Heart failure (HF) remains a leading cause of morbidity, hospitalization, and mortality worldwide. Advancement of mechanical circulatory support technology has led to the use of continuous-flow left ventricular assist devices (LVADs), reducing hospitalizations, and improving quality of life and outcomes in advanced HF. Recent studies have highlighted how metabolic and endocrine dysfunction may be a consequence of, or associated with, HF, and may represent a novel (still neglected) therapeutic target in the treatment of HF. On the other hand, it is not clear whether LVAD support, may impact the outcome by also improving organ perfusion as well as improving the neuro-hormonal state of the patients, reducing the endocrine dysfunction. Moreover, endocrine function is likely a major determinant of human homeostasis, and is a key issue in the recovery from critical illness. Care of the endocrine function may contribute to improving cardiac contractility, immune function, as well as infection control, and rehabilitation during and after a LVAD placement.
- ventricular assist devices
- VAD
- heart failure
- TSH
- infections
- anemia
- erythropoietin
1. Thyroid Dysfunction
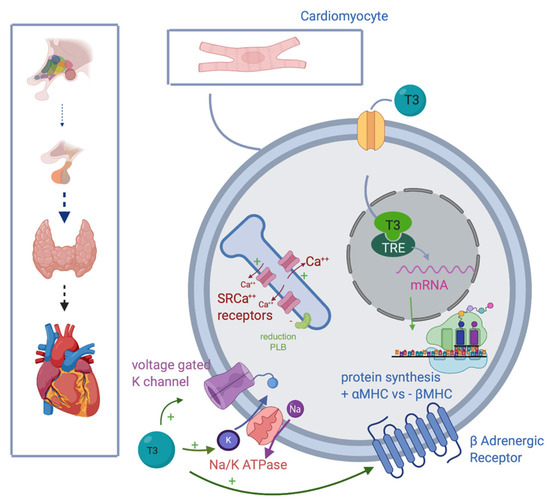
1.1. Effects of Thyroid Hormones on Cardiac Function
- -
-
Promoting synthesis of the α isoforms of the myosin heavy chain (faster contractility), and reducing β isoform (slow contractility), enhancing systolic function.
- -
-
Upregulating β1 receptors, improving adrenergic responsiveness.
- -
- -
-
Inducing sarcoendoplasmic reticulum (SR) Ca(2+) receptors SERCA2a and down-regulation of phospholamban ATPase.
- -
-
Acting on the sinoatrial node, T3 can also improve heart rate.
1.2. Considerations after LVAD Implant and Potential Implications for Supplementation
2. Vitamin D Deficiency and Supplementation
2.1. Effects on Cardiac Function
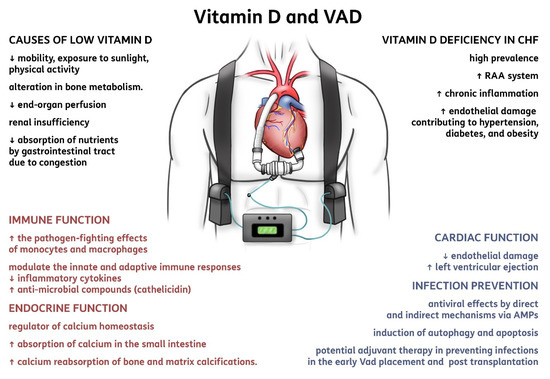
2.2. Considerations after LVAD Implant and Potential Implications for Supplementation
3. Erythropoiesis-Stimulating Agents and Iron Supplementation
3.1. Targeting Iron Deficiency and Anemia in Heart Failure
3.2. Considerations after LVAD Implant and Potential Implications for Supplementation
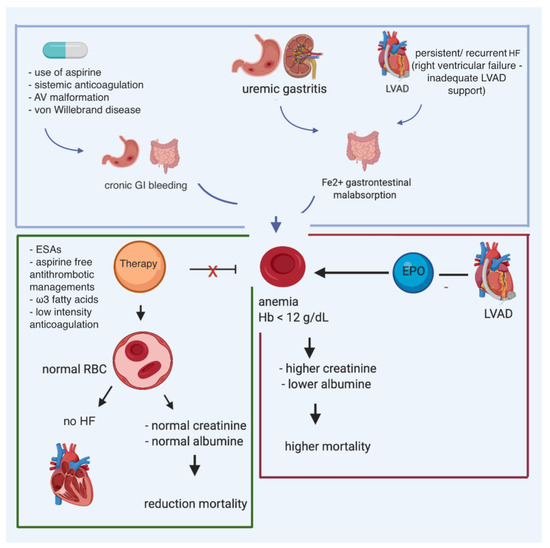
- -
-
Preoperative anemic patients who are on IV anticoagulants, with the target of perioperative reduction of PRBC transfusions.
