Pineal gland neoplasms are tumors with different and variable morphological, histological, and radiological characteristics and, consequently different diagnosis and management. Pineal tumors, are divided into germ cell tumors, pineal parenchymal tumors and tumors that derive from adjacent structures.
- pineal gland
- brain neoplasms
- pineal germ cell tumors
- pineal parenchymal tumor
- pineal metastasis
1. Introduction
Pineal neoplasms are fairly uncommon tumors, and they are predominantly childhood malignancies representing 3–11% of all pediatric brain tumors compared to <1% of brain tumors in adults [1][2][3][4][5][6]. Age, sex, and ethnicity may modulate the relative incidence of pineal neoplasms [7]. Pineal tumors are classified as: germ cell tumors, pineal parenchymal tumors and tumors that derive from adjacent anatomical structures. Germinoma is the most common pineal tumor, representing up to 50% of pineal tumors in Europe, the United States and Japan [1][8][9]. In a series of 370 pineal tumors in patients aged 3–73 years, it was observed that 27% were germinomas; 26% were astrocytomas; 12% were pineoblastomas; 12% were pineocytomas; 4.3% were ependymomas; 4.3% were teratomas; 2.7% were ganglioglioneuromas, lymphomas, meningiomas, metastases, and pineal cysts; 1.6% were mixed embryonal cell tumors (embryonal carcinomas)/malignant teratomas; 1.1% were choriocarcinomas; and 0.54% were oligodendrogliomas [10] (Figure 1).
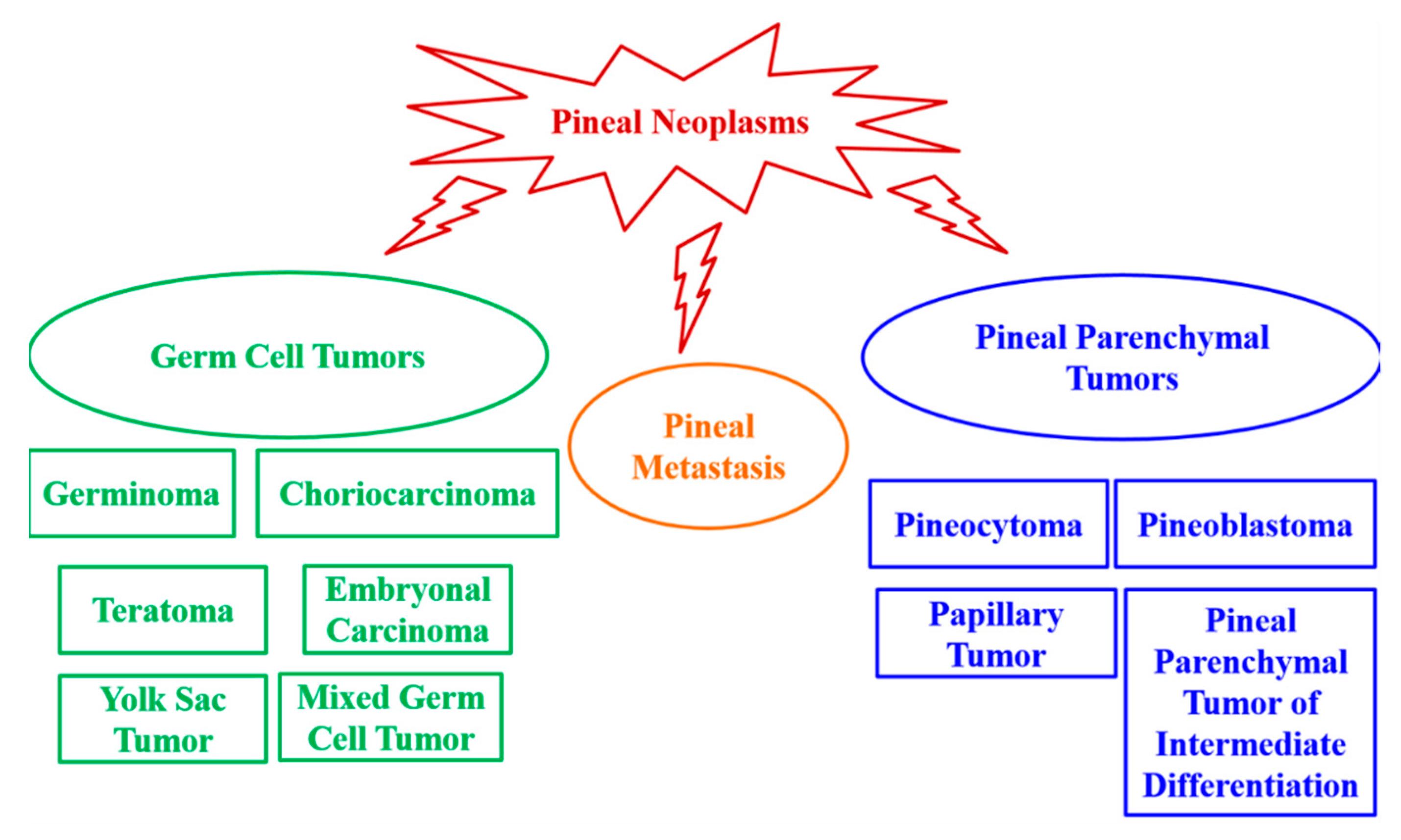
Figure 1. Pineal tumors classification.
