Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Grazia Cicirelli and Version 1 by Grazia Cicirelli.
Over the last decade, there has been considerable and increasing interest in the development of Active and Assisted Living (AAL) systems to support independent living. The demographic change towards an aging population has introduced new challenges to today’s society from both an economic and societal standpoint. AAL can provide an array of solutions for improving the quality of life of individuals, for allowing people to live healthier and independently for longer, for helping people with disabilities, and for supporting caregivers and medical staff.
- active assisted living
- wearable sensors
- smart objects
- environmental sensors
- data collection
- methodologies for data analysis
1. Introduction
In the last decade, smart environments have found wide application in several contexts, such as domotic, education, rehabilitation, assistance, and so on. Structuring classroom environments with new technologies makes learning more attractive, as well as providing support for teaching people with disabilities [1]. Similarly, new technological devices provide more specific tools and support for the rehabilitation of people with impairment [2][3]. In the context of home automation, the deployment of new technologies can improve the quality of daily life, provide easy access to many functions remotely, or allow the use of natural interfaces, such as gestures and voice, in order to control lighting, climate, entertainment systems, and appliances [4][5].
Contextually, a new need has recently emerged: as the population ages, new policies, systems, and technologies for supporting healthy aging are needed [6]. Aging leads to gradual physical decay, which increases the dependency on other people. Starting from this consideration, two different aspects can be examined. On the one hand, new technologies can be used to monitor older people in order to reduce daily physical assistance and prolong their autonomous life. In this context, medicine and diet adherence, sleep monitoring, or fall detection are some of the main issues that are to be considered and tackled. On the other hand, monitoring people who are not yet very old and that do not suffer from particular pathologies is strategic for the purpose of detecting eventual lifestyle changes and suspicious behaviors that could warn of the onset of neurodegenerative diseases at a very early stage.
In gerontology literature, the decrease in physical activity is considered to be strictly correlated with ageing, and it is associated with low social function, depression, and cognitive decline [7]. A focus on physical, social and cognitive activity is needed in order to promote active and healthy ageing, and to permit people to live independently for longer [8]. Active Assisted Living (AAL) technologies can intervene to help elderly people in the different stages of aging. Indeed, AAL is intended to develop innovation in order to keep people connected, healthy, active, and happy into their old age. It concerns the development of products and services that make a real difference to people’s lives, for those who face some of the challenges of ageing and those who care for older people who need help.
In recent years, a growing body of literature has examined the state of the art of AAL domain by different points of view. In [9][10], the authors focused on the technologies for Activity Recognition in Smart Home. In [11], a review of the literature on mobile technology, such as smartphones, smartwatches, and wristbands, is presented, which describes how these wearable technologies can be used to promote an active lifestyle. Non-wearable (i.e., ambient) technologies are surveyed in [12] for the development of various elderly care systems, whereas IoT Wearable Sensors are reviewed in [13][14]. In [15], video-based technologies have been reviewed. The AAL system requirements and implementation challenges examining the existing Reference Models and Reference Architectures, from an architectural point of view, are investigated in [16], which highlight both the quality attributes and critical issues.
2. Application Contexts
The design and development of an AAL system involve different aspects that can be summarized in three principal words: who, where, and what. Target people are persons with different abilities and skills that have to be monitored by the system (who). The application contexts vary from indoor to outdoor environments and, hence, involve different solutions from both the technological and methodological points of view (where). Finally, an AAL system implies a wide range of functionalities that span from simple alerts when dangerous events happen, to more complex behavioral analysis (what). Figure 1 outlines these aspects in a sketch and they are described in the following sections.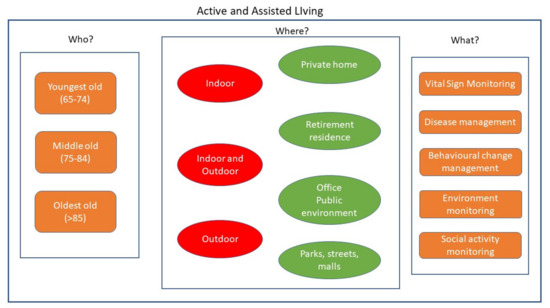
Figure 1. Fundamental aspects to be considered in the design and development of an AAL system: possible users (who?), environments (where?), and functionalities (what?).
2.1. Target Users
AAL systems are principally targeted to elderly adults, aiming maintain continuous support and prolong their autonomous life in an active and healthy way. Medical studies have categorized elderly people into three different classes, depending on their age: those between the ages of 65 and 74 years are classified as youngest-old, those between 75 and 84 years old as middle-old, and those aged over 85 years as oldest-old [17]. For all of these classes of people, health practices are aimed at disease management, at alarm alerting, or at behavioral change management. In recent years, several applications for diabetes control, depression treatment, hypertension control, medication adherence, and psychological support have been developed to allow people to live alone while having the possibility of daily control over their health status. Alarm alerting applications can save human life, when critical events, such as falls, prolonged inactivity, or environmental dangers, are detected. The early detection of behavioral changes is necessary before a notable deterioration of the basic activities involved in daily living [18]. Scientific studies have pointed out that the activity levels of people drop significantly when they retire. By the early identification of the risk factors of functional decline, this can be prevented in a large portion of the elderly population at the time of retirement by targeting timely interventions and reducing the risks. Furthermore, behavioral change applications include monitoring some dangerous attitudes, such as smoking, calorie intake for diet and exercise, and physical activity levels.