- -
-
Postoperative use started only when therapeutic anticoagulation is reached.
- -
-
During LVAD support in patients who require transfusions, and are still symptomatic, with renal failure and/or RVF.
References
- Kannan, L.; Shaw, P.A.; Morley, M.P.; Brandimarto, J.; Fang, J.C.; Sweitzer, N.K.; Cappola, T.P.; Cappola, A.R. Thyroid Dysfunction in Heart Failure and Cardiovascular Outcomes. Circ. Heart Fail. 2018, 11, e005266.
- Osuna, P.M.; Udovcic, M.; Sharma, M.D. Hyperthyroidism and the Heart. Methodist DeBakey Cardiovasc. J. 2017, 13, 60–63.
- Klein, I.; Danzi, S. Thyroid Disease and the Heart. Circulation 2007, 116, 1725–1735.
- Ito, K.; Kagaya, Y.; Shimokawa, H. Thyroid hormone and chronically unloaded hearts. Vasc. Pharmacol. 2010, 52, 138–141.
- Letsou, G.V.; Reverdin, S.; Frazier, O. Thyrotoxicosis-facilitated bridge to recovery with a continuous-flow left ventricular assist device. Eur. J. Cardio Thorac. Surg. 2013, 44, 573–574.
- Dipla, K.; Mattiello, J.A.; Jeevanandam, V.; Houser, S.R.; Margulies, K.B. Myocyte Recovery After Mechanical Circulatory Support in Humans With End-Stage Heart Failure. Circulation 1998, 97, 2316–2322.
- Pantos, C.; Xinaris, C.; Mourouzis, I.; Malliopoulou, V.; Kardami, E.; Cokkinos, D.V. Thyroid hormone changes cardiomyocyte shape and geometry via ERK signaling pathway: Potential therapeutic implications in reversing cardiac remodeling? Mol. Cell. Biochem. 2006, 297, 65–72.
- Pantos, C.; Mourouzis, I.; Galanopoulos, G.; Gavra, M.; Perimenis, P.; Spanou, D.; Cokkinos, D.V. Thyroid Hormone Receptor α1 Downregulation in Postischemic Heart Failure Progression: The Potential Role of Tissue Hypothyroidism. Horm. Metab. Res. 2010, 42, 718–724.
- Pantos, C.; Mourouzis, I.; Cokkinos, D.V. Thyroid hormone and cardiac repair/regeneration: From Prometheus myth to reality? Can. J. Physiol. Pharmacol. 2012, 90, 977–987.
- Nguyen, A.B.; Imamura, T.; Besser, S.; Rodgers, D.; Chung, B.; Raikhelkar, J.; Kalantari, S.; Smith, B.; Sarswat, N.; Labuhn, C.; et al. Metabolic Dysfunction in Continuous-Flow Left Ventricular Assist Devices Patients and Outcomes. J. Am. Heart Assoc. 2019, 8, e013278.
- Zittermann, A.; Sabatschus, O.; Jantzen, S.; Platen, P.; Danz, A.; Dimitriou, T.; Scheld, K.; Klein, K.; Stehle, P. Exercise-trained young men have higher calcium absorption rates and plasma calcitriol levels compared with age-matched sedentary controls. Calcif. Tissue Int. 2000, 67, 215–219.
- Zheng, S.; Yang, J.; Hu, X.; Li, M.; Wang, Q.; Dancer, R.C.; Parekh, D.; Gao-Smith, F.; Thickett, D.R.; Jin, S. Vitamin D attenuates lung injury via stimulating epithelial repair, reducing epithelial cell apoptosis and inhibits TGF-β induced epithelial to mesenchymal transition. Biochem. Pharmacol. 2020, 177, 113955.
- Martínez-Moreno, J.; Hernandez, J.C.; Urcuqui-Inchima, S. Effect of high doses of vitamin D supplementation on dengue virus replication, Toll-like receptor expression, and cytokine profiles on dendritic cells. Mol. Cell. Biochem. 2019, 464, 169–180.
