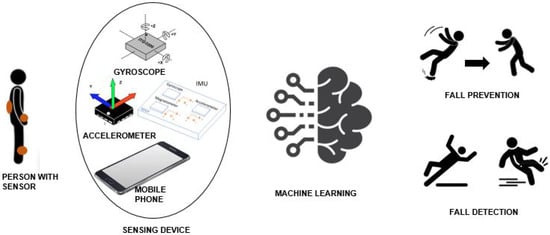
A fall can be described as an unpredicted event leading the participants to rest on the lower level (ground or floor). As a result, it causes injuries that can often be fatal. Psychological grievances are also considered as the consequence of falls. People may suffer from anxiety, depression, activity restriction, and fear of falling. The primary physiological issue in older adults is fear of falling, restricting their Activities of Daily Life (ADL). This fear leads to activity restriction, which may lead to inadequate gait balance and weakened muscle that affects the mobility and independence of older adults. Therefore, remote/wearable technologies are required to track, detect, and prevent falls for improving the overall quality of life (QoL). For this purpose, understanding of falls can be classified as fall prevention and fall detection. Fall detection refers to the detection of a fall using sensors/cameras to summon help. In contrast, fall prevention aims to avert falls by observing human locomotion. Numerous systems have been developed using different sensors and algorithms to detect and prevent the fall.
- fall detection
- fall prevention
- machine learning
1. Overview
Falls are unusual actions that cause a significant health risk among older people. The growing percentage of people of old age requires urgent development of fall detection and prevention systems. The emerging technology focuses on developing such systems to improve quality of life, especially for the elderly. A fall prevention system tries to predict and reduce the risk of falls. In contrast, a fall detection system observes the fall and generates a help notification to minimize the consequences of falls. A plethora of technical and review papers exist in the literature with a primary focus on fall detection. Similarly, several studies are relatively old, with a focus on wearables only, and use statistical and threshold-based approaches with a high false alarm rate. Therefore, this paper presents the latest research trends in fall detection and prevention systems using Machine Learning (ML) algorithms. It uses recent studies and analyzes datasets, age groups, ML algorithms, sensors, and location. Additionally, it provides a detailed discussion of the current trends of fall detection and prevention systems with possible future directions. This overview can help researchers understand the current systems and propose new methodologies by improving the highlighted issues.
2. Fall Detection
-
It provides an overview of the fall detection and prevention systems using wearables and non-wearables.
-
It elaborates on the frequently used ML algorithms in fall detection and prevention.
-
It provides a detailed analysis of the recent state-of-the-art studies. The analysis covers the dataset, participants, ML algorithms, acquisition sensors, and their placements.
-
It evaluates performance parameters such as accuracy, sensitivity, and specificity for different combinations of ML algorithms, sensors, and placements.
-
It provides a detailed discussion on the latest trends in fall detection and prevention systems along with the future directions.
3. Fall Detection and Prevention Systems
32.1. Non-Wearable Systems
32.2. Wearable Systems
32.3. System Overview

References
- Sciubba, J.D. Population Aging as a Global Issue; Oxford Research Encyclopedia of International Studies: Oxford, UK, 2020.
- Bittencourt, V.L.L.; Graube, S.L.; Stumm, E.M.F.; Battisti, I.D.E.; Loro, M.M.; Winkelmann, E.R. Factors associated with the risk of falls in hospitalized adult patients. Rev. Esc. De Enferm. USP 2017, 51.
- United Nations. World Population Ageing 2020 Highlights: Living Arrangements of Older Persons; United Nations Department of Economic and Social Affairs: NY, USA, 2020; Available online: https://www.un.org/development/desa/pd/news/world-population-ageing-2020-highlights (accessed on 24 July 2021).
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology 2016, 17, 567–580.
- Qiu, C.; Johansson, G.; Zhu, F.; Kivipelto, M.; Winblad, B. Prevention of cognitive decline in old age—Varying effects of interventions in different populations. Ann. Transl. Med. 2019, 7, S142.
- Barber, S.J.; Hamel, K.; Ketcham, C.; Lui, K.; Taylor-Ketcham, N. The effects of stereotype threat on older adults’ walking performance as a function of task difficulty and resource evaluations. Psychol. Aging 2020, 35, 250.
