As a global pandemic, COVID-19 shows no sign of letting up. With the control of the epidemic in China, the proportion of patients with severe and critical diseases being cured and discharged from hospital has increased, and the recovery of COVID-19 patients has become an important issue that urgently needs attention and solutions. By summarizing the exercise rehabilitation strategies and progress of SARS in 2003, this paper analyzed the differences in clinical indicators and recovery characteristics of severe pneumonia caused by the two viruses, and provided comprehensive exercise guidance and intervention strategies for COVID-19 patients for rehabilitation and nursing by referring to the problems and treatment strategies in the rehabilitation and nursing work of SARS. In the post-epidemic period, China will build a multi-dimensional epidemic prevention system by improving the effectiveness of mass training and strengthening local risk prevention and control.
- SARS-CoV-2
- COVID-19
- convalescent patient
- clinical symptoms
- exercise rehabilitation
- integration of sports and medicine
1. Introduction
2. Patients with COVID-19 Were Treated with SARS Rehabilitation Protocol
2.1. Respiratory Function
2.2. Sports Ability
2.3. Psychological Situation
3. Implications for COVID-19 Exercise Rehabilitation in China
In combination with the pathological research results of COVID-19 in the medical field, relevant studies have elaborated the main principles of strengthening physical exercise to effectively prevent COVID-19 [30][57]. First of all, moderate physical exercise can promote blood circulation, let the immune cells timely transport and destroy the virus in the body, which is the main basis for physical exercise you effectively resist and contain coronavirus [31][58].Secondly, increasing the activity of angiotensin converting enzyme (ACE) in the renin-angiotensin system (RAS) during exercise improves the structural adaptability of coronary artery tree, which can effectively resist SARS-CoV-2 and play a positive role in the mechanism of acute myocardial injury caused by COVID-19 [32][59]. Third, sedentary living at home can lead to muscle fixation, damage and deterioration of mitochondrial stability, and cause organic and systemic inflammation, which is also an important mechanism of COVID-19 pathogenesis [33][60]. Finally, the study also confirmed that physical exercise effectively counteracts and reduces the negative effects of COVID-19 on people’s physical and mental health [34][35][5,61]. Lung function injury greatly reduced patients’ daily activity ability and fatigue degree, pulmonary rehabilitation training was urgently needed to restore the lung function. Liu et al. [36][62] conducted a 6-week respiratory exercise intervention and rehabilitation treatment on 36 elderly patients with COVID-19 who were over 65 years old without related basic diseases, and the results showed that respiratory exercise could effectively improve the patients’ respiratory function, quality of life and anxiety, providing an important reference for clinical treatment. Investigations showed that more than 75% of COVID-19 hospitalized patients required oxygen therapy, approximately 54% developed respiratory failure, and more than 30% required mechanical ventilation to maintain pulmonary gas exchange. However, prolonged mechanical ventilation can lead to atrophy of the diaphragm and rapid development of systolic dysfunction, leading to the risk of ventilator (diaphragm) weakness and difficulty in getting COVID-19 patients off the ventilator [37][63]. Participated in related studies have shown that advance moderate endurance exercise, the infection will be after the coronavirus to accept ventilator support, from the endurance exercise induced by the diaphragm preadaptation benefit, endurance exercise can increase the superoxide dismutase (SOD) in the diaphragmatic muscle mitochondrial protein 2 (SOD2) level and the amount of heat shock protein 72 in cytoplasmic protein, promote the diaphragm of biochemical changes, effectively resist COVID-19 induced sepsis complications related to [37][38][39][40][63,64,65,66]. One thing the needs to be noted is that, in nursing work, a large number of patients who were bedridden and receiving mechanical breathing needed to receive rehabilitation treatment on the basis of safety assessment. Before the formal implementation of sports rehabilitation training, it was necessary to evaluate the symptoms, sports ability, quality of life, mental state and other aspects. Bansal’s team [41][67] evaluated the performance of 20 adults with disordered breathing