Pineal region masses may produce nonspecific signs and symptoms, and they usually cause syndromes of mass effect, including headaches, aqueductal stenosis, and hydrocephalus, or compressive hypothalamic syndromes, such as diabetes insipidus and slowed growth [11][12][13]. A mass in the pineal area may also interfere with the normal function of the pineal gland. Pineal tumors associated with acute and rapidly progressive hydrocephalus may be clinically managed via external ventriculostomy, endoscopic third ventriculostomy, ventriculoperitoneal/ventriculoatrial shunts, or direct removal [14].
It is fundamental to expand advanced imaging techniques, together with both clinical and laboratory knowledge to help to differentiate among the pineal neoplasms and thus realize accurate primary diagnoses and correct treatment and patient management plans. Open surgical resection and stereotactic or endoscopic biopsy are needed for pineal tissue diagnosis [15][16]. However, stereotactic biopsy seems to be associated with a higher risk of hemorrhage in pineal region tumors [4][17]. In practice, the diagnosis of pineal region neoplasms is based on clinical presentation, imaging, and pathology results. Serum and cerebrospinal fluid (CSF) biomarkers complement these standard diagnostic techniques by providing additional data before invasive procedures are performed [1][18][19]. Therefore, research into novel diagnostic markers, therapeutic approaches and follow-up guidelines is fundamental.
In this review, we report the features and clinical relevance of the main pineal gland tumors, underlining the importance of studying the triggering causes of pineal region masses, to enable effective primary diagnosis and, consequently, correct treatment and clinical management.
2. Main Characteristics of Pineal Gland Tumors
As summarized in Table 1, pineal neoplasms are heterogeneous tumors with different histological, morphological, and radiological features and, consequently, different diagnosis and management.
Table 1.
The table summarizes the main characteristics of pineal gland tumors.
| Histological Subtype |
Morphology/Histology | Incidence, Age and Sex Distribution | |
|---|---|---|---|
| Germ Cell Tumors | Germinomas | Not encapsulated tumors with variable proportions of germinoma cellular sheets or lobules composed of a mixture of large multipotential primitive germ cells and smaller cells that resemble lymphocytes. Often presented inflammatory infiltrates. | Most common pineal tumor (>50% of pineal tumors in Europe, the United States, and Japan). Male predominance. |
| Choriocarcinomas | Tumors with stromal vascular channels that form blood lakes and intratumoral hemorrhagic necrosis. | Rare pineal tumor (<5% of all pineal masses). Young men predominance (3–22 years of age). |
|
| Teratomas | Encapsulated tumors with multipotential cells that recapitulate normal organogenesis. (Teratoma may also be unencapsulated). | Second most common pineal tumors. Male predominance. |
|
| Pineal Parenchymal Tumor | Pineocytomas | Unencapsulate tumors with well-differentiated mature cells arranged in sheets. Pineocytic rosettes. |
About 14–30% of all pineal parenchymal tumors. More common in adults (30–60 years old). |
| Pineoblastomas | Undifferentiated or immature pineal cells. | 40% of all pineal parenchymal tumors. Highest incidence in children less of 2 years old. Slightly female predominance. |
|
| Papillary Tumors | Tumors with partially papillary structures lined by slightly polymorphic cells forming ependymal rosettes and pseudorosettes. The rosetted cells had thick processes resting on collagen surrounding the vessels. | Rare pineal parenchymal tumors. | |
| Pineal Parenchymal Tumors of Intermediate Differentiation | Pseudolobulated architecture with multiple cystic components. | Rare pineal parenchymal tumors which may occur in all ages. Slightly female predominance (teenagers and middle-aged women). |
Establishing a means of specific tissue diagnosis for patients with pineal region tumors is needed to distinguish among the variety of possible histomorphological tumor subtypes. In the last decade, specialized surgical and stereotactic techniques have evolved to provide specific, safer, and more effective options for obtaining, at least, correct tissue diagnosis. Advanced microsurgical techniques combined with improved preoperative management and postoperative critical care methods have made surgical resection the optimal therapy for almost all pineal tumors. However, the identification of new therapeutic targets and the development of more effective adjuvant therapies, as well as follow-up guidelines, are needed to improve pineal tumor outcomes.
References
- Carr, C.; O’Neill, B.E.; Hochhalter, C.B.; Strong, M.J.; Ware, M.L. Biomarkers of pineal region tumors: A review. Ochsner J. 2019, 19, 26–31.