- Ćwirlej-Sozańska, A.; Wiśniowska-Szurlej, A.; Wilmowska-Pietruszyńska, A.; Sozański, B. Determinants of ADL and IADL disability in older adults in southeastern Poland. BMC Geriatr. 2019, 19, 1–13.
- Guimarães, V.; Pereira, A.; Oliveira, E.; Carvalho, A.; Peixoto, R. Design and evaluation of an exergame for motor-cognitive training and fall prevention in older adults. In Proceedings of the 4th EAI International Conference on Smart Objects and Technologies for Social Good, Bologna, Italy, 28–30 November 2018; pp. 202–207.
- World Health Organization. WHO Global Report on Falls Prevention in Older Age; World Health Organization: Geneva, Switzerland, 2007.
- Scuffham, P.; Chaplin, S.; Legood, R. Incidence and costs of unintentional falls in older people in the United Kingdom. J. Epidemiol. Community Health 2003, 57, 740–744.
- Ravindran, R.M.; Kutty, V.R. Risk factors for fall-related injuries leading to hospitalization among community-dwelling older persons: A hospital-based case-control study in Thiruvananthapuram, Kerala, India. Asia Pac. J. Public Health 2016, 28, 70S–76S.
- Jung, S.H.; Hwang, J.M.; Kim, C.H. Inversion Table Fall Injury, the Phantom Menace: Three Case Reports on Cervical Spinal Cord Injury. Healthcare 2021, 9, 492.
- Falls. Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 20 May 2021).
- Lamb, S.E.; Jørstad-Stein, E.C.; Hauer, K.; Becker, C.; Prevention of Falls Network Europe and Outcomes Consensus Group. Development of a common outcome data set for fall injury prevention trials: The Prevention of Falls Network Europe consensus. J. Am. Geriatr. Soc. 2005, 53, 1618–1622.
- Drake, S.A.; Conway, S.H.; Yang, Y.; Cheatham, L.S.; Wolf, D.A.; Adams, S.D.; Wade, C.E.; Holcomb, J.B. When falls become fatal—Clinical care sequence. PLoS ONE 2021, 16, e0244862.
- Kistler, B.M.; Khubchandani, J.; Jakubowicz, G.; Wilund, K.; Sosnoff, J. Peer reviewed: Falls and fall-related injuries among US adults aged 65 or older with chronic kidney disease. Prev. Chronic Dis. 2018, 15, E82.
- Barker, E.T.; Howard, A.L.; Villemaire-Krajden, R.; Galambos, N.L. The rise and fall of depressive symptoms and academic stress in two samples of university students. J. Youth Adolesc. 2018, 47, 1252–1266.
- Park, Y.; Paik, N.J.; Kim, K.; Jang, H.; Lim, J. Depressive Symptoms, Falls, and Fear of Falling in Old Korean Adults: The Korean Longitudinal Study on Health and Aging (KLoSHA). J. Frailty Aging 2017, 6, 144–147.
- Zhu, H.; Samtani, S.; Brown, R.; Chen, H. A deep learning approach for recognizing activity of daily living (ADL) for senior care: Exploiting interaction dependency and temporal patterns. Manag. Inf. Syst. Q. 2020, 45, 859–896.
- Saboor, A.; Ahmad, R.; Ahmed, W.; Kiani, A.K.; Moullec, Y.L.; Alam, M.M. On Research Challenges in Hybrid Medium-Access Control Protocols for IEEE 802.15.6 WBANs. IEEE Sens. J. 2019, 19, 8543–8555.
- Saboor, A.; Ahmad, R.; Ahmed, W.; Alam, M.M. A Unique Backoff Algorithm in IEEE 802.15.6 WBAN. In Proceedings of the 2018 IEEE 88th Vehicular Technology Conference (VTC-Fall), Chicago, IL, USA, 27–30 August 2018; pp. 1–5.
- Yu, X. Approaches and principles of fall detection for elderly and patient. In Proceedings of the HealthCom 2008-10th International Conference on e-health Networking, Applications and Services, Singapore, 7–9 July 2008; pp. 42–47.
- Mubashir, M.; Shao, L.; Seed, L. A survey on fall detection: Principles and approaches. Neurocomputing 2013, 100, 144–152.
