KD is an eponym for a delayed post-traumatic bone osteonecrosis. Patients usually present with advanced stage kyphosis in the thoracolumbar (T-L) area within months to years after experiencing a minor trauma, initially presenting without any symptoms. Possible causes include avascular osteonecrosis, microfracture, atrophic nonunion, and a nutritional injury fracture.
- Kummell’s disease
- intravertebral vacuum cleft
- vertebral body collapse
- vertebral osteonecrosis
- surgical treatment
1. Introduction
Current literature states that the incidence of KD is around 7% to 37% in elderly individuals. The population in developed countries is aging and KD is a potential complication in up to one-third of OVCFs, which requires discussing an appropriate therapeutic approach for these patients [1][2][3][4][5][6][7][8][9][10][11][12][13][14]. KD usually affects the lower thoracic or upper lumbar region of the spine and it usually involves only a single vertebra [15]. The majority of injuries remain asymptomatic.
In the female age range of 50 to 54 around 10% of the patients suffered from at least 1 OVCF, but after the age of 80 statistics revealed a sudden spike to 50%. This analysis emphasizes a big role of prophylactic measures, watchful waiting, and the observation in an aging population that is at risk of osteoporosis or one with an OVCF. Prophylaxis should be implemented to minimize the prevalence of altered healing, nonunion, intravertebral vacuum clefts (IVC), and the most emerging and dangerous complication of vertebral fractures that is KD. These complications reduce the patient’s quality of life (QoL) and therefore require adequate preventive measures.
2. Epidemiology
However elderly patients with multiple comorbidities and a decreased BMD are at an even greater risk [16]. Whenever fractures fail to fuse, the patient’s pain increases, the QoL decreases, and even neurological deficits can occur. Current literature provides us with the evidence that justifies the use of radiological studies as a predictor of delayed union [17][18][19]. in their prospective cohort study from 2020 proposed the following radiological risk factors for nonunion 12 months after an OVCF:(1)a middle column
Additional risk factors are: the female sex, having a low body mass index (BMI), smoking, a sedentary lifestyle, low calcium intake, and frequent falls [16].
3. Risk Factors
Osteoporosis is the biggest risk factor for KD, hence its high frequency in the affected patient population. Osteoporosis is found in more than 20% of the population over 50 years of age and appears more often in slim white females [20].
The idiopathic origin of KD may be due to drug cytotoxicity, avascular necrosis, and decreased intraosseous blood flow [21].
Post-traumatic avascular necrosis is the most frequent factor causing decreased blood supply to the bone marrow. Any damage that can obstruct the vessel supplying the vertebral body can lead to non-healing and osteonecrosis.
There are a variety of conditions that can obstruct the artery lumen supporting the spine: sickle cell crisis, Gaucher’s disease, Caisson disease, SLE, prothrombotic states, pancreatitis, lipolytic enzymes, fluid overload, dyslipidemia, leukemia, lymphoma, diabetes mellitus, sarcoidosis, cirrhosis, hyperuricemia, malignancies, prolonged corticosteroid use (at least 5 mg per day over a period of 3 months), and alcohol abuse [22][23].
4. Treatment
Because the majority of OVCFs are type A or type B, the aforementioned scales primarily point towards conservative treatment, with the greatest focus being on the maintenance of the patient’s health when the disease is not significantly advanced [24]. Jang J.S. et al. and Stallenberg B. et al. established that patients with OVCFs with nonunion and back pain with or without symptoms of neurogenic compression are candidates for surgical stabilization [25][26]. Studies consistently show that up to a third of the patients will unfortunately not respond successfully to conservative therapy alone when dealing with OVCFs [27]. Even though patients with KD are elderly and suffer from multiple comorbidities, MIS reduces iatrogenic tissue trauma due to smaller incisions, decreases soft tissue damage and blood loss, and reduces muscular and ligamentous rupture.