- Ayelign, B.; Workneh, M.; Molla, M.D.; Dessie, G. Role Of Vitamin-D Supplementation In TB/HIV Co-Infected Patients. Infect. Drug Resist. 2020, 13, 111–118.
- Amrein, K.; Scherkl, M.; Hoffmann, M.; Neuwersch-Sommeregger, S.; Köstenberger, M.; Berisha, A.T.; Martucci, G.; Pilz, S.; Malle, O. Vitamin D deficiency 2.0: An update on the current status worldwide. Eur. J. Clin. Nutr. 2020, 74, 1498–1513.
- Amrein, K.; Martucci, G.; McNally, J.D. When not to use meta-analysis: Analysing the meta-analyses on vitamin D in critical care. Clin. Nutr. 2017, 36, 1729–1730.
- Amrein, K.; Schnedl, C.; Holl, A.; Riedl, R.; Christopher, K.B.; Pachler, C.; Purkart, T.U.; Waltensdorfer, A.; Munch, A.; Warnkross, H.; et al. Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: The VITdAL-ICU randomized clinical trial. JAMA 2014, 312, 1520–1530.
- Liu, N.; Su, H.; Zhang, Y.; Kong, J. The protective effect of 1,25(OH)2D3 against cardiac hypertrophy is mediated by the cyclin-dependent kinase inhibitor p21. Eur. J. Pharmacol. 2020, 888, 173510.
- Zittermann, A.; Ernst, J. Calciotropic and phosphaturic hormones in heart failure. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 971–979.
- Terrovitis, J.; Zotos, P.; Kaldara, E.; Diakos, N.; Tseliou, E.; Vakrou, S.; Kapelios, C.; Chalazonitis, A.; Nanas, S.; Toumanidis, S.; et al. Bone mass loss in chronic heart failure is associated with secondary hyperparathyroidism and has prognostic significance. Eur. J. Heart Fail. 2012, 14, 326–332.
- Ney, J.; Heyland, D.K.; Amrein, K.; Marx, G.; Grottke, O.; Choudrakis, M.; Autschbach, T.; Hill, A.; Meybohm, P.; Benstoem, C.; et al. The relevance of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D concentration for postoperative infections and postoperative organ dysfunctions in cardiac surgery patients: The eVIDenCe study. Clin. Nutr. 2019, 38, 2756–2762.
- Wu, C.; Kato, T.S.; Pronschinske, K.; Qiu, S.; Naka, Y.; Takayama, H.; Schulze-Späte, U.; Cremers, S.; Shane, E.; Mancini, D.; et al. Dynamics of bone turnover markers in patients with heart failure and following haemodynamic improvement through ventricular assist device implantation. Eur. J. Heart Fail. 2012, 14, 1356–1365.
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, Treatment, and Prevention of Vitamin D Deficiency: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930.
- Cashman, K.D. Vitamin D Deficiency: Defining, Prevalence, Causes, and Strategies of Addressing. Calcif. Tissue Int. 2020, 106, 14–29.
- Cariolou, M.; Cupp, M.A.; Evangelou, E.; Tzoulaki, I.; Berlanga-Taylor, A.J. Importance of vitamin D in acute and critically ill children with subgroup analyses of sepsis and respiratory tract infections: A systematic review and meta-analysis. BMJ Open 2019, 9, e027666.
- Lee, P.; Nair, P.; Eisman, J.A.; Center, J.R. Vitamin D deficiency in the intensive care unit: An invisible accomplice to morbidity and mortality? Intensiv. Care Med. 2009, 35, 2028–2032.
- Martucci, G.; McNally, D.; Parekh, D.; Zajic, P.; Tuzzolino, F.; Arcadipane, A.; Christopher, K.B.; Dobnig, H.; Amrein, K. Trying to identify who may benefit most from future vitamin D intervention trials: A post hoc analysis from the VITDAL-ICU study excluding the early deaths. Crit. Care 2019, 23, 200.
- Zittermann, A.; Ernst, J.B.; Pilz, S.; Dreier, J.; Kuhn, J.; Knabbe, C.; Gummert, J.F.; Morshuis, M.; Milting, H. Calciotropic and Phosphaturic Hormones in End-Stage Heart Failure Patients Supported by a Left-Ventricular Assist Device. PLoS ONE 2016, 11, e0164459.
- Zittermann, A.; Ernst, J.B.; Prokop, S.; Fuchs, U.; Dreier, J.; Kuhn, J.; Berthold, H.K.; Pilz, S.; Gouni-Berthold, I.; Gummert, J.F. Vitamin D supplementation and bone turnover in advanced heart failure: The EVITA trial. Osteoporos. Int. 2017, 29, 579–586.
