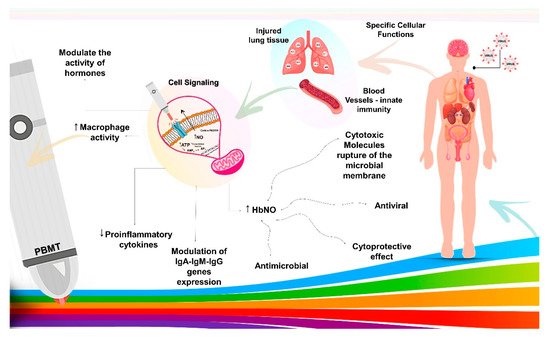
The schematic diagram illustrates COVID-19 infection in the human body, followed by rapid spread from viral sanctuary sites. Early innate host immune response dictates viral load at the acute phase. Photobiomodulation therapy (PBMT) acts on transmembrane receptors present in the mitochondria with specific cellular functions, modulating cells with functional deficits, such as blood cells and lung tissue, promoting signaling by the absorptivities of electromagnetic rays. These chromophores convert electromagnetic energy into adenosine triphosphate, and then induce increased macrophage activity, modulation of plasma hormone levels, decreased proinflammatory cytokines, modulated expression of IgA, IgM, and IgG immunoglobulins, and increase of the HbNO synthesis. The results are positive with the synthesis of cytotoxic molecules to microbial membranes, which leads to the destruction of microorganisms of all types in the blood and cytoprotective effect to human cells.
Since the onset of the disease, there is a consensus among clinicians and researchers about the role of the SARS-CoV-2 virus in pulmonary complications, which can lead to a severe respiratory syndrome. Nitric oxide (NO) is beneficial in low concentrations, but it can produce reactive nitrogen species (RNS), such as peroxynitrite, in high concentrations. Both ROS (species that react to oxygen) and RNS are destructive at high doses. In pulmonary inflammation, the increased influx of neutrophils produces high levels of ROS and RNS, damaging the lung tissue (Figure 2). PBMT can reduce ROS formation [
42,
43], reduce pulmonary edema, neutrophil influx, and promote lung tissue regeneration and better oxygenation to all related organs [
44].
As for the type of laser, infrared is preferred due to the greater capacity of penetrating the lung tissue [
45]. The dosimetry of adequate energy density is 9.5–10.5 J/cm
2. Continuous irradiation at different points in the respiratory system can be helpful in the treatment of COVID-19 pneumonia. PBMT can be used as a preventive approach in high-risk, elderly, or comorbid patients receiving pre-treatment PBMT while still at an early stage of the disease [
40]. In addition, PBMT can be considered a therapeutic approach in hospitalized patients before their condition worsens enough to require ICU admission [
44].
Moreover, in addition to the damage to lung tissues, SARS-CoV-2 also favors the formation of thrombi. Nitric oxide has the potential to treat thrombosis associated with mechanical devices due to its ability to reduce platelet activation and due to the central role of platelet adhesion in device thrombosis [
28]. One study, shown in Table 1, reports the effects of nitrite, distant red light, and their combination in various measures of blood clotting using a variety of agonists. The authors concluded that the combination of extreme red light and nitrite treatment decreased the coagulation measures in all cases [
28]. It is believed that the radiation from the infrared laser near the red (R/NIR) can stabilize the membrane of red blood cells (RBC) by increasing its resistance to destructive factors, reducing trauma in the use of equipment, such as extracorporeal circulation [
41].
Likewise, there are techniques for increasing the efficiency of light, such as PDT, since its penetration into tissues is limited. One technique is the association of PDT with phototherapy agents, which sensitize specific molecules to absorb light better. PDT has been clinically validated in several esophageal pathologies and some lung cancers and can be used to destroy pathogenic microorganisms such as bacteria and viruses [
29,
46]. This can also be seen in the association of PDT with Phthalocyanines, a phototherapeutic agent that makes incorporation by target cells easier. The use of phototherapeutic agent Phthalomethyl D shows promising effects if used with the aim of leading to immunological improvement, cure, and repair against viral induction [
32].