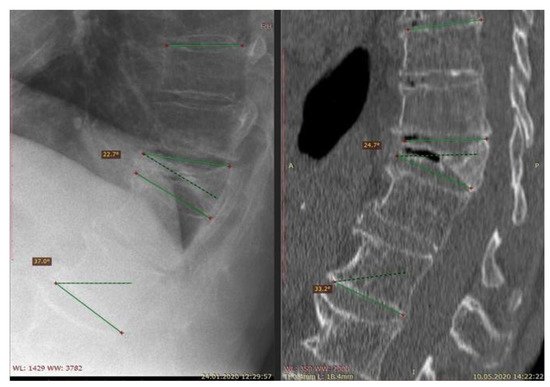
Over-the-counter pain medications are often effective in pain management, but they do not facilitate the healing process. Therefore, bone-strengthening drugs such as bisphosphonates and hormone replacement therapy may be prescribed to stabilize and restore the bone density [28]. Reducing the range of motion (ROM) with a back brace helps in weight-bearing and decreases postural flexion. Nevertheless as shown in Figure 1., it is controversial whether bracing is effective in the treatment of spinal injury and if it provides better outcomes [29].
The usual adverse effects of pharmaceuticals used by patients with KD that affect the central nervous system can lead to cognitive impairment, sedation, and constipation, especially in elderly patients. NSAIDs and acetaminophen use causes gastritis, gastric ulcers, hepatic and renal problems; especially in large doses, which can eventually lead to the worsening of the overall condition of the patient. The lack of physical activity can also lead to an impaired cardiovascular system and pulmonary function results [30]. There are not that many studies that clearly mention the complications of conservative therapy, but many physicians concur that patients using back brace are prone to back muscle atrophy, as stated by Mazanes D. et al.
The decision to perform surgery in order to improve the patient’s condition and to prevent further deterioration of the patient’s health is made in the following events: conservative management is ineffective; there are neurological complications; there is pain limiting the patient’s ROM; and when there is a significant degree of kyphosis and neurogenic claudication [31]. In a majority of the cases, surgery is chosen [32]. MIS is less traumatic than conventional open surgery, potentially resulting in a faster recovery while providing similar clinical mid to long-term results. Bone cement-augmented pedicle screw fixation and the SJ system are other options for restoring spinal stability, alleviating debilitating pain, and improving clinical outcomes [33].
References
- Hansen, E.J.; Simony, A.; Carreon, L.; Rousing, R.; Tropp, H.T.; Andersen, M.Ø. Vertebroplasty vs. SHAM for Treating Osteoporotic Vertebral Compression Fractures: A Double Blind RCT (VOPE). Integr. J. Orthop. Traumatol. 2019, 2, 1–6.
- Zhu, Y.; Cheng, J.; Yin, J.; Zhang, Z.; Liu, C.; Hao, D. Therapeutic effect of kyphoplasty and balloon vertebroplasty on osteoporotic vertebral compression fracture. Medicine 2019, 98, e17810.
- Lou, S.; Shi, X.; Zhang, X.; Lyu, H.; Li, Z.; Wang, Y. Percutaneous vertebroplasty versus non-operative treatment for osteoporotic vertebral compression fractures: A meta-analysis of randomized controlled trials. Osteoporos. Int. 2019, 30, 2369–2380.
- Xu, J.; Lin, J.; Li, J.; Yang, Y.; Fei, Q. “Targeted Percutaneous Vertebroplasty” Versus Traditional Percutaneous Vertebroplasty for Osteoporotic Vertebral Compression Fracture. Surg. Innov. 2019, 26, 551–559.
- Figueiredo, N.; Barra, F.; Moraes, L.; Rotta, R.; Casulari, L.A. Percutaneous vertebroplasty: A comparison between the procedure using the traditional and the new side-opening cannula for osteoporotic vertebral fracture. Arq. Neuro-Psiquiatr. 2009, 67, 377–381.
- Chen, C.; Bian, J.; Zhang, W.; Zhang, W.; Zhao, C.; Wei, H. Unilateral Versus Bilateral Vertebroplasty for Severe Osteoporotic Vertebral Compression Fractures. J. Spinal Disord. Tech. 2014, 27, E301–E304.
