The term “inappropriate secretion of thyroid-stimulating hormone; IST” was proposed by Gershengorn and Weintraub in 1975. In a subsequent report, IST was described as a condition characterized by elevated serum levels of immunoreactive thyroid-stimulating hormone (TSH) in the presence of elevated free thyroid hormone concentrations. Similarly, the term "syndrome of IST (SITSH)" is widely used in Japan to refer to a closely related condition; however, unlike that for IST, an elevated serum free triiodothyronine concentration is not a requisite criterion for SITSH diagnosis. IST or SITSH is an important indicator of resistance to thyroid hormone β (RTHβ) caused by germline mutations in genes encoding thyroid hormone receptor β (TRβ) and TSH-secreting pituitary adenoma.
- thyroid function
- inappropriate secretion of thyroid-stimulating hormone (IST)
- syndrome of inappropriate secretion of thyroid-stimulating hormone (SITSH)
- genuine IST
1. Introduction
Circulating concentrations of thyroid-stimulating hormone (TSH) and other thyroid hormones are tightly regulated in healthy individuals [1]. The liganded thyroid hormone receptor (TR) negatively regulates the synthesis and secretion of TSH in pituitary thyrotrophs, resulting in drastic decreases in serum TSH concentrations [2]. For example, the most common forms of hyperthyroidism, including Graves’ disease and toxic multinodular goiter, demonstrate elevated thyroid hormone levels with suppressed TSH concentrations.
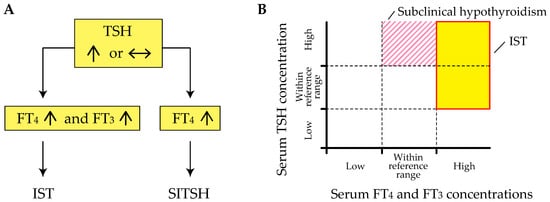
Inappropriate secretion of TSH (IST) is characterized by the laboratory findings of elevated free thyroxine (T4) and triiodothyronine (T3) concentrations in the presence of detectable TSH concentrations [3][4], contrary to what happens in the most common forms of hyperthyroidism (Figure 1 A). This abnormal pattern in the thyroid function test is an important hallmark of genetic and acquired disorders of the hypothalamus-pituitary-thyroid axis (HPT-axis), including resistance to thyroid hormone β (RTHβ) caused by germline mutations in genes encoding the β isoform of the TR (TRβ) and TSH-secreting pituitary adenoma (TSHoma). Although previous review articles have sufficiently investigated several conditions associated with IST, little information is available on systematic pathophysiological aspects of IST in previous review articles. In addition, a recent study has revealed that diagnostic delay and inappropriate treatments (e.g., pituitary surgeries in patients with RTHβ or thyroid ablation in patients with TSHoma) are still provided in several cases with thyroid hormone profiles suggestive of IST [5].
2. Definition of IST
The term “IST” was proposed by Gershengorn and Weintraub in 1975 [6]. In a subsequent report, IST was described as a condition characterized by elevated serum levels of immunoreactive TSH in the presence of elevated free thyroid hormone concentrations [3]. However, it has been suggested that TSH secretion is compensatory and appropriate in RTHβ, because the response to thyroid hormones in peripheral tissues is reduced due to impairment of the TR [7]. Beck-Peccoz et al. also suggested that the definition of “IST” appears inadequate, as it does not reflect the pathophysiological events underlying TSHoma and RTHβ [4]. Therefore, the authors proposed the term “central hyperthyroidism” instead of IST, because TSH itself is responsible for the hyperstimulation of the thyroid gland and the consequent thyrotoxicosis.
The term “syndrome of inappropriate secretion of thyroid-stimulating hormone (SITSH)” has been widely used in journal articles and textbooks written by Japanese researchers since the late 1980s. Based on the 2016 Japan Thyroid Association (JTA) guidelines for the diagnosis of RTHβ, SITSH is defined as being characterized by elevated free T4 and normal-to-elevated TSH concentrations [8] (Figure 1 A). An elevated serum free T3 concentration is not a requisite criterion for SITSH diagnosis. In this study, the author conducted a MEDLINE search using the keyword “SITSH” to retrieve relevant articles published between 1975 and 2020. The literature search yielded 30 articles, of which 28 were published in Japanese institutions.
