Diabetic retinopathy (DR) is a leading cause of preventable vision impairment and blindness in the European Region. Despite the fact that almost all European countries have some kind of prophylactic eye examination for people with diabetes, the examinations are not properly arranged and are not organized according to the principles of screening in medicine. In 2021, the current COVID-19 pandemic moved telemedicine to the forefront healthcare services.
- diabetic retinopathy
- population screening
- registry
1. Introduction
Diabetes mellitus (DM) has constantly increasing prevalence and incidence rates globally. According to the World Health Organization, about 422 million people worldwide have diabetes, and most of them live in low- or middle-income countries [1]. For people living with the disease, financially affordable diagnostic and treatment services are crucially important for their timely diagnosis, survival, and future quality of life.
Worldwide, over 95 million diabetic patients have DR, of which a third have vision-threatening DR and 7.6% macular edema [2]. Diabetic retinopathy (DR) is a leading cause of preventable vision impairment and blindness in the European Region as well [3][4][3,4]. The damaging effects of diabetes on vision could be prevented by screening programs based on early detection and prompt treatment [4][5][4,5].
The current technological advances in ophthalmology and the COVID-19 pandemic made telemedicine more accessible and a preferred way of providing health care services [6]. Increasing home-office time is one of the reasons more diabetic patients are informed, registered, and followed up. They spend more time on the internet searching, reading e-mails, and participating in online meetings related to their condition. Modern technologies deliver detailed, real-time videos, which when combined with accessible use of ophthalmology equipment allows more patients to a receive specialized medical opinion without even meeting an ophthalmologist.
Despite the fact that almost all European countries offer some kind of prophylactic eye examination for people with diabetes, the examinations are not always organized according to the principles of population-based screening established by Wilson and Jungner in 1968 and accepted by the World Health Organization (WHO) [7]. A well-developed screening program has the potential to identify early changes in the retina, allowing treatment to be offered before vision impairment or blindness appear.
Screening programs for DR are continuously changing and improving. New registries are created, and old ones are updated with increased coverage, new screening methods, and sources of information. The last review article for DR screening programs in Europe dates from 2015 by Pieczynski et al. This is a long period for a constantly developing highly technological specialty such as ophthalmology, which is our main reason for conducting this narrative review.
Early diagnosis of DR may save a substantial amount of resources for treatment and may increase the patients’ quality of life. One of the basic problems in screening for diabetic retinopathy is that many countries cannot detect everyone who has a diagnosis of diabetes. Without a proper registry of diabetic patients, some people may never be screened for DR.
This study aimed to conduct a narrative literature review on current DR screening programs and registries in the European Union (EU) member states for the last 20 years. Their geographical area, age group coverage, type of screening methods, time period, etc. are presented.
2. Findings
We identified 160 articles with the keywords “diabetic”, “retinopathy”, “screening”, and “registry” as well as 270 using “diabetic”, “retinopathy”, “registry”. The full texts of the 44 remaining articles were reviewed after we were sure that the studies met inclusion criteria. Summary characteristics of the diabetic screening programs or registries in the European Union from each of the included studies are presented in Table 1and the following text.
