Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Bastiaan Tops and Version 2 by Rita Xu.
EWSR1 belongs to the FET family of RNA-binding proteins including also Fused in Sarcoma (FUS), and TATA-box binding protein Associated Factor 15 (TAF15).
- EWSR1
- soft tissue tumors
- bone tumors
- pathology
- molecular
1. Introduction
Ewing sarcoma was molecularly defined by Delattre et al. in 1992 upon the identification of the Ewing sarcoma breakpoint region 1 (EWSR1) located on chromosome 22q12.2 and the term for this gene was coined [1]. EWSR1 is a multifunctional protein ubiquitously expressed in most cell types, indicating diverse roles in physiological cellular processes, including organ development and aging. Genetic and epigenetic pathways are modulated by EWSR1 but the exact mechanisms are still poorly understood [2].
EWSR1 belongs to the FET (also known as TET) family of RNA-binding proteins that also includes Fused in Sarcoma (FUS), and TATA-box binding protein Associated Factor 15 (TAF15) [2]. As a consequence of the multifunctional role of EWSR1 leading to a high frequency of transcription of the chromosomal region where the gene is located, EWSR1 is exposed to aberrations such as rearrangements. Consecutive binding to other genes leads to chimeric proteins inducing oncogenesis. These various somatic genetic rearrangements involving EWSR1 result in a fusion of its N-terminal coding region to the C-terminal DNA binding domain of one of several transcription factors. They are reported to act as aberrant transcription factors with the N-terminal domain of EWSR1 as a strong transactivator. The other TET family members are homologous and are involved in strikingly similar translocation events giving rise to the production of structurally similar oncoproteins [3][4][3,4].
With the advent of widely used modern molecular techniques during the last decades, it has become obvious that EWSR1 is involved in development of diverse benign and malignant tumors with mesenchymal, neuroectodermal, and epithelial/myoepithelial features [5]. As oncogenic transformation mediated by EWSR1-fusion proteins leads to such diverse tumor types, there must be a selection on a multipotent stem cell level [2].
2. Ewing Sarcoma
Arthur Purdy Stout and James Ewing were the first to describe this aggressive small, blue round-cell entity in 1918 and 1921, respectively [6][7][8][6,7,8]. Later on, the chromosomal translocation (11;22) was found by Aurias et al. and Turc-Carel et al. in 1983, the second breakthrough of translocation/fusion-gene associated sarcomas following alveolar rhabdomyosarcoma (ARMS) [9][10][11][9,10,11]. Subsequently, the fusion gene has been detected as mentioned in the introduction [1], being the genetic hallmark by an otherwise aspecific small blue, round-cell tumor. Ewing sarcoma, the prototypic round-cell sarcoma, is relatively common in comparison to other small blue round-cell sarcomas. It arises in soft tissue and bone of children, adolescents, and young adults. Exceptionally, older patients are affected. The mean age is in the second to third decade. White males have the highest incidence and black females the lowest due to ethnic genetic preposition differences. Tumors can originate anywhere in the body, and around 80% of the neoplasms arise in the bone with preference sites in decreasing order of frequency: lower extremities, pelvis, upper extremities, ribs, spine, and craniofacial. Distribution in the soft tissue is extremities, chest wall, retroperitoneum, paravertebral, pelvis, and head and neck. Visceral organs, skin, and epidural spaces are rarely involved [12][13][12,13]. The origin of the peripheral nerve as reported by Stout in 1918 can clinically be confused with malignant peripheral nerve sheath tumor [7]. Macroscopically, these infiltrative lesions are (multi)nodular), fleshy, and often necrotic. A pseudocapsule can be present in soft tissue neoplasms. Post-therapy specimens show fibrosis, necrosis, and hemorrhage, often without visible tumor [12][13][12,13]. Histologically, Ewing sarcoma is composed of cellular sheets of relatively featureless small cells with round dark nuclei and inconspicuous cytoplasm (Figure 1). In some cases, cells are larger displaying more nuclear variability. The cytoplasm can appear clear due to retraction artefacts. Homer-Wright rosettes may be numerous in a subset of cases initially called peripheral primitive neuroectodermal tumors [6][13][6,13]. Adamantinoma-like Ewing sarcoma shows more cohesive sheets and nests of cells with peripheral palisading, prominent desmoplastic stroma with production of hyaline membrane collagen, presence of keratin pearl formation, and comedo-like necrosis. These lesions are predestinated for misinterpretation as carcinoma, since keratins, including high molecular keratins, p40, and p63, are commonly positive [6][14][6,14].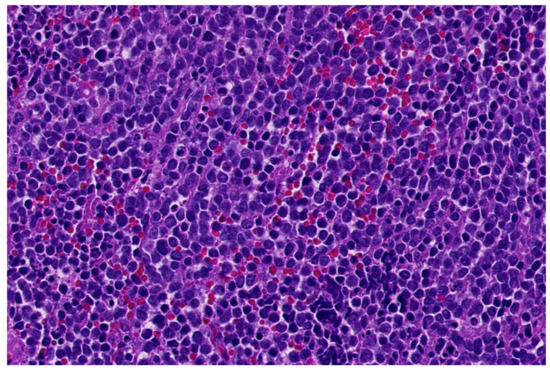
Figure 1.