- De Haan, K.; Groeneveld, A.B.; de Geus, H.R.; Egal, M.; Struijs, A. Vitamin D deficiency as a risk factor for infection, sepsis and mortality in the critically ill: Systematic review and meta-analysis. Crit. Care 2014, 18, 1–8.
- Martucci, G.; Volpes, R.; Panarello, G.; Tuzzolino, F.; Di Carlo, D.; Ricotta, C.; Gruttadauria, S.; Conaldi, P.G.; Luca, A.; Amrein, K.; et al. Vitamin D Levels in Liver Transplantation Recipients and Early Postoperative Outcomes: Prospective Observational DLiverX Study. Clin. Nutr. 2020.
- Nakamura, K.; Kageyama, S.; Kupiec-Weglinski, J.W. Innate immunity in ischemia-reperfusion injury and graft rejection. Curr. Opin. Organ. Transplant. 2019, 24, 687–693.
- Ochando, J.; Ordikhani, F.; Boros, P.; Jordan, S. The innate immune response to allotransplants: Mechanisms and therapeutic potentials. Cell. Mol. Immunol. 2019, 16, 350–356.
- Amrein, K.; Papinutti, A.; Mathew, E.; Vila, G.; Parekh, D. Vitamin D and critical illness: What endocrinology can learn from intensive care and vice versa. Endocr. Connect. 2018, 7, R304–R315.
- Del Valle, H.B.; Yaktine, A.L.; Taylor, C.L.; Ross, A.C. Dietary Reference Intakes for Calcium and Vitamin D; The National Academies Press: Washington, DC, USA, 2011.
- Heaney, R.P.; Davies, K.M.; Chen, T.C.; Holick, M.F.; Barger-Lux, M.J. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am. J. Clin. Nutr. 2003, 77, 204–210.
- Hathcock, J.N.; Shao, A.; Vieth, R.; Heaney, R. Risk assessment for vitamin D. Am. J. Clin. Nutr. 2007, 85, 6–18.
- Pfeifer, M.; Begerow, B.; Minne, H.W.; Abrams, C.; Nachtigall, D.; Hansen, C. Effects of a Short-Term Vitamin D and Calcium Supplementation on Body Sway and Secondary Hyperparathyroidism in Elderly Women. J. Bone Mineral Res. 2000, 15, 1113–1118.
- Ross, A.C.; Manson, J.E.; Abrams, S.A.; Aloia, J.F.; Brannon, P.M.; Clinton, S.K.; Durazo-Arvizu, R.A.; Gallagher, J.C.; Gallo, R.L.; Jones, G.; et al. The 2011 Report on Dietary Reference Intakes for Calcium and Vitamin D from the Institute of Medicine: What Clinicians Need to Know. J. Clin. Endocrinol. Metab. 2011, 96, 53–58.
- EFSA Panel on Dietetic Products, Nutrition and Allergies. Scientific Opinion on the Tolerable Upper Intake Level of vitamin D. EFSA J. 2012, 10, 2813.
- Klip, I.T.; Comin-Colet, J.; Voors, A.A.; Ponikowski, P.; Enjuanes, C.; Banasiak, W.; Lok, D.J.; Rosentryt, P.; Torrens, A.; Polonski, L.; et al. Iron deficiency in chronic heart failure: An international pooled analysis. Am. Heart J. 2013, 165, 575–582.e3.
- Qian, C.; Wei, B.; Ding, J.; Wu, H.; Wang, Y. The Efficacy and Safety of Iron Supplementation in Patients With Heart Failure and Iron Deficiency: A Systematic Review and Meta-analysis. Can. J. Cardiol. 2016, 32, 151–159.
- Anker, S.D.; Kirwan, B.-A.; Van Veldhuisen, D.J.; Filippatos, G.; Comin-Colet, J.; Ruschitzka, F.; Lüscher, T.F.; Arutyunov, G.P.; Motro, M.; Mori, C.; et al. Effects of ferric carboxymaltose on hospitalisations and mortality rates in iron-deficient heart failure patients: An individual patient data meta-analysis. Eur. J. Heart Fail. 2017, 20, 125–133.
- Levi, S.; Rovida, E. The role of iron in mitochondrial function. Biochim. Biophys. Acta Gen. Subj. 2009, 1790, 629–636.
