You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 2 by Peter Tang and Version 1 by Amanda Losi.
The COVID-19 pandemic has worked as a catalyst, pushing governments, private companies, and healthcare facilities to design, develop, and adopt innovative solutions to control it, as is often the case when people are driven by necessity. After 18 months since the first case, it is time to think about the pros and cons of such technologies, including artificial intelligence—which is probably the most complex and misunderstood by non-specialists—in order to get the most out of them, and to suggest future improvements and proper adoption.
- artificial intelligence
- new technologies
- pandemic management
- COVID-19
1. Introduction
In December 2019, the new virus SARS-CoV-2, causing the severe acute respiratory syndrome, emerged in China, and rapidly spread around the world with an exponential growth curve.
On 11 March 2020, the World Health Organization declared the outbreak a pandemic, named COVID-19, and, as of 8 June 2021, 173,271,769 total confirmed cases and 3,733,980 deaths had been reported in the world [1,2][1][2].
Before the development of a specific vaccine, many countries took some public health measures to prevent or diminish the possibility of contagion [3]. Currently, environmental measures—such as isolation, quarantine, social distancing, and community containment—and vaccination are the most commonly adopted means that can significantly reduce the effects of the outbreak [4,5][4][5].
The consequences of the COVID-19 pandemic are becoming more evident day after day. As the number of patients is rising, intensive care units (ICUs) are collapsing, while the number of victims is increasing [6,7][6][7]. Recession is damaging the world economy, education has been affected, and psychological distress is surging in the population of all the most affected countries [8,9][8][9]. Furthermore, healthcare systems require more resources to deal with the pandemic, for example, isolation wards for communicable diseases, departments for intensive care, specialized health workers, ventilators, diagnostic imaging devices, medical treatments, and protection devices [10].
In this context, artificial intelligence (AI) and new digital technologies can support institutions, medical staff, and stakeholders by facilitating the timely sharing of medical information and the clinical management of the pandemic, tracking transmission in real time and—perhaps most importantly—remotely monitoring positive patients [11]. Machine learning (ML), a subfield of AI, is increasingly being applied to the medical domain. In ML, computers iteratively learn from data without explicit rule-based programming, identifying patterns to support rational human decision-making [12,13][12][13]. AI and ML were instrumental in COVID-19 drug discovery and vaccine development [14].
2. Current Insights on Artificial Intelligence and COVID-19 Pandemic
The COVID-19 pandemic may be an opportunity to raise awareness on the importance of technological research applied to the medical field. New technologies may be used to spread medical information and knowledge, while physicians can play a role similar to that of influencers during the pandemic (some doctors have become very popular as opinion leaders) [52][15]. It would be interesting to exploit these possibilities, in order to spread healthy habits, disseminate medical culture, improve the understanding of medical decisions, and share the decision-making process [25][16]. The availability of open and big data gives scientists the possibility to perform studies reducing data collection time to a minimum, to assess the impact of new strategies, and to test new instruments to control the outbreak, including new applications. Thanks to a vast amount of data in electronic format, new hypotheses can be tested quickly, while results will be more reliable and significant from a statistical point of view.
Despite the premises and the potentiality of the apps mentioned above, the goal of containing the spread of the infection through tracking apps was only partially achieved. The reason for this is to be identified in the following points.
Countries are designing apps independently, and there are no standard guidelines: these smartphone apps are, in fact, health measures but are being developed without any risk assessment being carried out [21][17].
Each country still actually operates under different protocols, data organization, and legal rules, dispersing the effort to control the pandemic [15][18]. Smartphone users usually turn off Bluetooth when they are not using it, near other phone users, or to save battery charge. COVID-19 apps require users to keep Bluetooth always on, mainly when they are in public places. Due to the reopening of international travels, there is an increased risk of future waves of COVID-19: the international community should start working together to enable data sharing and data transfer between different contact-tracing apps. The isolation of contact-tracing apps will not contain the global spread of infectious diseases: all existing apps from foreign countries should communicate and exchange data [20][19].