| Country | First Author and Year of Publication | Time Period |
Covered Geographical Area |
Age Group Screened (Years) |
Number of Participants/DR Relative Share | Name of Register/ Type of Study |
|---|---|---|---|---|---|---|
| Finland | Laitinen et al. 2010 [8] | 2000–2001 | Whole of Finland | ≥30 | 7413/1% | Cross-sectional nationwide population survey |
| Hautala et al. 2014 [9] | 2007–2011 | 35 municipalities of the Northern Ostrobothnia Hospital District | No age limitation | 14,866/23% mild background retinopathy, 31% moderate or severe background retinopathy, 3%—PDR | Finnish Register of Visual Impairment | |
| Laatikainen et al. 2016 [10] | 1982–2010 | Whole of Finland | 18–64 | 42,626/0.09% | Finnish Register of Visual Impairment | |
| France | Massin et al. 2008 [11] | 2004–2006 | Paris region | 1–106 | 15,307/23.4% DR | Regional telemedical network/OPHDIAT/ |
| Schulze-Döbold et al. 2012 [12] | 2004–2009 | Paris region | All ages | 38,596/14.7% advanced stage retinopathy | Regional telemedical network/OPHDIAT/ | |
| Ireland | Kelliher et al. 2006 [13] | 1996–2003 | Whole of Ireland | No age limitation | 470/7% DR | The National Council for the Blind in Ireland (NCBI) |
| James et al. 2016 [14] | 2010–2012 | Mid-West of Ireland | ≥20 | 1434/20.1% background retinopathy, 8.2% sight threatening retinopathy | Mid-West Diabetic Retinopathy Screening Pro- gramme (MWDRS) | |
| Tracey et al. 2016 [15] | 2004–2013 | Whole of Ireland | 18–69 | 57,626–109,842/0.4–1.9% during 10-year period | National Council for the Blind of Ireland | |
| Denmark | Andersen et al. 2016 [16] | 2014–2015 | Whole of Denmark | ≥18 years | 77,968/18% NPDR, 4% PDR |
Danish Registry of Diabetic Retinopathy (DiaBase) |
| Holm et al. 2018 [17] | 2010 and still ongoing | Copenhagen City | No age limitation | 21,000/11.3% DR | National Patient Register Danish Adult Diabetes Database | |
| Scotland | Looker et al. 2014 [18] | 2006–2010 | >99% of the Scottish population | ≥12 | 187,822/0.6–1.8% referable background retinopathy | National diabetes registry—Scottish Care Information-Diabetes Collaboration (SCI-DC) database |
| Wales | Thomas et al. 2015 [19] | 2005 and still ongoing | Whole of Wales | ≥12 | 91,393/32.4% DR | Diabetic Retinopathy Screening Service for Wales (DRSSW) |
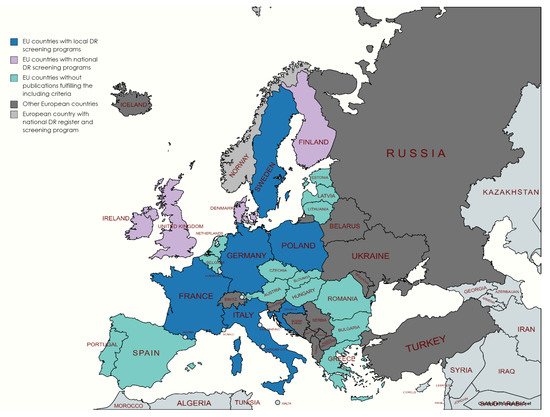
Only a few EU countries (Finland, Sweden, Ireland, and Denmark) have national DR screening programs (Figure 12). These programs are predominantly based on preexisting national population-based diabetes registers.
In Finland, the existing Finnish Register of Visual Impairment (RVI) does not require the permission of the patient for registration. Every patient with a diagnosed visual impairment is entitled to an ophthalmology examination, and patients with DR are included by the ophthalmologist in the register. The method of the screening is not specified, as every ophthalmologist might use a different approach. The organization guarantees that almost all diabetic patients are screened, although there is no particular DR register in the country [8][10].
In Sweden, unlike other EU countries, the Swedish Diabetes Registry is the source of information for the DR screening of patients with type 2 diabetes and type 1 diabetes who are on insulin treatment and for patients with a diagnosis at 30 years of age or younger. The register includes children and adults with a diagnosis of diabetes for up to five years when first recorded in the registry. Similar to Finland, the method of screening is not indicated. Both countries have local screening programs along with national ones.
Provisional lists of diabetic patients are made by a combination of Primary Care Reimbursement Service (PCRS) sources, Hospital In-Patient Enquiry (HIPE) scheme, Patient Administration System (PAS), and Laboratory Information System (LIS) sources [14][16]. The screening methods include a dilated ocular examination by a single ophthalmologist, primarily with slit-lamp biomicroscopy or with indirect and direct ophthalmoscopy in cases of poor patient mobility. Of the 1943 patients who were offered screening during the study period, 1434 attended, and 405 were diagnosed with different stages of DR. GPs can register patients, and the program constantly receives the contact details of the majority of persons with diabetes from the National Health Schemes.