- Noriega, D.C.; Rodrίguez-Monsalve, F.; Ramajo, R.; Sánchez-Lite, I.; Toribio, B.; Ardura, F. Long-term safety and clinical performance of kyphoplasty and SpineJack® procedures in the treatment of osteoporotic vertebral compression fractures: A pilot, monocentric, investigator-initiated study. Osteoporos. Int. 2019, 30, 637–645.
- Zhang, L.; Wang, J.; Feng, X.; Tao, Y.; Yang, J.; Wang, Y.; Zhang, S.; Cai, J.; Huang, J. A comparison of high viscosity bone cement and low viscosity bone cement vertebroplasty for severe osteoporotic vertebral compression fractures. Clin. Neurol. Neurosurg. 2015, 129, 10–16.
- Schwarz, F.; McLean, A.L.; Steinberg, A.L.; Ewald, C.; Kalff, R.; Waschke, A. Prospective randomized comparison of early versus newer-generation vertebral access devices for kyphoplasty. Arch. Orthop. Trauma Surg. 2019, 139, 1571–1577.
- Van Meirhaeghe, J.; Bastian, L.; Boonen, S.; Ranstam, J.; Tillman, J.B.; Wardlaw, D. A Randomized Trial of Balloon Kyphoplasty and Nonsurgical Management for Treating Acute Vertebral Compression Fractures: Vertebral body kyphosis correction and surgical parameters. Spine 2013, 38, 971–983.
- Yang, S.; Chen, C.; Wang, H.; Wu, Z.; Liu, L. A systematic review of unilateral versus bilateral percutaneous vertebroplasty/percutaneous kyphoplasty for osteoporotic vertebral compression fractures. Acta Orthop. Traumatol. Turc. 2017, 51, 290–297.
- Tang, J.; Guo, W.-C.; Hu, J.-F.; Yu, L. Unilateral and Bilateral Percutaneous Kyphoplasty for Thoracolumbar Osteoporotic Compression Fractures. J. Coll. Physicians Surg. Pak. 2019, 29, 946–950.
- Duan, Z.-K.; Zou, J.-F.; He, X.-L.; Huang, C.-D.; He, C.-J. Bone-filling mesh container versus percutaneous kyphoplasty in treating Kümmell’s disease. Arch. Osteoporos. 2019, 14, 109.
- Freedman, B.A.; Heller, J.G. Kummel Disease: A Not-So-Rare Complication of Osteoporotic Vertebral Compression Fractures. J. Am. Board Fam. Med. 2009, 22, 75–78.
- Fink, H.A.; Milavetz, D.L.; Palermo, L.; Nevitt, M.C.; Cauley, J.A.; Genant, H.K.; Black, D.M.; Ensrud, K.E.; Fracture Intervention Trial Research Group. What Proportion of Incident Radiographic Vertebral Deformities Is Clinically Diagnosed and Vice Versa? J. Bone Miner. Res. 2005, 20, 1216–1222.
- Formica, M.; Zanirato, A.; Cavagnaro, L.; Basso, M.; Divano, S.; Formica, C.; Felli, L. What is the Current Evidence on Vertebral Body Osteonecrosis?: A Systematic Review of the Literature. Asian Spine J. 2018, 12, 586–599.
- Kanchiku, T.; Imajo, Y.; Suzuki, H.; Yoshida, Y.; Taguchi, T. Usefulness of an Early MRI-based Classification System for Predicting Vertebral Collapse and Pseudoarthrosis After Osteoporotic Vertebral Fractures. J. Spinal Disord. Tech. 2014, 27, E61–E65.
- Tsujio, T.; Nakamura, H.; Terai, H.; Hoshino, M.; Namikawa, T.; Matsumura, A.; Kato, M.; Suzuki, A.; Takayama, K.; Fukushima, W.; et al. Characteristic Radiographic or Magnetic Resonance Images of Fresh Osteoporotic Vertebral Fractures Predicting Potential Risk for Nonunion: A prospective multicenter study. Spine 2011, 36, 1229–1235.