The topic of privacy is still a challenge for new health-related technologies. The anonymization of data is a necessary prerequisite [53][20]. However, in the context of apps, we are not talking about “anonymization” of data but about “pseudonymization”: the pseudonymization process allows data to be identified only if combined with other information, stored separately, so it is possible that a subject may still be identified. In order to preserve privacy, a graph of anonymized interpersonal interactions can be adopted, to show transmission vectors of contagion or contact points [54,55][21][22].
Since SARS-CoV-2 is a communicable disease, contact tracing is one of the core strategies to be adopted in order to minimize transmission. New digital technologies can help in monitoring the COVID-19 pandemic and in evaluating exposure risk by means of a geographic information system.
Forwarding recommendations to individuals at risk, pandemics may be contained without the need for mass quarantines (lockdowns) that are detrimental to the society as a whole. By anonymously tracing the movements of confirmed positive subjects, early identification of their contacts becomes feasible. The subsequent steps would be contact isolation and early detection of symptoms.
Respect for privacy is essential in order to apply monitoring systems, such as GPS and smartphone apps, at large. As of 15 October 2020, Immuni® has been downloaded 8 million times, but there is still reluctance to share movements even if anonymously, notwithstanding the fact that such movements and other personal information are shared more or less consciously daily through social media or access to various websites [56,57][23][24]. An online platform, in which every individual is identified by a nickname, may be developed to collect citizens’ health data, such as COVID-19 test results, symptoms, personal movements, etc. On the other hand, every time users download a new app, they give consent to share personal data with the owner of the app. This concept may be applied to health data as well. People should be aware that sharing medical data can lead to a significant improvement in public health, diminishing the risk of contagion and providing important information during an emergency.
In a medical condition such as SARS-CoV-2, ML can forecast a patient’s situation and eventually prevent cardiorespiratory failure, thanks to its predictive capabilities. ML can build a model based on the evolution of the subject’s biomedical parameters and, therefore, improve its predictions above the baseline since adoption.
In the context of a pandemic, where it is necessary to quickly transfer sensitive information about patients enrolled in experimental protocols to monitor the successful outcome of therapies or where it is necessary to transfer rapidly worsening patients from one health facility to another, technology plays a fundamental role. In order for communication between clinicians, from the same hospital or even more so from different hospitals, to be rapid and effective, it is important that the shared information is as essential, objective, and universally validated as possible. An EMR that meets these criteria would not only facilitate the daily work of the healthcare professional who compiles it, but it would also guarantee a quick and clear understanding of the clinical case by any colleague. In a pandemic, time is certainly a fundamental factor. Voice assistance to fill EMR may be an additional element to improve daily work: this “hands-off” or “hands-free” management would save time, especially in emergency or shortage conditions, or when the healthcare facility is saturated with patients.
Technological innovations have costs that are not always sustainable by all countries, especially where there is no basic infrastructure (internet connection, computers, personnel trained to use these resources). Health institutions should consider technology as an investment: even if it has starting costs, these are restored over time, in terms of increased productivity from a qualitative and quantitative point of view (Figure 1).