2.2. Indoor Environments
In the literature, most of the researches focus on AAL systems for indoor environments. One of the main application contexts related to medical and public health practices supported by devices that deliver health care services via mobile communication. New systems and methods have been developed for the continuous monitoring of biological, behavioral, or environmental data, delivering interventions, and assessing their outcomes. Through the development of systems collecting data coming from heterogeneous sensors and additional self-reported data, new information regarding physiological, psychological, emotional, and environmental states can be derived.
Indoor environments can be further differentiated in homes [19], where people live alone or with a few relatives and retirement residences, where more people live together, move in common spaces, perform group or individual activities, and undertake controlled physical activities [20]. Health status evaluation can be carried out by observing people movements, recognizing their actions, evaluating resting periods, monitoring food intake, and so on. Behavioral analysis can be done by detecting anomalies while comparing the actual behavior with the expected one [21]. Social activities in a group or interactions with relatives and friends can also be monitored.
2.3. Outdoor Environments
Elderly people spend a number of hours of the day outside the home environment. Recent studies have pointed out the need for seniors to spend time in outdoor environments, as they are motivated to be more active not only physically, but also spiritually and socially [22]. Moreover, outdoor habits, such as walking, shopping, meeting other people, and performing physical activities, can greatly help in the prevention of functional decline. If, on one hand, this is widely recognized to be very beneficial for elderly people, on the other hand it inevitably causes new safety concerns. In outdoor environments, elderly people can be exposed to several risks, such as falls or excessive heat or cold. Furthermore, in the case of people having early symptoms of dementia, wandering and becoming confused or lost are common risks. In these scenarios, the main objective of AAL systems is to provide support to elderly people in various aspects, such as in checking the routes, recognizing anomalous behaviors, evaluating motion activities, and so on.
In recent years, several projects have developed different solutions to expand ambient assisted systems from indoor spaces to outdoor and public environments, with the aim of creating different services for improving the wellbeing of people [23]. In general, these projects gather data from people observations, store them securely, and, by their analysis, create intervention systems that can be applied for both general or specific monitoring scenarios. These systems can support elderly people by giving them hints and suggestions that are based on the analyzed data acquired daily [24][25] in order to slow the progression of their cognitive and behavioral decline [26].
3. Technologies
3.1. Wearable Sensors
In recent years, a number of wearable sensors have been miniaturized and made very efficient in terms of energy consumption. Three-axis accelerometers, gyroscopes, and magnetometers are the most commonly used wearable sensors, which are usually worn at the user hip or waist. They have been extensively applied for different purposes, such as to assess the postural stability of a subject [27], to detect and classify falls [28][29][30][31][32], or to analyze the gait cycle [33]. Moreover, these sensors are embedded in mobile technologies, such as smartphones, smartwatches, and wristbands, which also support the continuous monitoring of biological, behavioral, and environmental data [34][35][36].
Solutions that are based on passive Radio-Frequency Identification (RFID) technology have been largely used to identify the dynamic position of people moving in indoor environments. Information regarding human motion is carried out when wearable electromagnetic markers (tags) move within an electromagnetic field that is radiated by an interrogating antenna and sensed by the remote receiver or reader [37][38]. This type of system not only monitors movements and location, but also accidental falls [39].
An additional technology that has undergone significant developments over the last two decades is Bluetooth Low Energy (BLE) technology, which has paved the way to Bluetooth Smart for wearable devices, which has also solved the limitations related to low broadband connectivity in some particular environments. This technology has been considered for healthcare applications, such as daily physical activity monitoring, health monitoring in cardiac patients, intelligent stethoscope development, emotional level diagnosis [40], falls, and location of elderly people [41]. When multiple areas of an environment are equipped with BLE scanners and BLE beacons are attached to home residents, the system records residents’ activities, which helps to localize and track them [42], detect risky areas, and to prevent injuries and dangerous events without intruding on personal privacy [43].
The AAL systems examined so far, principally monitor the behavioral status of people. Additional relevant parameters have to be monitored in order to ascertain overall health status of an individual. These are the physiological parameters, which are also known as vital signs, such as heart rate (HR), blood pressure, body temperature, respiratory rate, and blood oxygen saturation. Keeping track of vital bodily functions can be done through different sensors that can be complementary to the aforementioned sensors in order to build complete long-term health monitoring systems in daily-life scenarios. Recent improvements in the performance and cost-effectiveness of microelectro-mechanical systems have opened new possibilities in continuous vital sign monitoring. In particular, ballistocardiography (BCG) and seismocardiography (SCG) are promising techniques for extracting information on cardiac events and phases. They are based on IMU sensors positioned over the subject’s sternum for assessing the breathing rate and quality metrics of physical activities [44], or for measuring vibrations that are produced by the heart’s mechanical activity [45]. Smart technology is also used to equip portable objects, such as glasses, in order to evaluate some vital signs, such as heart rate, respiratory rate, regularity of pulse and respiration, the presence and length of apnea events, the temperature distribution on the face, etc. [46]. Such methods are very important for healthcare professionals, because they allow for collecting important medical information without the connection of dedicated hardware to the patient, but with a more natural method.
