315.
- Machado, T.Y.S.; Enokihara, M.M.S.E.S.; Iida, T.M.; Porro, A.M. Adult linear IgA bullous dermatosis: Report of three cases. An. Bras. Dermatol. 2018, 93, 435–437.
- Giraud, L.; Welfringer-Morin, A.; Boccara, O.; Frassati-Biaggi, A.; Leclerc-Mercier, S.; Grootenboer-Mignot, S.; Bodemer, C.; Hadj-Rabia, S. Neonatal and self-healing linear immunoglobulin A dermatosis. J. Eur. Acad. Dermatol. Venereol. 2019, 34, e86–e87.
- Egami, S.; Suzuki, C.; Kurihara, Y.; Yamagami, J.; Kubo, A.; Funakoshi, T.; Nishie, W.; Matsumura, K.; Matsushima, T.; Kawaida, M.; et al. Neonatal Linear IgA Bullous Dermatosis Mediated by Breast Milk–Borne Maternal IgA. JAMA Dermatol. 2021.