In this scenario, with the use of PDT by the ILIB technique through radial artery for 30 min at a wavelength of 660–460 nm, 100 mW output power, and in continuous wave mode for point irradiation (Ecco Fibras, São Paulo, SP, Brazil) and the use of Phthalomethyl D administered orally or introduced into the digestive tract, wound healing and the systemic inflammatory process were improved. It can be suggested that, at low doses, phagocytic activity increases, and cell viability decreases after the execution of this technique. Thus, the relationship between the action of the laser and the activation of monocytic cells may explain the process of resolving systemic inflammation with more efficient wound closure. Thus, its contribution to the anti-inflammatory response during viral infection may be an approach to SARS-CoV-2 [
32].
Clinical study using PDT in 300 patients, methylene blue (MB) photosensitizer and 660 nm red light applied in the oral and nasal cavity, compared to placebos, led to significant decreases in morbidity and reduced mortality rates, contributing to the immune response [
47]. In vitro, PDT with MB and Radachlorin, using continuous laser with wavelength 662 nm at doses of 16 J/cm
2 and 40 J/cm
2 of laser irradiation, shows high antiviral activity against SARS-CoV-2 [
48].
Furthermore, COVID-19 mainly attacks the lung and heart tissues. This is because the coronavirus binds to the cell through the angiotensin-converting receptor, which is highly expressed in lung and heart cells. Thus, it is vital that the receptor is not available to bind to the coronavirus, and for that, Vitamin D, which also binds to that receptor, can help. There are no acute cases of heart attack at balanced levels of Vitamin D due to COVID-19 [
31]. In addition, Vitamin D has a broad spectrum of immunomodulatory, antifibrotic, anti-inflammatory and antioxidant actions [
9,
49].
One of the safest ways to increase Vitamin D levels in the body is the use of the 50 mW 589 nm yellow laser, which can be applied through the nose or acupuncture points (acupuncture laser) [
31]. In addition, Vitamin D deficiency has been found, to be related to increased mortality and disease progression. It was also observed that the expression of inflammatory cytokines was inhibited by Vitamin D, and its insufficiency was related to the overexpression of cytokines and that it plays an important role in cardiovascular diseases and diabetes mellitus, risk factors for the disease [
45]. Therefore, ways to obtain good Vitamin D levels in the body can be a preventive approach to complications of COVID-19 [
31,
49].
In severe SARS-CoV-2 infections, recent histopathological studies have emphasized the important role of Endothelial Cells (EC) in immune-thrombosis, vascular dysfunction, and inflammation. The storm of pro-inflammatory cytokines, commonly seen in irregular immune responses, can also cause endothelial dysfunction (EnD). The endothelitis caused by COVID-19 can explain the impairment of the systemic microcirculatory function of different organs and is highly harmful [
50]. The endothelium performs multiple functions, such as regulating the transport of biologically active substances, barrier, participation in phagocytosis, and control of the diffusion of fluids, electrolytes, metabolic products, and platelet adhesion. Therefore, EnD can be catastrophic, becoming a primary cause of high mortality and the development of diseases or complications that disrupt a fully human life, so preventing the development of EnD is paramount [
37,
50].
Thus, with LLLT, at the systemic level, it is possible to activate microcirculation and metabolism, better regeneration of lung tissue, increased local immunity, and improved muscle support for the respiratory act. As a result, laser illumination using the ILIB technique has been widely used to correct endothelial function. The “classic” way of using this method is with a wavelength of 635 nm, 2–3 mW of lighting power at the fiber outlet, 10–20 min of exposure. With this technique, in seven daily sessions, patients with mild illness (six people) achieved an overall improvement in health, relief of chest pain during cough, and improvement in sputum discharge due to the increased effectiveness of the cough impulse [
37,
51].
One patient, with a severe disease course, used five combined laser therapy procedures: ILBI-525 intravenous laser blood illumination + LUVBITM violet laser ultra-blood illumination (525 nm wavelength, green spectrum, 2 mW lighting power, 5 min exposure per zone + 365 nm wavelength, UV spectrum, 2 mW of illumination and 5 min exposure per zone on alternate days) and exposure to pulsed IR LLLT (904 nm wavelength with light pulse duration of 100 ns, pulsed power of 15 W, power density of 10–15 W/cm
2, frequency of 80 Hz and 1.5 min of exposure). With this approach, in the fifth procedure, the patient noticed a significant improvement in general health and the disappearance of shortness of breath with moderate physical effort [
37,
51,
52].