In outdoor contexts, standard mobile devices can be used for increasing the elderly’s independence without them having to interact with the technology. By using the built-in sensors of cellphones, normal activities can be discerned from those that are considered not allowed and dangerous for the health of the observed individuals [47]. By integrating information that is provided by a GPS and accelerometer with online weather data, it is possible to infer physical and mental health information, such as long exposure to hazardous weather, wandering, or getting lost in order to create safe outdoor spaces [48]. Sensor boxes that are interfaced with mobile/phone applications acting as intelligent navigators can make street navigation accessible to impaired people [49].
3.2. Smart Everyday Objects
With the recent emergence of Internet of Things (IoT) and miniaturized sensors and processors, everyday objects can be identifiable, and they possess the ability to communicate and interact: in a word they can be smart. In this way, home appliances can communicate with each other or be controlled remotely, providing home residents with new facilities that are able to detect anomalies or assess health issues early, in order to apply prevention policies or trigger actions [50][51][52]. In AAL contexts, smart every day objects are generally used together with wearable sensors to acquire joint knowledge regarding individual activities and interactions with the objects in the environment [53][54][55].
Home cooking is one of the basic activities in a daily routine. Monitoring elderly people when they use kitchen appliances is very important in preventing injures and increasing safety. The first signs of cognitive disorders are often easily seen in behaving variations during meal preparation or cooker handling. Some common appliances, such as refrigerators, microwaves, and cooktops, are interconnected with each other to provide assistance in meal preparation tasks [56]. Furthermore, specific conditions, such as the presence of objects on cookers, the presence of lids on the pots, and the liquid level in the pots, can be monitored during the cooking process [57].
Sensors in furniture, such as doors, beds, chairs, washstand, toilet, and cupboards, allow for the non-obtrusive monitoring of daily living activities, providing presence statistics of users in different spaces of the environment [54][58]. Furthermore, power meters can be used to monitor appliance usage, such as TV set or lamps [55], whereas smart pill box devices can be very useful for checking medication intake [53].
Many other solutions have been proposed to provide intelligent functionalities to specific objects and monitor some specific issues that are related to the health and safety of elderly people. Cushion sensors, for example, can be used in wheelchairs to track user posture [59] or capture the heart rate of a person sitting on it [60]. Smart carpets and smart walls can have various functionalities, such as monitoring the walking activity of people, in order to detect falls, measure gait, and count the number of people traversing the environment (socializing activity) [61][62].
3.3. Environmental Sensors
Environmental monitoring sensors are used to detect parameters, such as temperature or air quality, which could have an adverse impact on elderly people [63][64]. They also contribute to monitoring daily life activities [65][66] or localizing people [67][68][69][70] and objects around people [71]. Unlike wearable sensors and smart object sensors, environmental sensors are placed in the environment without being invasive for people and without structuring or replacing home objects.
Radio-frequency-based systems, through the analysis of the reflections of radio-frequency signals, can be used for monitoring different people’s activities, such as sleep monitoring by inferring the subjects’ sleep postures [72], capturing people’s 3D dynamics, learning people’s interactions with the objects [73], and for detecting changes in movement patterns [74]. Microwave sensors can operate through optically opaque materials, such as clothing, as they are not impacted by external visible lighting and scene color, and they may eventually help to sense through fog and smoke. Intelligent metasurface systems transform measured microwave data into images and allow for the recognition of hand signs and vital signs of multiple non-cooperative people [75][76][77].
Intelligent optical systems are an example of environmental sensory systems that are used for biomedical signal acquisition to reveal rigid and uncontrollable gestures, postural instability, or small tremor, which can be signs of incoming neurological diseases. Low-cost devices, such as Kinect™and Wii™, can be easily installed for monitoring the daily activity of people in order to keep an active and healthy life under observation and to notify caregivers in the case of calls for help [2][78][79].
3.4. Social Assistive Robots
Social Assistive Robots are less common than wearable or environmental sensors, but they represent an emerging technology that can support and enhance human activities, especially in heavy tasks [80]. Social Assistive Robots can be used for different purposes: to overcome elderly inabilities; to relieve nursing staff from time-consuming, non-empathic, and repetitive tasks in retirement house [81][82]; to transport food or medicine carts; for grasping objects [20]; for laundry collection; and, delivery services, mail delivery, warehouse logistics, trash logistics, and cleaning material logistics [83]. With the spread of these innovative technologies, the service quality can increase and, at the same time, resident and staff satisfaction improve. In this context, it is also important to personalize the human–robot interaction by endowing the robot with human-like social skills (i.e., natural language processing, user emotion estimation, etc.) [84][85].