Physicians must keep in mind that elevated thyroid hormone concentrations are requisite for the diagnosis of IST, because at least two previous studies defined the laboratory findings of inappropriately elevated TSH concentration concurrent with non-elevated thyroid hormone concentrations as the criterion for IST [9][10]. Tyrosine kinase inhibitor therapy, specifically therapy using axitinib, can reportedly cause inappropriately elevated TSH concentrations despite the thyroid hormone concentrations being within the reference range [11]. Similar patterns of thyroid function profiles have been reported in patients with macro-thyrotropin (macro-TSH) [12][13][14], or in those with RTHβ and Hashimoto’s thyroiditis [15]. These findings of thyroid function tests meet the definition of subclinical hypothyroidism but not IST (Figure 1 B).
3. Pathophysiology of IST
Gershengorn and WeintraSub proposed a classification of IST in terms of its pathogenesis [6]. The major classification was fficient evidependent on whether IST was either associated with a neoplasm (class I) or was not (class II). Neoplastic IST (class I) was further classified based on tumor location (i.e., class I-A; pituitary tumors and class I-B; non-pituitary tumors (ectopic production)). Non-neoplastic ISTs (class II) were classified into three groups: RTH (class II-A), abnormal stimulation of TSH secretion by thyrotropin-releasing hormone (TRH) or other stimulators (class II-B), and defective suppression of TSH secretion by somatostatin, dopamine, or other suppressors (class II-C).
Sce has been accumulated for several conditions associated with IST, as summarized in Table 1. In a rececond, Refetoff et al. proposed the term impaired sensitivity to thyroid hormone (ISTH), which includes RTHβ, non-TR-RTH, selenocysteine insertion sequence-binding protein 2 (SBP2) defect, monocarboxylate transporter 8 (MCT8) defect, and RTHα caused by germline mutations in the genes encodingt study reported by Campi and colleagues the α isoform of the TR (TRα) [165]., Among them, the hormonal profile of non-TR-RTH fulfills the definition of IST. In contrast, thyroid function profiles of SBP2 defects, MCT8 defects, and RTHα do not meet the definitionthe term “genuine IST” was used to indicate the etiology of IST, because they are associated with high serum T4 or T3 only concurrent with non-suppressed TSH concentrations [7][17].