Classical morphology of Ewing sarcoma (HE; 40× magnification).
Table 1.
Differential diagnoses of Ewing sarcoma.
| Entity | Morphology | IHC | Common Genetic Alterations | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| CIC-sarcoma | Sheets of undifferentiated round/spindle/epitheloid cells; mild nuclear pleomorphism; and necrosis | CD99 (mostly patchy), WT1, ETV4, DUX4, and NUT ( | CIC-NUTM1 | ) | CIC-DUX4/FOXO4/LEUTX/NUTM1/2A | fusions | ||||
| BCOR-sarcoma | Sheets/nests/short fascicles of uniform; bland round-oval-spindle cells; rich capillary network; and myxoid matrix (variable) | BCOR, SATB2, cyclin D1, TLE1, CCNB3 ( | BCOR-CCNB3 | ), and CD99 (50%) | BCOR-CCNB3/MAML3/ZC3H7B, KMT2D | ); | BCOR | ITD*; and | YWHAE-NUTM2B; | *ITD, internal tandem duplication |
| EWSR1 | -nonETS round-cell sarcomas | Cords/nests/pseudoacinar pattern of round-spindle cells; bland-pleomorphic spectrum; and fibro-/myxohyaline stroma | CD99, NKX2.2, and CKAE1/3 (focal, dot-like) | EWSR1 | /FUS-NFATc2 | |||||
| Diverse morphology: round-spindle cells; fibrous stroma | Co-expression of myogenic markers (desmin/myogenin/MyoD1), neurogenic markers (S100/SOX10/MITF/GFAP) and keratins (AE1/3) | EWSR1-PATZ1 or EWSR1-VEZF1 | ||||||||
| Desmoplastic small round-cell tumor | Sheets/nests/cords of uniform; bland round cells; and desmoplastic stroma | Desmin (dot-like), keratin, EMA, and WT1 (C-terminus) | EWSR1-WT1 | |||||||
| Lymphoblastic lymphoma | Small-medium blastoid cells; minimal cytoplasm | CD99, TdT, CD45, CD34, CD1a, and B- and T-cel markers | Diverse | |||||||
| Small-cell carcinoma | Small-medium round-oval cells; salt and pepper chromatin; indistinct nucleoli; molding; and apoptosis | Keratins, CD56, synaptophysin, chromogranin, and TTF1 |
Diverse; | TP53, PTEN | mutations; | RB1 | , 3p loss; and | MYC | amplification | |
| NUT carcinoma | Poorly cohesive sheets of primitive/basaloid cells; abrupt keratinization; and coagulative necrosis | CK5/6, P40, P63, and NUT | NUT-BRD3/BRD4/NSD3/CIC/BCORL1/MGA/MXD4 | |||||||
| Myoepithelial carcinoma | Solid sheets/nests of cell with high nuclear grade or undifferentiated round-cell morphology; facultatively glandular component; necrosis; and high mitotic count | Pankeratins, S100, EMA, GFAP, SOX10, P63, SMA, calponin, desmin (focal); and INI1 loss (subset) | EWSR1 | rearrangements (various fusion partners); | PLAG1 | rearrangements (mixed tumors) | ||||
| ARMS | Nests with central discohesion-solid nests; monomorphic primitive round cells; and multinucleated wreath-like giant cells | Desmin, myogenin (strong, diffuse), MyoD1, keratin, neuro-endocrine markers (CD56, synaptophysin, and chromogranin) | PAX3/PAX7-FOXO1 | |||||||
| Sinonasal glomangiopericytoma | Solid-fascicular pattern; spindle-round cells with minimal atypia; arranged around staghorn vessels; and perivascular hyalinization | Beta-catenin (nuclear), SMA | CTNNB1 | mutations | ||||||
| Glomus tumor | Solid-nested pattern; small, uniform round cells with round nucleus, amphophilic-slightly eosinophilic cytoplasm and sharply defined cell borders; and variable vascular pattern | SMA with membranous accentuation, caldesmon, and collagen IV | MIR143-NOTCH1/2/3 | , and | BRAF/KRAS | mutations | ||||
| Rhabdoid tumor | Solid pattern; rounded-polygonal cells with vesicular nuclei and prominent nucleoli; and eosinophil hyaline-like cytoplasmic inclusions | Diverse; keratins, EMA, CD99, synaptophysin, SALL4, glypican-3, and INI1 loss | SMARCB1 | biallelic loss, | SMARCB1 | or | SMARCA4 | (germline) mutations | ||
| Mesenchymal chondrosarcoma | Biphasic: poorly differentiated round cells and islands of hyaline cartilage; staghorn-like vessels | S100, CD99, SOX9, EMA, desmin, myogenin, and MyoD1 | HEY1-NCOA2 | |||||||
| Synovial sarcoma with round-cell features | Fascicles or sheets of small round hyperchromatic cells; high N/C ratio; staghorn vessels; necrosis; and thin fibrovascular septa | CD99, BCL2, CD56, TLE1, S100 (focal), EMA, and keratins (variable) | SS18-SSX1/2/4 |