3.5. Discussion: Pros and Cons of Different Technologies
The recent advancement in technological developments has made a wide variety of sensors available, even at a low cost, such as wearable rings, bracelets, smart watches, and mobile phones, for monitoring many functional parameters that are related to people’s health and activities. These sensors have to be worn and they may not be accepted by older people. Less intrusive sensors can be introduced in intelligent dresses and, together with antennas placed in the environment, can provide information for the detection of people. Other more complex sensors for monitoring vital signs are, at the moment, in an experimental phase and, although they have been shown to be effective in experimental tests, they must be miniaturized for being acceptable as wearable devices or have to be used for disease monitoring with a conscious involvement. Environmental sensors that are based on optical or microwave technologies are less invasive for people and they have been demonstrated to be robust for both activity detection and vital sign monitoring. They have to be placed properly in the environment and they may require infrastructure changes for their installation. Smart objects or sensors in furniture can be used to monitor daily life activities and interactions with objects. Additionally, in this case, some of the proposed solutions only require the addition of IoT sensors to the furniture that is already available; in other cases, it is necessary to replace objects with smart ones. A large number of sensors could be installed at different locations of the elderly people’s residence or house [86] depending on the specific parameters that have to be measured and the particular events that would be monitored. The selection of sensors among all of these possibilities depend on several factors: the costs of the sensors, their intrusiveness, their acceptability from users, the level of intervention that is required in the environments, the privacy issues that are related to the use of each sensor, and so on. Because these sensors have widely demonstrated their usefulness and potentialities, in the future they are certainly going to become of ordinary use. Thus, not only will the wearable sensors be a part of everyday life, but the environmental ones, even if they require structural interventions, will also be given in the new residences, thus making the flats and all the furniture smart.
References
- Ramkumar, M.O.; Catharin, S.; Nivetha, D. Survey of Cognitive Assisted Living Ambient System Using Ambient Intelligence as a Companion. In Proceedings of the IEEE International Conference on System Computation, Automation and Networking (ICSCAN), Pondicherry, India, 29–30 March 2019.
- Geman, O.; Costin, H. Automatic assessing of tremor severity using non linear dynamics artificial neural networks and neurofuzzy classifier. Adv. Electr. Comput. Eng. 2014, 12, 133–138.
- Yamine, J.; Prini, A.; Lavit, N.M.; Dinon, T.; Giberti, H.; Malosio, M. A Planar Parallel Device for Neurorehabilitation. Robotics 2020, 9, 104.
- Martirano, L.; Mitolo, M. Building Automation and Control Systems (BACS): A Review. In Proceedings of the IEEE International Conference on Environment and Electrical Engineering and 2020 IEEE Industrial and Commercial Power Systems Europe (EEEIC/I& CPS Europe), Madrid, Spain, 9–12 June 2020.
- Wozniak, M.; Połap, D. Intelligent Home Systems for Ubiquitous User Support by Using Neural Networks and Rule-Based Approach. IEEE Trans. Ind. Inf. 2020, 16, 2651–2658.
- Population Structure and Ageing. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php (accessed on 1 March 2021).
- Marinescu, I.A.; Bajenaru, L.; Dobre, C. Conceptual Approaches in Quality of Life Assessment for the Elderly. In Proceedings of the IEEE 16th International Conference on Embedded and Ubiquitous Computing (EUC), Bucharest, Romania, 29–31 October 2018.
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology 2016, 17, 567–580.
- Li, R.; Lu, B.; McDonald-Maie, K.D. Cognitive assisted living ambient system: A survey. Digit. Commun. Netw. 2015, 1, 229–252.
- Sanchez-Comas, A.; Synnes, K.; Hallberg, J. Hardware for Recognition of Human Activities: A Review of Smart Home and AAL Related Technologies. Sensors 2020, 20, 4227.
- Helbostad, J.L.; Vereijken, B.; Becker, C.; Todd, C.; Taraldsen, K.; Pijnappels, M.; Aminian, K.; Mellone, S. Mobile Health Applications to Promote Active and Healthy Ageing. Sensors 2017, 17, 622.
- Uddin, M.Z.; Khaksar, W.; Torresen, J. Ambient Sensors for Elderly Care and Independent Living: A Survey. Sensors 2018, 18, 2027.
- Stavropoulos, T.G.; Papastergiou, A.; Mpaltadoros, L.; Nikolopoulos, S.; Kompatsiaris, I. IoT Wearable Sensors and Devices in Elderly Care: A Literature Review. Sensors 2020, 20, 2826.
- Maskeliunas, R.; Damasevicius, R.; Segal, S. A Review of Internet of Things Technologies for Ambient Assisted Living Environments. Future Internet 2019, 11, 259.
- Climent-Perez, P.; Spinsante, S.; Mihailidis, A.; Florez-Revuelta, F. A review on video-based active and assisted living technologies for automated lifelogging. Expert Syst. Appl. 2020, 139, 112847.
- Amina, E.; Anouar, A.; Abdellah, T.; Abderahim, T. Ambient Assisted living system’s models and architectures: A survey of the state of the art. J. King Saud-Univ. Comput. Inf. Sci. 2020, 32, 1–10.