- Takahashi, S.; Hoshino, M.; Takayama, K.; Iseki, K.; Sasaoka, R.; Tsujio, T.; Yasuda, H.; Sasaki, T.; Kanematsu, F.; Kono, H.; et al. Predicting delayed union in osteoporotic vertebral fractures with consecutive magnetic resonance imaging in the acute phase: A multicenter cohort study. Osteoporos. Int. 2016, 27, 3567–3575.
- Steel, H.H. Kümmell’s disease. Am. J. Surg. 1951, 81, 161–167.
- He, D.; Yu, W.; Chen, Z.; Li, L.; Zhu, K.; Fan, S. Pathogenesis of the intravertebral vacuum of Kümmell’s disease. Exp. Ther. Med. 2016, 12, 879–882.
- McCarthy, J.; Davis, A. Diagnosis and Management of Vertebral Compression Fractures. Am. Fam. Phys. 2016, 94, 44–50.
- Lim, J.; Choi, S.-W.; Youm, J.-Y.; Kwon, H.-J.; Kim, S.-H.; Koh, H.-S. Posttraumatic Delayed Vertebral Collapse: Kummell’s Disease. J. Korean Neurosurg. Soc. 2018, 61, 1–9.
- Kondo, K.L. Osteoporotic Vertebral Compression Fractures and Vertebral Augmentation. Semin. Interv. Radiol. 2008, 25, 412–424.
- Jang, J.-S.; Kim, D.-Y.; Lee, S.-H. Efficacy of Percutaneous Vertebroplasty in the Treatment of Intravertebral Pseudarthrosis Associated With Noninfected Avascular Necrosis of the Vertebral Body. Spine 2003, 28, 1588–1592.
- Stallenberg, B.; Madani, A.; Burny, F.; Gevenois, P.A. The Vacuum Phenomenon: A CT sign of nonunited fracture. Am. J. Roentgenol. 2001, 176, 1161–1164.
- Pilitsis, J.G. Vertebral Compression Fractures, American Association of Neurological Surgeons Vertebral Compression Fractures—Symptoms, Complications, Diagnosis and Treatments. Available online: (accessed on 2 August 2020).
- Pierce, T.P.; Jauregui, J.J.; Elmallah, R.K.; Lavernia, C.J.; Mont, M.A.; Nace, J. A current review of core decompression in the treatment of osteonecrosis of the femoral head. Curr. Rev. Musculoskelet. Med. 2015, 8, 228–232.
- Vaccaro, A.; Kandziora, F.; Fehlings, M.; Shanmughanathan, R. Nonoperative Treatment/Bracing for A0 Minor, Nonstructural Fractures. Available online: (accessed on 2 August 2020).
- Parry, S.M.; Puthucheary, Z.A. The impact of extended bed rest on the musculoskeletal system in the critical care environment. Extreme Physiol. Med. 2015, 4, 1–8.
- O’Neill, T.W.; Felsenberg, D.; Varlow, J.; Cooper, C.; Kanis, J.A.; Silman, A.J. The prevalence of vertebral deformities in European men and women: The european vertebral osteoporosis study. J. Bone Miner. Res. 1996, 11, 1010–1018.
- Mazanec, D.J.; Podichetty, V.K.; Mompoint, A.; Potnis, A. Vertebral compression fractures: Manage aggressively to prevent sequelae. Clevel. Clin. J. Med. 2003, 70, 147–156.
- Noriega, D.; Maestretti, G.; Renaud, C.; Francaviglia, N.; Ould-Slimane, M.; Queinnec, S.; Ekkerlein, H.; Hassel, F.; Gumpert, R.; Sabatier, P.; et al. Clinical Performance and Safety of 108 SpineJack Implantations: 1-Year Results of a Prospective Multicentre Single-Arm Registry Study. BioMed Res. Int. 2015, 2015, 173872.
