In patients undergoing diagnostic coronary angiography (CA) and percutaneous coronary interventions (PCI), the benefits associated with radial access compared with the femoral access approach remain controversial. Radial access in patients undergoing CA with or without PCI is associated with lower mortality, MACE, major bleeding and vascular complications, irrespective of clinical presentation, ACS or STEMI, compared with femoral access.
- femoral
- radial
- coronarography
- PCI
- acute coronary syndrome
- stable coronary artery disease
1. Introduction
Patients with coronary artery disease (CAD) typically present with chest pain or shortness of breath. In patients with stable or unstable CAD, coronary angiography (CA), as the gold standard for detection and assessment of coronary artery stenoses, is performed, according to current clinical guidelines [1]. Revascularization therapy is indicated in patients with acute coronary syndrome (ACS) and in those with confirmed significant coronary stenosis not responding to optimal medical therapy or demonstrating marked limitation of physical activity [1]. Percutaneous coronary intervention (PCI), as an alternative to coronary artery bypass graft surgery, was introduced in the 1990s and is currently performed as a revascularization tool in the majority of patients with CAD [2]. The traditional approach for CA and PCI has been through the femoral artery, owing to its large caliber, which provides easy access [3]. Bleeding is the most common complication of PCI and is associated with poor clinical outcomes [4][5][4,5]. However, since 1989, the trans-radial approach has been attempted as an alternative to femoral access [6] and has resulted in less access-site bleeding due to the easily compressible radial artery; the superficial anatomy of the radial artery also encourages early patient discharge after procedures [7]. However, the radial approach for diagnostic CA and PCI requires a longer learning curve and higher procedure volumes in order to achieve adequate and safe skills. Over the last decades, several published randomized clinical trials (RCTs) assessed the value of the radial compared with the femoral approach in patients undergoing diagnostic CA and PCI with respect to residual ischemic, bleeding, and combined outcomes. The results of these RCTs remain controversial.
2. Radial Access for Coronary Angiography Compared with Femoral Access
2.1. Patients with Acute Coronary Syndrome (ACS)
All-cause mortality was reported in all 18 trials. All-cause mortality occurred in 179 patients (1.7%) assigned to the radial approach and in 245 patients (2.3%) assigned to the femoral approach at the latest follow-up. All-cause mortality was lower in patients assigned to the radial approach compared to those assigned to the femoral approach (RR: 0.73; 95% CI: 0.61 to 0.89; p = 0.001.
Major bleeding was reported in 17/18 RCTs, having occurred in 573 patients (5.1%) assigned to the radial approach and in 984 patients (9.3%) assigned to the femoral approach.
MACE was reported in all 18 included RCTs, in which 542 patients (6.7%) were assigned to the radial approach and 657 patients (8%)were assigned to the femoral approach at the latest follow-up. MACE were fewer in patients assigned to the radial approach compared to those assigned to the femoral approach.
Major vascular complications were reported in 16/18 RCTs, having occurred in 132 patients (1.3%) assigned to the radial approach and 308 patients (2.9%) assigned to the femoral approach at the latest follow-up. Major vascular complications were less in patients assigned to the radial approach compared to those assigned to the femoral approach.
Myocardial infarction was reported in 17/18 RCTs, having occurred in 392 patients (3.7%) assigned to the radial approach and in 432 patients (4.1%) assigned to the femoral approach at the latest follow-up. Myocardial infarction was not different between patients assigned to the radial compared to the femoral approach.
Stroke was reported in 11/18 included RCTs. Stroke occurred in 62 patients (0.6%) assigned to the radial approach and in 51 patients (0.5%) assigned to the femoral approach at the latest follow-up. Stroke was not different between patients assigned to the radial approach compared to those assigned to the femoral approach.
2.2. Patients with STEMI
All-cause mortality was reported in all 14 trials, having occurred in 124 patients (2.3%) assigned to the radial approach and in 181 patients (3.2%) assigned to the femoral approach at the latest follow-up. All-cause mortality was lower in patients assigned to the radial approach compared to those assigned to the femoral approach.
Major bleeding was reported in all 14 included RCTs, with 46 patients (1.3%) assigned to radial approach and 95 patients (2.7%) assigned to femoral approach at the latest follow-up. Major bleeding was lower in patients assigned to the radial approach compared to those assigned to the femoral approach.