- Lee, S.B.; Oh, J.H.; Ho Park, J.; Choi, S.P.; Wee, J.H. Differences in youngest-old, middle-old, and oldest-old patients who visit the emergency department. Clin. Exp. Emerg. Med. 2018, 5, 249–255.
- Cattelani, L.; Belvederi Murri, M.; Chesani, F.; Chiari, L.; Bandinelli, S.; Palumbo, P. Risk Prediction Model for Late Life Depression: Development and Validation on Three Large European Datasets. IEEE J. Biomed. Health Inform. 2019, 23, 2196–2204.
- Alhomsan, M.N.; Hossain, M.A.; Mizanur Rahman, S.M.; Masud, M. Situation Awareness in Ambient Assisted Living for Smart Healthcare. IEEE Access 2017, 5, 20716–20725.
- Nastac, D.I.; Arsene, O.; Dragoi, M.; Stanciu, I.D.; Mocanu, I. An AAL scenario involving automatic data collection and robotic manipulation. In Proceedings of the 3rd IET International Conference on Technologies for Active and Assisted Living (TechAAL), London, UK, 25 March 2019.
- Parvin, P.; Paternó, F.; Chessa, S. Anomaly Detection in the Elderly Daily Behavior. In Proceedings of the 14th International Conference on Intelligent Environments, Rome, Italy, 25–28 June 2018.
- Fernandes, C.D.; Depari, A.; Sisinni, E.; Ferrari, P.; Flammini, A.; Rinaldi, S.; Pasetti, M. Hybrid indoor and outdoor localization for elderly care applications with LoRaWAN. In Proceedings of the IEEE International Symposium on Medical Measurements and Applications (MeMeA), Bari, Italy, 1 June–1 July 2020.
- Activage. Available online: https://www.activeageproject.eu (accessed on 20 February 2021).
- Hlicopter. Available online: http://www.helicopter-aal-eu (accessed on 20 February 2021).
- Konstadinidou, A.; Kaklanis, N.; Paliokas, I.; Tzovaras, D. A unified cloud-based framework for AAL services provision to elderly with cognitive impairments. In Proceedings of the 7th IEEE International Conference on Cognitive Infocommunications (CogInfoCom), Wroclaw, Poland, 16–18 October 2016.
- Casaccia, S.; Bevilacqua, R.; Scalise, L.; Revel, G.M.; Astell, A.J.; Spinsante, S.; Rossi, L. Assistive sensor-based technology driven self-management for building resilience among people with early stage cognitive impairment. In Proceedings of the IEEE International Symposium on Measurements & Networking (M&N), Catania, Italy, 8–10 July 2019.
- Pierleoni, P.; Belli, A.; Palma, L.; Paoletti, M.; Raggiunto, S.; Pinti, F. Postural stability evaluation using wearable wireless sensor. In Proceedings of the IEEE 23rd International Symposium on Consumer Technologies (ISCT), Ancona, Italy, 19–21 June 2019.
- Andó, B.; Baglio, S.; Lombardo, C.O.; Marletta, V. A Multisensor Data-Fusion Approach for ADL and Fall classification. IEEE Trans. Instrum. Meas. 2016, 65, 1960–1967.
- Badgujar, S.; Pillai, A.S. Fall Detection for Elderly People using Machine Learning. In Proceedings of the 11th International Conference on Computing, Communication and Networking Technologies (ICCCNT), Kharagpur, India, 1–3 July 2020.
- Xie, J.; Guo, K.; Zhou, Z.; Yan, Y.; Yang, P. ART: Adaptive and Real-time Fall Detection Using COTS Smart Watch. In Proceedings of the 6th International Conference on Big Data Computing and Communications (BIGCOM), Deqing, China, 24–25 July 2020.
- Nouredanesh, M.; Gordt, K.; Schwenk, M.; Tung, J. Automated Detection of Multidirectional Compensatory Balance Reactions: A Step Towards Tracking Naturally Occurring Near Falls. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 478–487.
- Sarabia, D.; Usach, R.; Palau, C.; Esteve, M. Highly-Efficient Fog-Based Deep Learning Aal Fall Detection System. Internet Things 2020, 11, 100185.
- Ur Rehman, R.Z.; Buckley, C.; Micó-Amigo, M.E.; Kirk, C.; Dunne-Willows, M.; Mazzá, C.; Qing Shi, J.; Alcock, L.; Rochester, L.; Del Din, S. Accelerometry-Based Digital Gait Characteristics for Classification of Parkinson’s Disease: What Counts? IEEE Open J. Eng. Med. Biol. 2020, 1, 65–73.
- Lutze, R. Practicality of Smartwatch Apps for Supporting Elderly People—A Comprehensive Survey. In Proceedings of the IEEE International Conference on Engineering, Technology and Innovation (ICE/ITMC), Stuttgart, Germany, 17–20 June 2018.
- Andó, B.; Baglio, S.; Lombardo, C.O.; Marletta, V. An Event Polarized Paradigm for ADL Detection in AAL Context. IEEE Trans. Instrum. Meas. 2015, 64, 1814–1825.
