Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Ryszard Pluta and Version 2 by Peter Tang.
In epileptic patients, pharmacological treatment with available anticonvulsants leads to seizure control in <70% of cases. Surgical intervention can lead to control in a selected subset of patients, but still leaves a significant number of patients with uncontrolled seizures. In drug-resistant epilepsy, the ketogenic diet proves to be useful.
- epilepsy
- drug-resistant epilepsy
- ketogenic diet
- therapy
- ketones
- gut microbiota
- side effects
1. Introduction
Epilepsy is a chronic brain disorder that is characterized by recurrent seizures, which are short episodes of involuntary movement that can affect part or all of the body, sometimes accompanied by loss of consciousness and control of bladder or bowel function. Epilepsy is defined as the occurrence of 2 or more unprovoked seizures. A common type of epilepsy affecting 6 in 10 people is idiopathic epilepsy, which means that in over 50% of global cases, the cause of the disease is not identified [1]. Epilepsy of known cause is called secondary or symptomatic epilepsy. Causes of secondary or symptomatic epilepsy are: brain tumors, stroke, brain infection and severe head injury, congenital abnormalities associated with brain defects, brain damage as a result of prenatal or perinatal injuries, and certain genetic syndromes [2]. About 50–70 million people worldwide suffer from epilepsy [2][3][2,3]. It is estimated that 2.4–4.6 million people worldwide are diagnosed with epilepsy each year [3]. These global load estimates are falling more on the populations of low- and middle-income countries, where the cumulative estimate of annual incidence of epilepsy is much higher (139 per 100,000 people) than in high-income countries (49 per 100,000 people) [3]. Regardless of the country’s income, the public health burden of epilepsy carries a high risk of disability, economic loss, social isolation, and premature death [4]. Epilepsy is a serious and costly health problem worldwide and includes estimated indirect and direct costs annually of around EUR 15.5 billion in Europe [4] and USD 15.5 billion in the United States [5]. In this regard, the World Health Organization has made this a priority, calling for the development of national healthcare plans for the treatment of epilepsy, not only to ensure the availability of effective care, but also to prevent its causes. Almost 80–90% of people diagnosed with epilepsy live in low- and middle-income countries [2][6][2,6]. Recent studies in low-, middle-, and high-income countries have shown that up to 70% of adults and children with epilepsy can be successfully treated with antiepileptic drugs. After 2 to 5 years of successful therapy and no seizures, medications can be withdrawn in approximately 70% of children and 60% of adults without recurrence. As the above information shows, available pharmacological treatment for epilepsy has limited effectiveness. Surgical intervention can lead to seizure control in a selected subset of patients, but still leaves a significant number of patients with uncontrolled seizures. The ketogenic diet has proven useful in cases of epilepsy in which pharmacological and/or surgical treatment is not effective as shown below.
2. Classic Epilepsy Therapy
Classic epilepsy treatment includes pharmacological and surgical therapy or vagus nerve stimulation. Despite these therapies, approximately 30% of patients with epilepsy do not have sufficiently controlled seizures and become resistant to drugs [7]. This is defined as insufficient seizure control, despite optimal therapy using a combination of two or more appropriately selected antiepileptic drugs. Under these circumstances, adding next antiepileptic drug often does not significantly reduce seizures. Although epilepsy research is ongoing, the mechanisms of this disease have not been completely elucidated and fully effective therapy for all epilepsy patients has not yet been developed. Epilepsy is the highest research priority for many pharmaceutical companies, which makes epilepsy one of the most studied brain disease in the pharmaceutical industry, but despite such tremendous commitment, we are not seeing significant progress in developing new effective drugs. Patients with drug-resistant epilepsy are addicted to informal care of family and friends as well as healthcare professionals such as social workers, neurologists, and psychologists. Problems associated with drug-resistant epilepsy in children, adolescents, and adults cause repeated hospitalizations of numerous patients. Living with uncontrolled epilepsy has a negative impact on the quality of life of patients with epilepsy and their caregivers.
3. Ketogenic Diet
A ketogenic diet should be considered for patients who have not responded adequately to therapy with two well-selected and well-dosed antiepileptic drugs. Therefore, neurologists often recommend other therapies, such as diet, including ketogenic diet, to provide patients with better antiepileptic control. The ketogenic diet is a last resort treatment for many children, adolescents, and adults with epilepsy resistant to routine medications. It should be recognized that, despite the development of new antiepileptic drugs every year, the treatment, as already mentioned, in about one-third of patients with epilepsy is not fully effective. Ketogenic diet treatment is a non-pharmacological therapy used worldwide, especially for children with epilepsy that is difficult to control. Ketogenic diet has been used in patients with difficult-to-treat epilepsy since 1921, with minor changes in recent years [7]. The ketogenic diet assumes a very high-fat and low-carbohydrate diet, reducing carbohydrate to less as 10% of used energy [8]. This restriction triggers a systemic shift from glucose metabolism toward the metabolism of fatty acids yielding ketone bodies, such as acetoacetate and β-hydroxybutyrate as substrates for energy. The ketogenic diet provides sufficient protein for growth and development. Energy is mostly derived from fat delivered in the diet and by the utilization of body fat. The ketogenic diet is a biochemical model of fasting, which shifts organs to utilize ketone bodies as the source to replace glucose for the brain. The ketogenic diet allows about 90% of the total caloric income from fat and 6% from protein and 4% from carbohydrates. For many refractory epileptic patients, dietary treatment promises to improve the quality of life with a significant decrease in seizure frequency. For this reason, an increase in the global use of the ketogenic diet is currently observed. Successful implementation of this diet depends on the active support of the health care team, the social and educational system, and finally the family. The ketogenic diet requires strict dietary and medical control due to its restrictiveness and side effects [6][7][6,7].
4. Possible Anti-Seizure Mechanisms of the Ketogenic Diet
Although the anticonvulsant mechanisms of ketogenic diet are not still completely understood, it is believed that ketone bodies and polyunsaturated fatty acids presumably play a major role in the anticonvulsant effect of ketogenic diet. During ketogenic diet treatment, body energy is generally generated by the oxidation of fatty acids in mitochondria, resulting in the production of large amounts of acetyl-CoA. Accumulation of acetyl-CoA leads to the synthesis of two ketone bodies mainly in the liver, acetoacetate, and β-hydroxybutyrate, which then enter the blood circulation. Ketone bodies are then used as an alternative source of energy in the brain instead of glucose. After entering the brain, the ketone bodies are transformed into acetyl-CoA and then enter the tricarboxylic acid cycle in the mitochondria of the brain, which ultimately leads to the production of adenosine triphosphate (ATP). Several hypotheses regarding ketone bodies are considered as key mediators involved in the anticonvulsant effect of the ketogenic diet. Based on several studies, potential mechanisms focus essentially on the role of neurotransmitters, brain energy metabolism, oxidative stress, and ion channels, which are briefly discussed below [9][10][23,24] (Figure 1).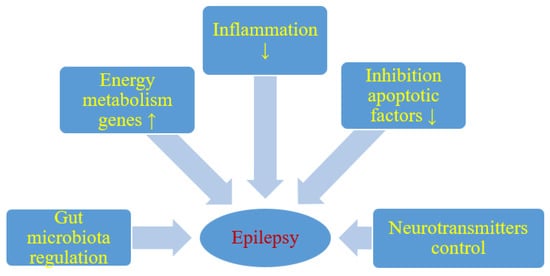
Figure 1. Likely effect of a ketogenic diet on seizure activity. ↑- increase, ↓- decrease.