DiaBase contains data collected from hospital eye departments and private ophthalmological practices for all diabetes patients aged ≥18 years in the five regions of Denmark. Prevalence of non-proliferative diabetic retinopathy (early stage of DR in which symptoms are mild or nonexistent) of 14,034 patients and proliferative DR (advanced stage of diabetic eye disease which affects central and peripheral vision) of 3118 patients among a total of 77,968 diabetes patients nationwide for a two-year period have been reported. The proportion of patients with diabetic retinopathy regression in Denmark is greater than the proportion of patients with progression, although the number of newly diagnosed patients with diabetes has been increasing every year [16][18]. This fact demonstrates the success of DiaBase and the importance of the existing well-functioning national registry and screening program.
A non-mydriatic camera installed in the diabetology department has been used for fundus photographs of diabetic patients, which have been taken by trained nurses and electronically transmitted to the ophthalmology department for interpretation. Only patients with no documented DR or mild DR are referred for screening. The centers are located in the diabetology departments of 11 different hospitals and healthcare centers. Two retinal photographs are generally taken by trained orthoptists and nurses, one centered on the posterior pole and the other on the optic disc.
In Germany, there are no existing screening programs or DR registry. Information about DR patients comes from a population-based registry of blindness in the country. The register contains a code indicating the probable cause of blindness. That coding is based on a review of written medical and ophthalmological opinions.
However, few geographically limited population-based studies report the prevalence and incidence of DR in the past [20][21][25,26]. There are several telemedicine regional screening programs in progress [22][23][24][27,28,29]. All of them are based on fundus photos taken in diabetes centers by trained nurses, paramedical staff, or other medical personnel. The preferred screening method is nonmydriatic color fundus photos electronically transmitted to a reading center for examination by certified expert ophthalmologists.
The United Kingdom is the largest country in Europe with nationwide screening for all patients with DM above the age of 12 years. It contains over 9 million patients in total, which covers around 6% of the UK population. The THIN database contains individual patient information recorded by primary care practitioners as part of their routine clinical care. There is no separate registry of patients with DR, but it is an enormous database containing information about all diabetic patients and patients with retinopathy related to diabetes.
Everyone who has a Primary Care Physician and a respective NHS identifier number and has been diagnosed with diabetes receives an invitation letter for a diabetic eye screening appointment once a year. The rate of retinopathy is 2807 per 100,000 screened in 2003–2016 year. Screening includes two 45° fields mydriatic photographs [25][32]. Screening images are evaluated by higher-ranked graders with a subsequent referral to an NHS hospital with eye services when that is indicated.
In 2006, Scotland launched a national Scottish DR Screening service (DRS). Patients identified as high risk are referred to eye clinics for assessment and further management. Patients eligible for screening are identified via the national diabetes registry—the Scottish Care Information-Diabetes Collaboration (SCI-DC) database. When photographic images are ungradable, a slit-lamp examination is undertaken.
In Wales, a population-based diabetes register was established based on information from the hospital patient administration systems and lists of diabetic patients from all primary care practices in 2001. It is performed by optometrists trained to use slit-lamp biomicroscopy and non-contact lens or by ophthalmology nurses who are trained to take the photographs and grade them. All persons invited for screening receive an appointment letter with a date, time, and venue for the screening. Thirty photographic teams consisting of a healthcare professional and an accredited photographer take two 45° fields (one macula centered and one nasal)
Northern Ireland has a regional Diabetic Eye Screening Program (DESP). Invitation letters with a fixed date and time for screening are sent to all eligible people. Two or more photographs are taken of each eye using a special camera by an optometrist. If a person is over 50 years of age, eye drops are instilled about 15 min before the test to dilate their pupils [26][33].
3. Conclusions
In the era of technology and preventive medicine, there are still developed European countries with no national DR screening programs or registry. Based on our literature review, countries of Western Europe have successful ongoing screening programs. For Eastern European countries, there is insufficient information. In the meantime, global incidence rates of DM rise steeply due to aging populations.