- Haghi, M.; Geissler, A.; Fleischer, H.; Stoll, N.; Thurow, K. Ubiqsense: A Personal Wearable in Ambient Parameters Monitoring based on IoT Platform. In Proceedings of the International Conference on Sensing and Instrumentation in IoT Era (ISSI), Lisbon, Portugal, 29–30 August 2019.
- Amendola, S.; Bianchi, L.; Marrocco, G. Movement detection of human body segments: Passive radio-frequency identification and machine-learning technologies. IEEE Antennas Propag. Mag. 2015, 57, 23–37.
- Paolini, G.; Masotti, D.; Antoniazzi, F.; Cinotti, T.S.; Costanzo, A. Fall Detection and 3-D Indoor Localization by a Custom RFID Reader Embedded in a Smart e-Health Platform. IEEE Trans. Microw. Theory Tech. 2019, 67, 5329–5339.
- Ozgit, D.; Butler, T.; Oluwasanya, P.W.; Occhipinti, L.G.; Hiralal, P. “Wear and Forget” patch for ambient assisted living. In Proceedings of the IEEE International Conference on Flexible and Printable Sensors and Systems (FLEPS), Glasgow, UK, 8–10 July 2019.
- Rajamohanan, D.; Hariharan, B.; Unnikrishna Menon, K.A. Survey on Smart Health Management using BLE and BLE Beacons. In Proceedings of the 9th International Symposium on Embedded Computing and System Design (ISED), Kollam, India, 13–14 December 2019.
- Zambrano-Montenegro, D.; García-Bermúdez, R.; Bellido-Outeirino, F.J.; Flores-Arias, J.M.; Huhn, A. An approach to beacons-based location for AAL systems in broadband communication constrained scenarios. In Proceedings of the IEEE 8th International Conference on Consumer Electronics—Berlin (ICCE-Berlin), Berlin, Germany, 2–5 September 2018.
- Ciabattoni, L.; Foresi, G.; Monteriù, A.; Pepa, L.; Pagnotta, D.P.; Spalazzi, L.; Verdini, F. Real time indoor localization integrating a model based pedestrian dead reckoning on smartphone and BLE beacons. J. Ambient Intell. Humaniz. Comput. 2019, 10, 1–12.
- Morita, T.; Taki, K.; Fujimoto, M.; Suwa, H.; Arakawa, Y.; Yasumoto, K. BLE Beacon-based Activity Monitoring System toward Automatic Generation of Daily Report. In Proceedings of the IEEE International Conference on Pervasive Computing and Communications (PerCom 2018), Athens, Greece, 19–23 March 2018.
- Cocconcelli, F.; Mora, N.; Matrella, G.; Ciampolini, P. Seismocardiography-based detection of heartbeats for continuous monitoring of vital signs. In Proceedings of the 11th Computer Science and Electronic Engineering (CEEC), Colchester, UK, 18–20 September 2019.
- Mora, N.; Cocconcelli, F.; Matrella, G.; Ciampolini, P. Fully Automated Annotation of Seismocardiogram for Noninvasive Vital Sign Measurements. IEEE Trans. Instrum. Meas. 2020, 69, 1241–1250.
- Andrushevich, A.; Biallas, M.; Kistler, R.; Ruminski, J.; Bujnowski, A.; Wtorek, J. Open smart glasses development platform for AAL applications. In Proceedings of the Global Internet of Things Summit (GIoTS), Geneva, Switzerland, 6–9 June 2017.
- Wan, J.; Byrne, C.A.; O’Grady, M.J.; O’Hare, G.M.P. Managing Wandering Risk in People With Dementia. IEEE Trans. Hum. Mach. Syst. 2015, 45, 819–823.
- Garcia, A.C.B.; Vivacqua, A.S.; Sánchez-Pi, N.; Martí, L.; Molina, J.M. Crowd-Based Ambient Assisted Living to Monitor the Elderly’s Health Outdoors. IEEE Softw. 2017, 34, 53–57.
- Mancini, A.; Frontoni, E.; Zingaretti, P. Embedded Multisensor System for Safe Point-to-Point Navigation of Impaired Users. IEEE Trans. Intell. Transp. Syst. 2015, 16, 3543–3555.
- Garcia-Magarino, I.; Lacuesta, R.; Lloret, J. Agent-Based Simulation of Smart Beds With Internet-of-Things for Exploring Big Data Analytics. IEEE Access 2018, 6, 366–379.
- Koutli, M.; Theologou, N.; Tryferidis, A.; Tzovaras, D. Abnormal Behavior Detection for Elderly People Living Alone Leveraging IoT Sensors. In Proceedings of the IEEE 19th International Conference on Bioinformatics and Bioengineering (BIBE), Athens, Greece, 28–30 October 2019.
- Kristaly, D.M.; Moraru, S.A.; Neamiu, F.O.; Ingureanau, D.E. Assistive Monitoirng System Inside a Smart House. In Proceedings of the International Symposium in Sensing and Instrumentation in IoT Era (ISSI), Shanghai, China, 6–7 September 2018.