Secondincluding TSHoma, in the phenomenon of hysteresis in the HPRT-axis (lagging TSH recovery), persistent TSH elevation (or suppression) with consequent lagging of thyrotroph recovery following hypothyroidism (or thyrotoxicosis) has been documented for many years [18]. DeHβ, and a syndrome clinically and biochemicalayed response of thyrotrophs could result in non-suppression of TSH despite elevated thyroid hormones in several conditions (e.g., pre-existing hypothyroidism secondary to chronic thyroiditis and subsequent onset of destructive thyroiditis, or levothyroxine replacement therapy associated with poor compliance). Here, we focus on the potential mechanism of this condition in terms of epigenetic regulationy indistinguishable from RTHβ but without mutations in the TRβ gene (non-TR-RTH).
Hyst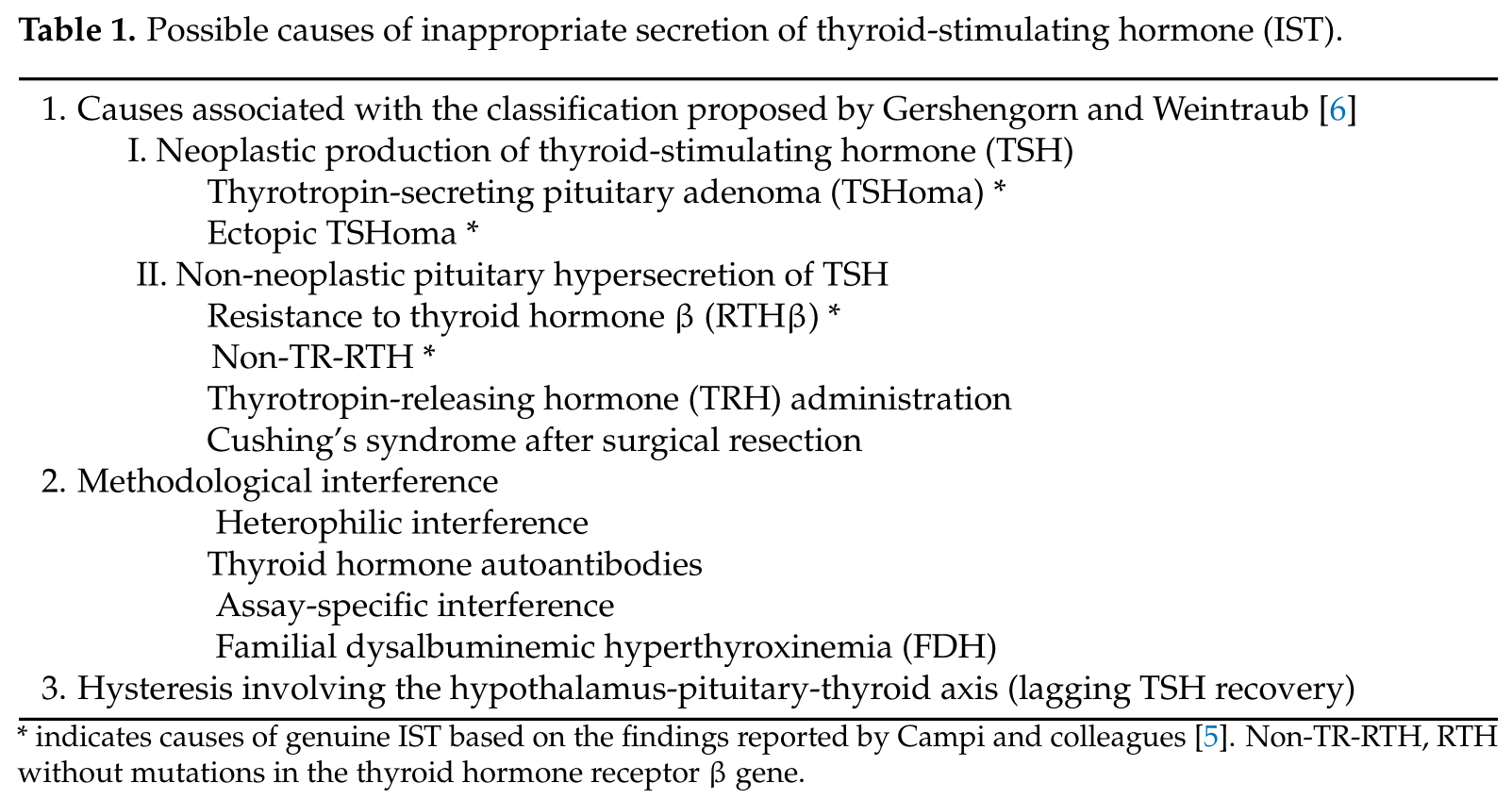
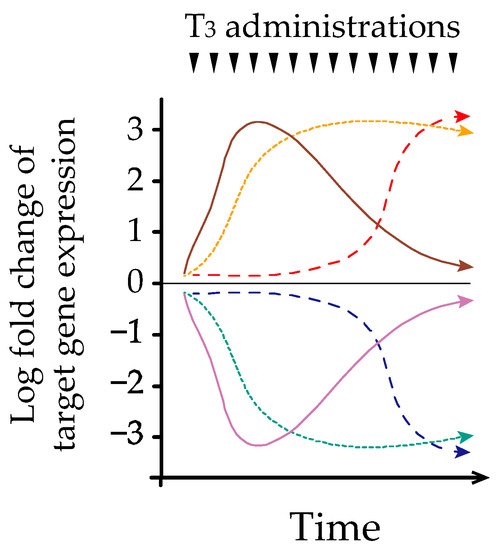
Geresis refers to the phenomenon observed in systems exhibiting a memory effect, such that the response to an input is delayed by a lag time [19]. Melvhengorn and Wein et al. first described hysteresis involving the HPT-axis in 2007 [20]. However, theraub precise mechanism underlying this phenomenon remains poorly understood. We and others have identified early, late, and sustained patterns of hepatic transcriptional responses after acute and/or chronic thyroid hormone treatment in adult murine modelposed a classification of IST in terms [21][22] (Figure 2 ). Further analysis of epigenetic regulation demonstrated that histone H3 acetylation at lysinets pathogenesis 9[6]. and 14 (H3K9/K14ac) was associated witTh acute thyroid hormone stimulation, whereas histone H3 trimethylation at lysine 4 (H3K4me3) is associated with chronic stimule major classification [22]. Similarly, Umezawas et al. reported that chronic thyroid hormone treatment in a rat pituitary cell line caused sustained suppression of TRH, which was dependent on whether IST was either associated with a prolonged decrease in H3K4me3 and only a transient reduction in H3K9/K14ac [23]. Baneoplasm (clased on these findings, different chromatin modifications of target genes could play an important role in regulating transcription during acute and chronic thyroid hormone treatments. We have also reported that thyroid hormones reduce hepatic TRβ protein expression in a time-dependent manner [24]. Taken together, time-dependent I) or was not (class II). Neoplastic IST (changes in transcriptional mechanisms may partly explain the hysteresis of thyroid hormone-responsive genes. Fass I) was further studies are needed to clarify the mechanism of hysteresis associated with the HPT-axis, especially using the pituitary and hypothalamic models.