- Igual, R.; Medrano, C.; Plaza, I. Challenges, issues and trends in fall detection systems. Biomed. Eng. Online 2013, 12, 1–24.
- Del Din, S.; Kirk, C.; Yarnall, A.J.; Rochester, L.; Hausdorff, J.M. Body-Worn Sensors for Remote Monitoring of Parkinson’s Disease Motor Symptoms: Vision, State of the Art, and Challenges Ahead. J. Parkinson’s Dis. 2021, 11, S35–S47.
- Delahoz, Y.S.; Labrador, M.A. Survey on fall detection and fall prevention using wearable and external sensors. Sensors 2014, 14, 19806–19842.
- Saboor, A.; Kask, T.; Kuusik, A.; Alam, M.M.; Le Moullec, Y.; Niazi, I.K.; Zoha, A.; Ahmad, R. Latest Research Trends in Gait Analysis Using Wearable Sensors and Machine Learning: A Systematic Review. IEEE Access 2020, 8, 167830–167864.
- Ren, L.; Peng, Y. Research of Fall Detection and Fall Prevention Technologies: A Systematic Review. IEEE Access 2019, 7, 77702–77722.
- Prakash, C.; Kumar, R.; Mittal, N. Recent developments in human gait research: Parameters, approaches, applications, machine learning techniques, datasets and challenges. Artif. Intell. Rev. 2018, 49, 1–40.
- Alaqtash, M.; Sarkodie-Gyan, T.; Yu, H.; Fuentes, O.; Brower, R.; Abdelgawad, A. Automatic classification of pathological gait patterns using ground reaction forces and machine learning algorithms. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; pp. 453–457.
- Islam, M.M.; Tayan, O.; Islam, M.R.; Islam, M.S.; Nooruddin, S.; Kabir, M.N.; Islam, M.R. Deep Learning Based Systems Developed for Fall Detection: A Review. IEEE Access 2020, 8, 166117–166137.
- Muro-De-La-Herran, A.; Garcia-Zapirain, B.; Mendez-Zorrilla, A. Gait analysis methods: An overview of wearable and non-wearable systems, highlighting clinical applications. Sensors 2014, 14, 3362–3394.
- Rizk, H.; Yamaguchi, H.; Youssef, M.; Higashino, T. Gain without pain: Enabling fingerprinting-based indoor localization using tracking scanners. In Proceedings of the 28th International Conference on Advances in Geographic Information Systems, Seattle, WA, USA, 3–6 November 2020; pp. 550–559.
- Serra, R.; Knittel, D.; Di Croce, P.; Peres, R. Activity recognition with smart polymer floor sensor: Application to human footstep recognition. IEEE Sens. J. 2016, 16, 5757–5775.
- Singh, A.P.; Luhach, A.K.; Gao, X.Z.; Kumar, S.; Roy, D.S. Evolution of wireless sensor network design from technology centric to user centric: An architectural perspective. Int. J. Distrib. Sens. Netw. 2020, 16, 1550147720949138.
- De Miguel, K.; Brunete, A.; Hernando, M.; Gambao, E. Home camera-based fall detection system for the elderly. Sensors 2017, 17, 2864.
- Lou, Z.; Wang, L.; Jiang, K.; Wei, Z.; Shen, G. Reviews of wearable healthcare systems: Materials, devices and system integration. Mater. Sci. Eng. R. Rep. 2020, 140, 100523.
- Niknejad, N.; Ismail, W.B.; Mardani, A.; Liao, H.; Ghani, I. A comprehensive overview of smart wearables: The state of the art literature, recent advances, and future challenges. Eng. Appl. Artif. Intell. 2020, 90, 103529.
- Shahzad, A.; Kim, K. FallDroid: An automated smart-phone-based fall detection system using multiple kernel learning. IEEE Trans. Ind. Inform. 2018, 15, 35–44.
- Khan, M.A.; Saboor, A.; Kim, H.c.; Park, H. A Systematic Review of Location Aware Schemes in the Internet of Things. Sensors 2021, 21, 3228.