- Su Keum, S.; Hwan Lee, C.; Ju Kang, S. Device to Device Collaboration Architecture for Real- Time Identification of User and Abnormal Activities in Home. In Proceedings of the 29th International Telecommunication Networks and Applications Conference (ITNAC), Auckland, New Zealand, 27–29 November 2019.
- Bassoli, M.; Bianchi, V.; De Munari, I.; Ciampolini, P. An IoT Approach for an AAL Wi-Fi-Based Monitoring System. IEEE Trans. Instrum. Meas. 2017, 66, 3200–3209.
- Bianchi, V.; Ciampolini, P.; De Munari, I. RSSI-Based Indoor Localization and Identification for ZigBee Wireless Sensor Networks in Smart Homes. IEEE Trans. Instrum. Meas. 2019, 6, 566–575.
- Jayatilaka, A.; Su, Y.; Ranasinghe, D.C. HoTAAL: Home of social things meet ambient assisted living. In Proceedings of the IEEE International Conference on Pervasive Computing and Communication Workshops, Sydney, NSW, Australia, 14–18 March 2016.
- Pavlicevic, N.; Zaric, N.; Radonjic, M. Analysis of Ultrasound Sensor Applicability in AAL Systems for Cooking Process Monitoring. In Proceedings of the 24th International Conference on Information Technology (IT), Zabljak, Montenegro, 18–22 February 2020.
- Rafferty, J.; Nugent, C.D.; Liu, J.; Chen, L. From Activity Recognition to Intention Recognition for Assisted Living Within Smart Homes. IEEE Trans. Hum. Mach. Syst. 2017, 47, 368–379.
- Yoo, B.; Muralidharan, S.; Lee, C.; Lee, J.; Ko, H. KLog-Home: A Holistic Approach of In-Situ Monitoring in Elderly-Care Home. In Proceedings of the IEEE International Conference on Computational Science and Engineering (CSE) and IEEE International Conference on Embedded and Ubiquitous Computing (EUC), New York, NY, USA, 1–3 August 2019.
- Malik, A.R.; Pilon, L.; Boger, J. Development of a Smart Seat Cushion for Heart Rate Monitoring Using Ballistocardiography. In Proceedings of the IEEE International Conference on Computational Science and Engineering (CSE) and IEEE International Conference on Embedded and Ubiquitous Computing (EUC), New York, NY, USA, 1–3 August 2019.
- Muheidat, F.; Tawalbeh, L. In-Home Floor Based Sensor System-Smart Carpet to Facilitate Healthy Aging in Place (AIP). IEEE Access 2020, 8, 178627.
- Oguntala, G.A.; Abd-Alhameed, R.A.; Ali, N.T.; Hu, Y.F.; Noras, J.M.; Eya, N.N.; Elfergani, I.; Rodriguez, J. SmartWall Novel RFID-Enabled Ambient Human Activity Recognition Using Machine Learning for Unobtrusive Health Monitoring. IEEE Access 2019, 7, 68022–68033.
- Shirali, M.; Norouzi, M.; Ghassemian, M.; Jai-Persad, D. A Testbed Evaluation for an Indoor Temperature Monitoring System in Smart Homes. In Proceedings of the IEEE 20th International Conference on High Performance Computing and Communications, Exeter, UK, 28–30 June 2018.
- Veiga, A.; García, L.; Parra, L.; Lloret, J.; Augele, V. An IoT-based Smart Pillow for Sleep Quality Monitoring in AAL Environments. In Proceedings of the Third International Conference on Fog and Mobile Edge Computing (FMEC), Barcelona, Spain, 23–26 April 2018.
- Scalise, L.; Petrini, V.; Di Mattia, V.; Russo, P.; De Leo, A.; Manfredi, G.; Cerri, G. Multiparameter electromagnetic sensor for AAL indoor measurement of the respiration rate and position of a subject. In Proceedings of the IEEE International Instrumentation and Measurement Technology Conference (I2MTC), Pisa, Italy, 11–14 May 2015.
- Bleda-Tomas, A.L.; Maestre-Ferriz, R.; Beteta-Medina, M.Á.; Vidal-Poveda, J.A. AmICare: Ambient Intelligent and Assistive System for Caregivers support. In Proceedings of the IEEE 16th International Conference on Embedded and Ubiquitous Computing (EUC), Bucharest, Romania, 29–31 October 2018.
- Fanti, M.P.; Faraut, G.; Lesage, J.J.; Roccotelli, M. An Integrated Framework for Binary Sensor Placement and Inhabitants Location Tracking. IEEE Trans. Syst. Man Cybern. Syst. 2018, 48, 154–160.
- De, P.; Chatterjee, A.; Rakshit, A. PIR Sensor based AAL Tool for Human Movement Detection: Modified MCP based Dictionary Learning Approach. IEEE Trans. Instrum. Meas. 2020, 69, 7377–7385.
- Jimenez, A.R.; Seco, F.; Peltola, P.; Espinilla, M. Location of persons using binary sensors and BLE beacons for ambient assitive living. In Proceedings of the 2018 International Conference on Indoor Positioning and Indoor Navigation (IPIN), Nantes, France, 24–27 September 2018.