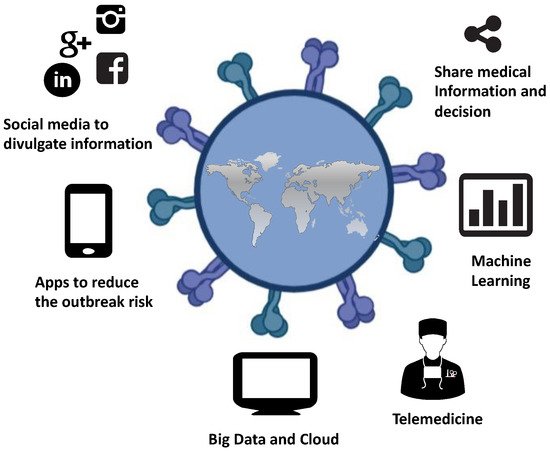
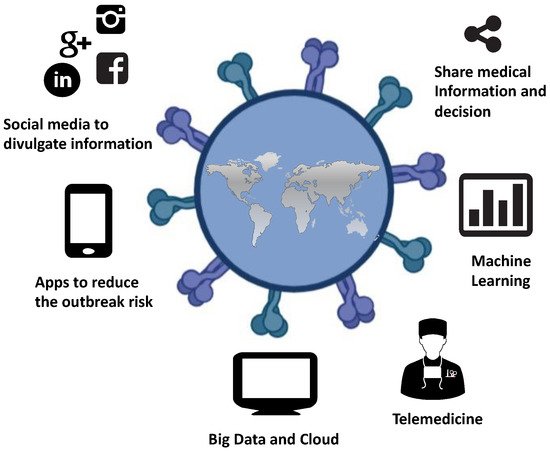
Figure 1. Artificial intelligence and new technologies against the COVID-19 pandemic.
The process of technological innovation in the medical field should be achieved step by step: even small innovations are able to bring great benefits. The technological progress of the countries with the greatest economic resources can play a protective role toward countries with fewer resources, not only blocking the virus in the country in which it is detected but also giving other countries timely information to face the looming threat. Another advantage of technological investments in the COVID-19 emergency is the reduction of lockdown time and of new infections, which translates in terms of a faster economic recovery and reduced healthcare expenses [58][25].
The fact that healthcare facilities could be sources of contagion has drawn attention on new models of care that avoid face-to-face contact between clinicians and patients: there has been particular interest in telemedicine and video consultations. These instruments may be useful for clinicians who are self-isolating, for patients asking about COVID-19, for people with heightened anxiety, for those with symptoms related to SARS-CoV-2 (when a video consultation may reduce the need to visit a potentially contagious patient), and for older or immunosuppressed patients. However, video consultation of patients is unlikely to be appropriate for severely ill individuals, when a full physical examination or procedure cannot be deferred, or when comorbidities affect the patient’s ability to use technology.
The COVID-19 crisis revealed the limitations of our current structures to face a surge of acutely ill patients requiring hospitalization and close monitoring. A technological upgrade of monitoring methods in hospital wards may be part of the solution. In all these respects, telemedicine has proven to be a valuable ally during this pandemic. A unified European and world policy has been lacking in this regard, leaving the solution to the discretion of each country, which is influenced by the sociocultural context and the possible repercussions on public opinion.
There is a need for safety protocols, maintenance personnel, and experts dedicated to the training of health workers. Managing and organizing computerized health data requires specific professional skills: this is the field of the Data Scientist, who should be involved since inception in the data mining life cycle: collection, preparation, exploration, analysis, prediction, prescription, and reporting [32][26].
Clinicians of all specialties, in each country, have faced an unknown disease, adopting therapeutic protocols that they deemed to be suitable to fight the new disease and resorting to drugs and medical devices that were already in their possession. In this climate of uncertainty, the exchange of new diagnostic, instrumental, and therapeutic knowledge between health workers from various countries is of fundamental importance.
AI and new medical technologies are powerful tools that should be closely supervised to make sure that their application to the healthcare field is in accordance with current regulations. These devices are leading the field toward Medicine 2.0. All these instruments are going to take a part in daily clinical practice, and they have the potential to connect the world, making healthcare more inclusive, diffuse, and at the same time tailored to the patients.
New technologies have an essential role in the humanization of hospital care, which consists in not only providing patients with excellent medical care through the appropriate treatment and supportive measures but also discussing the quality, quantity, and type of health care with patients and their family, and in providing emotional and psychological support for patients, families, and staff [59][27].