- Saboor, A.; Mustafa, A.; Ahmad, R.; Khan, M.A.; Haris, M.; Hameed, R. Evolution of Wireless Standards for Health Monitoring. In Proceedings of the 2019 9th Annual Information Technology, Electromechanical Engineering and Microelectronics Conference (IEMECON), Jaipur, India, 13–15 March 2019; pp. 268–272.
- Hemmatpour, M.; Ferrero, R.; Montrucchio, B.; Rebaudengo, M. A review on fall prediction and prevention system for personal devices: Evaluation and experimental results. Adv. Hum. Comput. Interact. 2019, 2019.
- Kim, T.H.; Choi, A.; Heo, H.M.; Kim, K.; Lee, K.; Mun, J.H. Machine learning-based pre-impact fall detection model to discriminate various types of fall. J. Biomech. Eng. 2019, 141.
- Wang, L.; Xue, Z.; Ezeana, C.F.; Puppala, M.; Chen, S.; Danforth, R.L.; Yu, X.; He, T.; Vassallo, M.L.; Wong, S.T. Preventing inpatient falls with injuries using integrative machine learning prediction: A cohort study. NPJ Digit. Med. 2019, 2, 1–7.
- Salleh, S.M.; mohd yusoff, a.h.; ngadimon, K.; Koh, C.Z. Neural Network Algorithm-based Fall Detection Modelling. Int. J. Integr. Eng. 2020, 12, 138–150.
- Kumar, V.C.; Ha, S.; Sawicki, G.; Liu, C.K. Learning a Control Policy for Fall Prevention on an Assistive Walking Device. In Proceedings of the 2020 IEEE International Conference on Robotics and Automation (ICRA), Paris, France, 31 May–31 August 2020; pp. 4833–4840.
- Sucerquia, A.; López, J.D.; Vargas-Bonilla, J.F. SisFall: A fall and movement dataset. Sensors 2017, 17, 198.
- Martínez-Villaseñor, L.; Ponce, H.; Brieva, J.; Moya-Albor, E.; Núñez-Martínez, J.; Peñafort-Asturiano, C. UP-fall detection dataset: A multimodal approach. Sensors 2019, 19, 1988.
- Caby, B.; Kieffer, S.; de Saint Hubert, M.; Cremer, G.; Macq, B. Feature extraction and selection for objective gait analysis and fall risk assessment by accelerometry. Biomed. Eng. Online 2011, 10, 1–19.
- Shawen, N.; Lonini, L.; Mummidisetty, C.K.; Shparii, I.; Albert, M.V.; Kording, K.; Jayaraman, A. Fall detection in individuals with lower limb amputations using mobile phones: Machine learning enhances robustness for real-world applications. JMIR Mhealth Uhealth 2017, 5, e151.
- Saleh, M.; Jeannès, R.L.B. Elderly fall detection using wearable sensors: A low cost highly accurate algorithm. IEEE Sens. J. 2019, 19, 3156–3164.
- Chen, K.H.; Yang, J.J.; Jaw, F.S. Accelerometer-based fall detection using feature extraction and support vector machine algorithms. Instrum. Sci. Technol. 2016, 44, 333–342.
- Dubois, A.; Mouthon, A.; Sivagnanaselvam, R.S.; Bresciani, J.P. Fast and automatic assessment of fall risk by coupling machine learning algorithms with a depth camera to monitor simple balance tasks. J. Neuroeng. Rehabil. 2019, 16, 1–10.
- Mao, Z.; Wu, L.; Song, L.; Huang, D. Data Preprocessing and Kalman Filter Performance Improvement Method in Integrated Navigation Algorithm. In Proceedings of the 2019 Chinese Control Conference (CCC), Guangzhou, China, 27–30 July 2019; pp. 3416–3422.
- Ajerla, D.; Mahfuz, S.; Zulkernine, F. A real-time patient monitoring framework for fall detection. Wirel. Commun. Mob. Comput. 2019, 2019.
- Zhang, J.; Xiong, Y.; Min, S. A new hybrid filter/wrapper algorithm for feature selection in classification. Anal. Chim. Acta 2019, 1080, 43–54.
- Bommert, A.; Sun, X.; Bischl, B.; Rahnenführer, J.; Lang, M. Benchmark for filter methods for feature selection in high-dimensional classification data. Comput. Stat. Data Anal. 2020, 143, 106839.