- Guerra, C.; Bianchi, V.; De Munari, I.; Ciampolini, P. CARDEAGate: Low-cost, ZigBee-based localization and identification for AAL purposes. In Proceedings of the IEEE International Instrumentation and Measurement Technology Conference (I2MTC) Proceedings, Pisa, Italy, 11–14 May 2015.
- Chen, S. Toward Ambient Assistance: A Spatially aware Virtual Assistant eNabled by object detection. In Proceedings of the International Conference on Computer Engineering and Application (ICCEA), Guangzhou, China, 18–20 March 2020.
- Yue, S.; Yang, Y.; Wang, H.; Rahul, H.; Katabi, D. BodyCompass: Monitoring Sleep Posture with Wireless Signals. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2020, 4, 1–25.
- Fan, L.; Li, T.; Yuan, Y.; Katabi, D. In-Home Daily-Life Captioning Using Radio Signals. Computer Science—ECCV. arXiv 2020, arXiv:2008.10966.
- Vahia, V.; Kabelac, Z.; YuHsu, C.; Forester, B.; Monette, P.; May, R.; Hobbs, K.; Munir, U.; Hoti, K.; Katabi, D. Radio Signal Sensing and Signal Processing to Monitor Behavioral Symptoms in Dementia: A Case Study. Am. J. Geriatr. Psychiatry 2020, 28, 820–825.
- Li, L.; Shuang, Y.; Ma, Q.; Li, H.; Zhao, H.; Wei, M.L.; Liu, C.; Hao, C.; Qiu, C.; Cui, T. Intelligent metasurface imager and recognizer. Light Sci. Appl. 2019, 8, 97.
- Del Hougne, P.; Imani, M.; Diebold, A.; Horstmeyer, R.; Smith, D. Learned Integrated Sensing Pipeline: Reconfigurable Metasurface Transceivers as Trainable Physical Layer in an Artificial Neural Network. Adv. Sci. 2020, 7, 1901913.
- Li, H.Y.; Zhao, H.T.; Wei, M.L.; Ruan, H.X.; Shuang, Y.; Cui, T.J.; del Hougne, P.; Li, L. Intelligent Electromagnetic Sensing with Learnable Data Acquisition and Processing. Patterns 2020, 1, 100006.
- Cebanov, I.; Dobre, C.; Gradinar, A.; Ciobanu, R.I.; Stanciu, V.D. Activity Recognition for Ambient Assisted Living using off-the shelf Motion sensing input devices. In Proceedings of the Global IoT Summit (GIoTS), Aarhus, Denmark, 17–21 June 2019.
- Ryselis, K.; Petkus, T.; Blazauskas, T.; Maskeliunas, R.; Damasevicius, R. Multiple Kinect based system to monitor and analyze key performance indicators of physical training. Hum. Centr. Comput. Inf. Sci. 2020, 10, 51.
- Thamil Amudhu, L.B. A review on the use of socially assistive robots in education and elderly care. Mater. Today Proc. 2020, in press.
- Hasenauer, R.; Belviso, C.; Ehrenmueller, I. New Efficiency: Introducing Social Assistive Robots in Social Eldercare Organizations. In Proceedings of the IEEE International Symposium on Innovation and Entrepreneurship (TEMS-ISIE), Hangzhou, China, 24–26 October 2019.
- Kearney, K.T.; Presenza, D.; Saccá, F.; Wright, P. Key challenges for developing a Socially Assistive Robotic (SAR) solution for the health sector. In Proceedings of the IEEE 23rd International Workshop on Computer Aided Modeling and Design of Communication Links and Networks (CAMAD), Barcelona, Spain, 17–19 September 2018.
- Ramdani, N.; Panayides, A.; Karamousadakis, M.; Mellado, M.; Lopez, R.; Christophorou, C.; Rebiai, M.; Blouin, M.; Vellidou, E.; Koutsouris, D. A Safe, Efficient and Integrated Indoor Robotic Fleet for Logistic Applications in Healthcare and Commercial Spaces: The ENDORSE Concept. In Proceedings of the 20th IEEE International Conference on Mobile Data Management (MDM), Hong Kong, China, 10–13 June 2019.
- Bui, H.D.; Chong, N.Y. An Integrated Approach to Human-Robot-Smart Environment Interaction Interface for Ambient Assisted Living. In Proceedings of the IEEE Workshp on Advanced Robotics and Its Social Impacts (ARSO), Genova, Italy, 27–29 September 2018.
- Loghmani, M.R.; Patten, T.; Vincze, M. Towards Socially Assistive Robots for Elderly. An End-to-end Object Search Framework. In Proceedings of the IEEE International Conference on Pervasive Computing and Communications Workshops (PerCom Workshops), Athens, Greece, 19–23 March 2018.
- Lloret, J.; Canovas, A.; Sendra, S.; Parra, L. A smart communication architecture for ambient assisted living. IEEE Commun. Mag. 2015, 53, 26–33.
More