3. Conclusion
It is now known that hospitalized COVID-19-positive patients must remain isolated from the outside world. Patients can interact only with healthcare professionals. In this era, the interaction with healthcare personnel has become more complicated because of the physical screens placed between healthcare workers and patients, such as masks, sanitary suits, and personal protection devices. Patients have a restricted way of communicating with their relatives and medical staff. Furthermore, all the medical protective devices make healthcare workers indistinguishable. Patients cannot understand whether the people they are talking to are nurses, doctors, or other healthcare personnel, making them feel disoriented and anxious. Despite this, it was possible to adopt some modern and technological solutions to give comfort to patients. A small laptop or smartphone allows communications with the healthcare workers, listening to music therapy sessions, or video-calling or recording a diary (intensive care diaries), or contact between patients and their families outside the intensive care units. During the whole period of hospitalization in intensive care or in COVID-19 wards, relatives received information about their sick family members from the doctors via a phone call, approximately once or twice a day. When patients were intubated, family members could no longer see them until they were discharged. Unfortunately, the high case fatality rate of Coronavirus implied that some families could not see their relatives anymore, after they were admitted to the hospital. The use of electronic devices, such as tablets, and the possibility to make video calls would allow families to talk to and see their sick relatives. Obviously, these tools should also be easy to use for non-IT professionals.
References
- Johns Hopkins Coronavirus Resource Center. COVID-19 Map. Available online: https://coronavirus.jhu.edu/map.html (accessed on 18 June 2021).
- Melegari, G.; Giuliani, E.; Maini, G.; Barbieri, L.; Baffoni, P.; Bertellini, E.; Barbieri, A. Novel coronavirus (2019-nCov): Do you have enough intensive care units? Med. Intensiva 2020, 44, 583–585.
- Wilder-Smith, A.; Freedman, D.O. Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J. Travel Med. 2020, 27, 27.
- Sjödin, H.; Wilder-Smith, A.; Osman, S.; Farooq, Z.; Rocklöv, J. Only strict quarantine measures can curb the coronavirus disease (COVID-19) outbreak in Italy, 2020. Eurosurveillance 2020, 25, 2000280.
- Wilder-Smith, A.; Chiew, C.J.; Lee, V.J. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect. Dis. 2020, 20, e102–e107.
- Musulin, J.; Šegota, S.B.; Štifanić, D.; Lorencin, I.; Anđelić, N.; Šušteršič, T.; Blagojević, A.; Filipović, N.; Ćabov, T.; Markova-Car, E. Application of artificial intelligence-based regression methods in the problem of covid-19 spread prediction: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 4287.
- Anđelić, N.; Šegota, S.B.; Lorencin, I.; Jurilj, Z.; Šušteršič, T.; Blagojević, A.; Protić, A.; Ćabov, T.; Filipović, N.; Car, Z. Estimation of COVID-19 Epidemiology Curve of the United States Using Genetic Programming Algorithm. Int. J. Environ. Res. Public Health 2021, 18, 959.
- Banerjee, D.; Das, D.; Pal, S.; Paul, S.R.; Debnath, A.; Reza, M. Effect of covid-19 on digital transformations in teaching learning methodology and its consequences in society: A review. J. Phys. Conf. Ser. 2021, 1797, 012066.
- Štifanić, D.; Musulin, J.; Miočević, A.; Šegota, S.B.; Šubić, R.; Car, Z. Impact of COVID-19 on Forecasting Stock Prices: An Integration of Stationary Wavelet Transform and Bidirectional Long Short-Term Memory. Complexity 2020, 2020, 12.
- Lorencin, I.; Šegota, S.B.; Anđelić, N.; Blagojević, A.; Šušteršić, T.; Protić, A.; Arsenijević, M.; Ćabov, T.; Filipović, N.; Car, Z. Automatic Evaluation of the Lung Condition of COVID-19 Patients Using X-ray Images and Convolutional Neural Networks. J. Pers. Med. 2021, 11, 28.
- Jiang, L.; Wu, Z.; Xu, X.; Zhan, Y.; Jin, X.; Wang, L.; Qiu, Y. Opportunities and challenges of artificial intelligence in the medical field: Current application, emerging problems, and problem-solving strategies. J. Int. Med. Res. 2021, 49, 1–11.