- Hoes, M.F.; Beverborg, N.G.; Kijlstra, J.D.; Kuipers, J.; Swinkels, D.W.; Giepmans, B.N.; Rodenburg, R.J.; Van Veldhuisen, D.J.; De Boer, R.A.; Van Der Meer, P. Iron deficiency impairs contractility of human cardiomyocytes through decreased mitochondrial function. Eur. J. Heart Fail. 2018, 20, 910–919.
- Mordi, I.R.; Tee, A.; Lang, C.C. Iron Therapy in Heart Failure: Ready for Primetime? Card. Fail. Rev. 2018, 4, 28–32.
- Cleland, J.G.F.; Zhang, J.; Pellicori, P.; Dicken, B.; Dierckx, R.; Shoaib, A.; Wong, K.; Rigby, A.; Goode, K.; Clark, A.L. Prevalence and Outcomes of Anemia and Hematinic Deficiencies in Patients With Chronic Heart Failure. JAMA Cardiol. 2016, 1, 539–547.
- Klip, I.T.; Jankowska, E.A.; Enjuanes, C.; Voors, A.A.; Banasiak, W.; Bruguera, J.; Rozentryt, P.; Polonski, L.; Van Veldhuisen, D.J.; Ponikowski, P.; et al. The additive burden of iron deficiency in the cardiorenal-anaemia axis: Scope of a problem and its consequences. Eur. J. Heart Fail. 2014, 16, 655–662.
- Martens, P.; Nijst, P.; Verbrugge, F.H.; Smeets, K.; Dupont, M.; Mullens, W. Impact of iron deficiency on exercise capacity and outcome in heart failure with reduced, mid-range and preserved ejection fraction. Acta Cardiol. 2017, 73, 115–123.
- Nanas, J.N.; Matsouka, C.; Karageorgopoulos, D.; Leonti, A.; Tsolakis, E.; Drakos, S.G.; Tsagalou, E.P.; Maroulidis, G.D.; Alexopoulos, G.P.; Kanakakis, J.E.; et al. Etiology of Anemia in Patients With Advanced Heart Failure. J. Am. Coll. Cardiol. 2006, 48, 2485–2489.
- Jankowska, E.A.; Rozentryt, P.; Witkowska, A.; Nowak, J.; Hartmann, O.; Ponikowska, B.; Borodulin-Nadzieja, L.; Banasiak, W.; Polonski, L.; Filippatos, G.; et al. Iron deficiency: An ominous sign in patients with systolic chronic heart failure. Eur. Heart J. 2010, 31, 1872–1880.
- Jelani, Q.-U.-A.; Attanasio, P.; Katz, S.D.; Anker, S.D. Treatment with Iron of Patients with Heart Failure With and Without Anemia. Heart Fail. Clin. 2010, 6, 305–312.
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200.
- Swedberg, K.; Young, J.B.; Anand, I.S.; Cheng, S.; Desai, A.S.; Diaz, R.; Maggioni, A.P.; McMurray, J.J.V.; O’Connor, C.; Pfeffer, M.A.; et al. Treatment of Anemia with Darbepoetin Alfa in Systolic Heart Failure. N. Engl. J. Med. 2013, 368, 1210–1219.
- Mix, T.-C.H.; Brenner, R.M.; Cooper, M.E.; De Zeeuw, D.; Ivanovich, P.; Levey, A.S.; McGill, J.B.; McMurray, J.J.; Parfrey, P.S.; Parving, H.-H.; et al. Rationale—Trial to Reduce Cardiovascular Events with Aranesp Therapy (TREAT): Evolving the management of cardiovascular risk in patients with chronic kidney disease. Am. Heart J. 2005, 149, 408–413.
- Vrtovec, B.; Radovancevic, R.; Delgado, R.M.; Radovancevic, B.; Bracey, A.W.; Gregoric, I.D.; Frazier, O. Significance of anaemia in patients with advanced heart failure receiving long-term mechanical circulatory support. Eur. J. Heart Fail. 2009, 11, 1000–1004.
- Nassif, M.E.; Patel, J.S.; Shuster, J.E.; Raymer, D.S.; Jackups, R.; Novak, E.; Gage, B.F.; Prasad, S.; Silvestry, S.C.; Ewald, G.A.; et al. Clinical Outcomes With Use of Erythropoiesis Stimulating Agents in Patients With the HeartMate II Left Ventricular Assist Device. JACC Heart Fail. 2015, 3, 146–153.