4. Differential Diagnosis of IST
Oclassified based once the existence of genuine IST is confirmed, it is important to differentiate between RTHβ, non-TR-RTH, and TSHoma [5]umor location (i. The possible presence of neurological signs and symptoms associated with the pressure effects of the pitu., class I-A; pituitary adenoma or clinical features of concomitant hypersecretion of other pittumors and class I-B; non-pituitary hormones supports the probability of pituitary TSHoma occurrence. Because no differences in the basal concentrations of TSH and free thyroid hormones have been reported [25][26], severatumors (ectopic production)). Non-neopl diagnostic steps are required. First, investigating the presence of IST in the family members of a patient can provide important clues for the diagnosis of RTHβ, because no familial cases of TSHoma have been documented [27]. Notably, the fstic ISTs (class II) were classified into three groups: RTH (class II-A), abnorequency of de novo RTHβ cases is approximately 20% [7]. Second, genetic tel sting and imaging studies are useful to confirm the diagnosis of RTHβ and TSHoma, respectively. However, differential diagnosis may be challenging if the pituitary adenoma is very small or missing in patients with the absence of mutations in the TRβ gene. Patients with IST and negative pituitary findings may develop TSHoma during long-term follow-up, as Campi et al. recently reported that pituitary MRI returned negative results in 6 of 26 cases with TSHoma [5]. The differeulation of TSH secretion by thyrotropin-releasing hormontial diagnosis between non-TR-RTH and TSHoma is important in some patients with pituitary adenoma, because approximately 10% of the healthy adult population has pituitary abnormalities on MRI scans that are compatible with the diagnosis of asymptomatic pituitary adenomas (TRH) or other stimulators (class II-B), and [28]. A recent study revealed that 11 out of 45 patients with RTHβ have small pituitary lesions [5].
Several fective supprocedures for the differential diagnosis of problematic cases of IST have been proposed, including dynamic testing and determination of biochemical parameters. In line with dynamic testing, it has been suggested that the combination of dynamic testing could increase the accuracy of the diagnostic workup [26][29]. Firstssion of TSH secretion by somatostatin, the TRH stimulation test demonstrated normal or increased TSH responses (similar to hypothyroid) in most patients with RTHβ or non-TR-RTH, whereas the vast majority of patients with TSHoma do not respond to TRH [25][27][30]. Second, the T3-sopamine, or other suppression test (fixed dose of 75–100 μg of liothyronine (L-T3) administered for 7–10 dayrs (class [31][27]II-C) is useful to evaluate t.
Whe presence of TSHoma, because TSH concentrations after T3-suppression are reportedly higher in cases with TSHoma than in cases with RTHβ [5][32]. Thir Gershengorn and, a standardized diagnostic protocol using incremental doses of L-T3 [33], inWeintraub propostead of a fixed dose is important for the diagnosis of RTHβ and non-TR-RTH, wherein blunted TSH suppression after TRH administration and diminished metabolic response are typically observed [7]. However, dyd their classifications, clinical enamtic tests using fixed or incremental doses of L-T3 are time-consuming and contraindicated in elderly patients or in those with coronary heart diseaseties of I-A and II-A had [32]. Fourth, attention has been paid to dynamic tests using somatostatin analogs (SSAs). Mannavola identified a significant reduction in serum thyroid hormone concentrations after the long-term administration of SSA in patients with TSHoma but not in those with RTHβ [34]. Moocumented, but other classes were receontly, Han et al. demonstrated that even a short-term dynamic test using short-acting SSAs may provide an alternative diagnosticly postulated approach for TSHoma [356].
The measSurement of biochemical parameters is also important to reach a differential diagnosis in problematic cases of IST. Previous stubsequent studies have revealed that serum glycoprotein hormone α-subunit (α-GSU) concentrations are elevated in more than 70% of patients with TSHoma, particularly in those with a macroadenoma [36], whereas thveral condis parameter is within the reference range in most patients with RTHβ or non-TR-RTH [25][27]. Aions or s with other biochemical parameters, measurement of metabolic markers of thyroid hormone action can be helpful in determining peripheral resistance to thyroid hormones. Among these markers, serum sex hormone-binding globulin (SHBG) and carboxy-terminal cross-linked telopeptide of type-I collagen (ITCP) appear to be useful for differential diagnoses [26][29]. Other circulating markers, including alkaline tuations are associated with IST, as prophosphatase, brain natriuretic peptide, cholesterol, creatine kinase, and ferritin are of limited help in assessing the impact of thyroid hormones on peripheral tissues [25][26][37].
For a besed by the autter understanding of the differential diagnosis of problematic cases of IST (or SITSH), several flowcharts have been proposed [5][8][26][29]ors.