- Tamrazi, B.; Nelson, M.; Blüml, S. Pineal region masses in pediatric patients. Neuroimaging Clin. N. Am. 2017, 27, 85–97.
- Louis, D.N.; Ohgaki, H.; Wiestler, O.D.; Cavenee, W.K.; Burger, P.C.; Jouvet, A.; Scheithauer, B.W.; Kleihues, P. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007, 114, 97–109, Erratum in Acta Neuropathol. 2007, 114, 547.
- Abbassy, M.; Aref, K.; Farhoud, A.; Hekal, A. Outcome of single-trajectory rigid endoscopic third ventriculostomy and biopsy in the management algorithm of pineal region tumors: A case series and review of the literature. Childs Nerv. Syst. 2018, 34, 1335–1344.
- Ostrom, Q.T.; Gittleman, H.; Xu, J.; Kromer, C.; Wolinsky, Y.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary brain and other central nervous system tumors diagnosed in the United States in 2009-2013. Neuro Oncol. 2016, 18, v1–v75.
- Schipmann, S.; Keurhorst, D.; Köchling, M.; Schwake, M.; Heß, K.; Sundermann, B.; Stummer, W.; Brentrup, A. Regression of pineal lesions: Spontaneous or iatrogenic? A case report and systematic literature review. World Neurosurg. 2017, 108, 939–947.
- Iorio-Morin, C.; Kano, H.; Huang, M.; Lunsford, L.D.; Simonová, G.; Liscak, R.; Cohen-Inbar, O.; Sheehan, J.; Lee, C.C.; Wu, H.M.; et al. Histology-stratified tumor control and patient survival after stereotactic radiosurgery for pineal region tumors: A report from the International Gamma Knife Research Foundation. World Neurosurg. 2017, 107, 974–982.
- Nomura, K. Epidemiology of germ cell tumors in Asia of pineal region tumor. J. Neurooncol. 2001, 54, 211–217.
- Villano, J.L.; Propp, J.M.; Porter, K.R.; Stewart, A.K.; Valyi-Nagy, T.; Li, X.; Engelhard, H.H.; McCarthy, B.J. Malignant pineal germ-cell tumors: An analysis of cases from three tumor registries. Neuro Oncol. 2008, 10, 121–130.
- Regis, J.; Bouillot, P.; Rouby-Volot, F.; Figarella-Branger, D.; Dufour, H.; Peragut, J.C. Pineal region tumors and the role of stereotactic biopsy: Review of the mortality, morbidity, and diagnostic rates in 370 cases. Neurosurgery 1996, 39, 907–912, discussion 912–914.
- Smirniotopoulos, J.G.; Rushing, E.J.; Mena, H. Pineal region masses: Differential diagnosis. Radiographics 1992, 12, 577–596.
- Wang, K.Y.; Chen, M.M.; Malayil Lincoln, C.M. Adult primary brain neoplasm, including 2016 World Health Organization classification. Neuroimaging Clin. N. Am. 2021, 31, 121–138.
- Seilanian Toosi, F.; Aminzadeh, B.; Faraji Rad, M.; Nekooei, S.; Nahidi, M.; Keykhosravi, E. Pineal and suprasellar germinoma cooccurence with vertebra plana: A case report. Brain Tumor Res. Treat. 2018, 6, 73–77.
- Choque-Velasquez, J.; Resendiz-Nieves, J.; Jahromi, B.R.; Colasanti, R.; Raj, R.; Vehviläinen, J.; Tynninen, O.; Collan, J.; Niemelä, M.; Hernesniemi, J. Extent of resection and long-term survival of pineal region tumors in Helsinki neurosurgery. World Neurosurg. 2019, 131, e379–e391.
- Cho, A.; Cho, S.S.; Buch, V.P.; Buch, L.Y.; Lee, J.Y.K. Second Window Indocyanine Green (SWIG) near infrared fluorescent transventricular biopsy of pineal tumor. World Neurosurg. 2020, 134, 196–200.
- Mathieu, D.; Iorio-Morin, C. Stereotactic radiosurgery for pineal region tumors. Prog. Neurol. Surg. 2019, 34, 173–183.
- Field, M.; Witham, T.F.; Flickinger, J.C.; Kondziolka, D.; Lunsford, L.D. Comprehensive assessment of hemorrhage risks and outcomes after stereotactic brain biopsy. J. Neurosurg. 2001, 94, 545–551.
- Mayol Del Valle, M.; De Jesus, O. Pineal gland cancer. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020.
- Chiba, K.; Aihara, Y.; Komori, T.; Kawamata, T. Placental alkaline phosphatase in cerebrospinal fluid as a biomarker for optimizing surgical treatment strategies for pineal region germ cell tumors. Brain Tumor Pathol. 2020, 37, 60–68.