Knowing that LLLT is effective against the cytokine storm and ARDS, promoting tissue healing and regeneration, experimental models in animals have shown a decrease in inflammation without impairing lung function in the case of acute lung injuries, which could be an approach to pulmonary inflammatory diseases [
25]. In this experimental study, the effect of LLLT on chronic obstructive pulmonary disease was evaluated. The results demonstrated that LLLT significantly reduced the number of inflammatory cells and the secretion of pro-inflammatory cytokines as IL-1 β, IL-6, and TNF-α in bronchoalveolar lavage (BAL). It was also observed that LLLT decreased collagen deposition and the expression of the purinergic P2X7 receptor. Thus, LLLT is considered a promising treatment for other lung diseases, such as COVID-19 [
25].
In addition, prolonged time on ventilators causes lung injuries, which can further aggravate the disease. For this, the use of LLLT is shown to minimize this side effect. This was proven in experimental models of ventilator-induced lung injury in rats, and with the use of LLLT there was an anti-inflammatory effect via decreased lung injury scores and lower neutrophil counts in alveoli, interstitial, and bronchial lavage [
42]. Modulation of inflammatory factors and a drive for healing are needed to help patients get off the ventilators. Thus, LLLT is a safe and non-invasive technique that has been used for decades in the treatment of pain, wound healing, and health conditions, including diseases of the respiratory system. LLLT combined with standard medical care to optimize response to treatments, reduce inflammation, promote healing, and speed recovery times is a promising approach [
33].
Another technique that can be useful in this scenario is PBMT when used alone or combined with the static magnetic field (PBMT-sMF). In a study, with patients with severe COVID-19 that required mechanical ventilation were randomly assigned to receive PBMT-sMF (six sites on the lower chest—189 J in total and two sites in the neck area—63 J in total) or PBMT-sMF placebo daily for the entire ICU stay, it was noted that PBMT-sMF was able to improve some ventilatory parameters, in addition to the infectious process, and immune response [
36]. Thus, these techniques suggest that treatment with PBMT-sMF or LLLT may reduce the burden on the hospital and health systems and the use of scarce health care resources during this pandemic [
33,
36].
PBMT techniques in the hospital were observed in the clinical case of patient with severe COVID-19 [
34]. This was the case of a 32-year-old Asian woman with morbid obesity and a body mass index of 52, and a history of excision of meningioma and asthma presented to the emergency room with a positive COVID-19 test and shortness of breath, cough, and diarrhea. The patient presented hypoxia with oxygen saturation via pulse oximetry (SpO2) of 88% in room air, tachypneic with a respiratory rate of 35, feverish temperature of 100.5 ºF, pulse rate 89, and blood pressure 106/84. The condition was considered severe, and was worsened, leading to her admission to the ICU. As a result, treatment with LLLT was started. During the first laser treatment, her SpO2 increased from 92% to 97% at 3 L/min of oxygen within 10 min of starting treatment. After the second laser treatment, the patient was breathing without dyspnea. After treatments, her respiratory rate returned abnormally 19–20 breaths/min. After the fourth treatment, the patient was able to ambulate independently and improved the ability to perform activities of daily living. The patient was discharged two days after her last treatment with 1 L/min of oxygen [
34].
Another case was that of a 57-year-old African American man with severe COVID-19 who received four sessions of PBMT once a day by a laser scan and with pulsed modes of 808 nm and super pulses of 905 nm for 28 min [
35]. Oxygen saturation (SpO2) increased from 93–94% to 97–100%, while oxygen demand decreased from 2–4 L/min to 1 L/min. The RALE score improved from 8 to 5. The Pneumonia Severity Index improved from Class V (142) to Class II (67). Additional pulmonary indium (Brescia-COVID and SMART-COP) decreased from 4 to 0. CRP normalized from 15.1 to 1.23. This patient tolerated all 4 treatments daily and observed a significant improvement in breathing immediately after each treatment. Paroxysmal coughing fits were resolved after the third treatment. Upon completion of the fourth treatment, the patient was able to ambulate with physical therapy. The next day after his final treatment, the patient was discharged to an acute rehabilitation facility with oxygen at 1 L/min [
35].
Perhaps soon, the results of clinical trials currently underway should contribute to the assessment of PBMT efficacy for improving respiratory, inflammatory, coagulation and morbidity-mortality parameters in patients undergoing these studies.