MACE was reported in all 14 included RCTs, having occurred in 265 patients (4.8%) assigned to the radial approach and in 319 patients (5.7%) assigned to the femoral approach at the latest follow-up. MACE was less in patients assigned to the radial approach compared to those assigned to the femoral approach.
Major vascular complications were reported in 13/14 RCTs, with 71 patients (2.1%) assigned to the radial approach and 148 patients (4.2%) assigned to the femoral approach at the latest follow-up. Major vascular complications were fewer in patients assigned to the radial approach compared to those assigned to the femoral approach.
Myocardial infarction was reported in 13/14 RCTs, having occurred in 33 patients (1.3%) assigned to the radial approach and in 35 patients (1.4%) assigned to the femoral approach at the latest follow-up. Myocardial infarction was not different between patients assigned to the radial compared to the femoral approach.
Stroke was reported in 10/14 included RCTs, with 19 patients (0.8%) assigned to the radial approach and 14 patients (0.6%) assigned to the femoral approach at the latest follow-up. Stroke was not different between patients assigned to the radial compared to the femoral approach.
3. Summary
(1) The use of radial access compared with femoral access was associated with a significant 26% relative risk reduction in all-cause mortality and 47% relative risk reduction in major bleeding in all patients undergoing CA. The risk reduction was also demonstrated irrespective of the clinical presentation of ACS (27% and 37%, respectively) or STEMI (31% and 43%, respectively). (2) The use of radial access was associated with 18% fewer MACE and 63% fewermajor vascular complications. Again, the radial approach was associated with lower risk of MACE, irrespective of clinical presentation of ACS (17% and 56%, respectively) or STEMI (16% and 52%, respectively) (Figure 14). (3) There was no significant difference in myocardial infarction and stroke between patients assigned to radial approachwith respect to those assigned to the femoral approach in the two subgroups with ACS or STEMI (Figure 14).
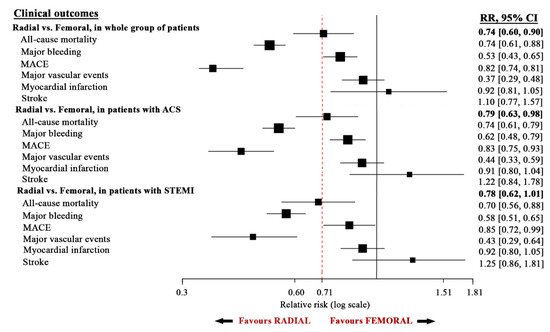
Figure 14.
Summary of outcome in all study groups.
Coronary angiography and PCI procedures are used in the diagnosis and management of CAD [8][49]. The traditional approach for CA and PCI, from their introduction, has been through the femoral artery, based on the easy access it offers due to the large caliber [3]. The transfemoral approach for CA and PCI gained widespread acceptance by operators because of the following advantages: long history of use, easy technicality, and the ability of clinicians to use larger catheters and equipment for various interventions [9][50]. However, the femoral catheterization approach has some disadvantages, including the need for patients’ prolonged bed rest, which could be associated with back pain, urinary retention, and neuropathy, particularly in the elderly [6][10][11][6,51,52],as well as prolonged arterial compression related complications, e.g., peripheral ischemia.
Such advantages could be explained on the basis of reduced limb-threatening ischemia, less need for lying flat (e.g., due to back pain, obesity, or congestive heart failure), and earlier patient discharge. The reduced limb-threatening ischemia could be explained on the basis of a lower likelihood of radial atherosclerosis disease, which is disease known to affect femoral arteries [12][53]. The technique also does not cross the descending and thoracic aorta, which are known for their involvement in the process of atherosclerosis; hence, this process does not involve the potential thromboembolic complications of the femoral approach [12][53]. On the other hand, the main limitations of the trans-radial approach are the relatively smaller caliber [13][54], potential technical challenges in some patients, potential vessel spasm [13][54], longer procedure time requiring higher radiation [14][55] and a steep learning curve [15][16][56,57]. Despite these limitations, data from the last decades support the use of radial access as the default approach for CA and PCI in the whole spectrum of patients with suspected CAD who are undergoing invasive diagnosis and PCI.