- Boulos, M.N.K.; Geraghty, E.M. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: How 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int. J. Health Geogr. 2020, 19, 1–12.
- Alimadadi, A.; Aryal, S.; Manandhar, I.; Munroe, P.B.; Joe, B.; Cheng, X. Artificial intelligence and machine learning to fight COVID-19. Physiol. Genom. 2020, 52, 200–202.
- Arshadi, A.K.; Webb, J.; Salem, M.; Cruz, E.; Calad-Thomson, S.; Ghadirian, N.; Collins, J.; Diez-Cecilia, E.; Kelly, B.; Goodarzi, H.; et al. Artificial Intelligence for COVID-19 Drug Discovery and Vaccine Development. Front. Artif. Intell. 2020, 3, 65.
- Kongats, K.; McGetrick, J.A.; Raine, K.D.; Voyer, C.; Nykiforuk, C.I. Assessing general public and policy influencer support for healthy public policies to promote healthy eating at the population level in two Canadian provinces. Public Health Nutr. 2019, 22, 1492–1502.
- Giuliani, E.; Melegari, G.; Carrieri, F.; Barbieri, A. Overview of the main challenges in shared decision making in a multicultural and diverse society in the intensive and critical care setting. J. Eval. Clin. Pract. 2019, 26, 520–523.
- Anonymous. Show evidence that apps for COVID-19 contact-tracing are secure and effective. Nature 2020, 580, 563.
- Ming, L.C.; Untong, N.; Aliudin, N.A.; Osili, N.; Kifli, N.; Tan, C.S.; Goh, K.W.; Ng, P.E.; Al-Worafi, Y.M.; Lee, K.S.; et al. Mobile Health Apps on COVID-19 Launched in the Early Days of the Pandemic: Content Analysis and Review. JMIR mHealth uHealth 2020, 8, e19796.
- Du, L.; Raposo, V.L.; Wang, M. COVID-19 contact tracing apps: A technologic tower of babel and the gap for international pandemic control. JMIR mHealth uHealth 2020, 8, e23194.
- Barbieri, D.; Bigarelli, G. General Data Protection Regulation: A Relational Approach. J. Eur. Am. Intell. Stud. 2018, 53, 25–39.
- Gonçalves-Ferreira, D.; Sousa, M.; Bacelar-Silva, G.M.; Frade, S.; Antunes, L.F.; Beale, T.; Cruz-Correia, R. OpenEHR and General Data Protection Regulation: Evaluation of Principles and Requirements. JMIR Med. Inform. 2019, 7, e9845.
- Cioffi, A.; Lugi, C.; Cecannecchia, C. Apps for COVID-19 contact-tracing: Too many questions and few answers. Ethic. Med. Public Health 2020, 15, 100575.
- Zhang, M.; Chow, A.; Smith, H. COVID-19 Contact-Tracing Apps: Analysis of the Readability of Privacy Policies (Preprint). J. Med. Internet Res. 2020, 22, e21572.
- Bengio, Y.; Ippolito, D.; Janda, R.; Jarvie, M.; Prud’Homme, B.; Rousseau, J.-F.; Sharma, A.; Yu, Y.W. Inherent privacy limitations of decentralized contact tracing apps. J. Am. Med. Inform. Assoc. 2021, 28, 193–195.
- Javaid, M.; Haleem, A.; Vaishya, R.; Bahl, S.; Suman, R.; Vaish, A. Industry 4.0 technologies and their applications in fighting COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 419–422.
- Hofer, I.S.; Burns, M.; Kendale, S.; Wanderer, J.P. Realistically Integrating Machine Learning into Clinical Practice: A road map of opportunities, challenges, and a potential future. Anesth. Analg. 2020, 130, 1115–1118.
- Rivi, V.; Melegari, G.; Blom, J.M. How to humanise the COVID-19 intensive care units. BMJ Evid. Based Med. 2021.
More