on an incremental cardiopulmonary exercise test. It found that VO2max was lower than average and that patients more frequently cited dyspnea as the cause of their exercise limitations. However, due to the specific cultural, historical and geographical background in China, the exercise rehabilitation of COVID-19 had its own requirements and characteristics. Similarly, the illness severity pattern was divided into four groups: asymptomatic infected patients, symptomatic patients isolating at home symptomatic patients admitted to hospital, and symptomatic patients requiring ventilator support in critical care. Here, we concluded COVID-19 patients’ exercise rehabilitation strategies in three stages of clinical treatment, restoration, and remote healthcare, and divided clinical patients into two groups of patients with mild disease, critically ill patients, and list specific exercise rehabilitation strategies recommendations accordingly in Figure 1.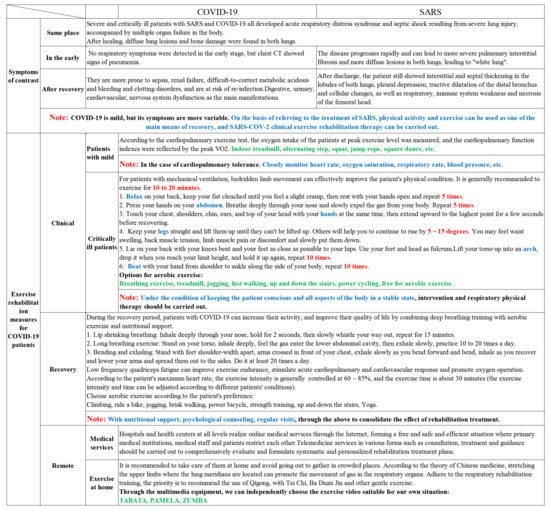
3.1. Clinical Exercise Rehabilitation Methods for COVID-19 Patients
- (1)
-
Relaxation training: lie flat on the bed, relax the whole body muscles, clench fists, feel the muscle tension in the fingers, knuckles, and palms, keep the movement until you feel a slight cramp, then open your hands to relax and rest, repeat five times.
- (2)
-
Abdominal breathing training: the patient presses his hands on the abdomen, and exercises with the abdomen when breathing, breathes deeply through the nose until it can’t breathe in, and then slowly and rhythmically expel the gas from the body, repeat five times.
- (3)
-
Upper limb elevation training: the patient touches the chest, shoulders, chin, ears, and top of the head with the index finger, and then stretches up to the highest point for a few seconds and then recovers, with both hands at the same time.
- (4)
-
Elevating lower limbs training: straighten legs and lift them up until fatigue, assisted by others to continue to rise by 5 to 15 degrees, when the patient feels waist soreness, back muscle tension, slight pain or discomfort, switch to the other leg.
- (5)
-
Hip bridge training: bend the knees in the supine position, put your feet close to your hips as much as possible, use your feet and head as the fulcrum, add elbows if necessary, lift up to arch, feel the extension of the waist and back, hips and lower limbs When you reach your limit height, put it down and hold it up again, repeat 10 times.
- (6)
-
Meridian patting training: the patient pats along the side of the body from shoulder to ankle in turn, alternating up and down, and repeats 10 times.
3.2. Exercise Rehabilitation Methods for COVID-19 Patients after Recovery
COVID-19 inpatients are often accompanied by related basic diseases [48][73], so it is important to remember to blindly carry out all kinds of respiratory supportive therapy. On the basis of clarifying the internal mechanism of respiratory exercise and COVID-19, it is an important field to strengthen the research on the intervention of respiratory rehabilitation exercise for patients with related basic diseases or induced complications, which needs to be deepened and solved urgently. The specific methods are as follows: (1) respiratory breathing: inhale deeply through your nose, hold for 2 seconds, and then slowly exhale through a whistle, repeat practice for 15 minutes; (2) long breathing exercises: stand up torso, relax the muscles, inhale deeply, feel the air enter the lower abdominal cavity, then exhale slowly, the slower the better, fully feel the process of the air leaving the lungs, trachea, and nasal cavity, practice 10~20 times every day; (3) bend and exhale exercise: stand with your feet shoulder-width apart, cross your arms in front of your chest, exhale slowly when you bend your body forward, and inhale when your arms fall and spread out to both sides when you recover, stick to it every day at least 20 times. Besides, abdominal breathing can be found in a variety of physical and mental exercises, which can enhance respiratory function, stimulate the vagus nerve and produce a relaxation response, including yoga, meditation and Qigong [49][50][74,75]. The technical operation of abdominal breathing is very simple. The subjects consciously move the stomach when inhaling, tighten the stomach muscles, and let them fall inward when exhaling with focusing on the breath and avoiding to hold your breath [36][62]. Before training, set the exercise intensity according to the patient’s maximum heart rate, generally controlled at 60–85%, and the exercise time is about 30 minutes (the exercise intensity and time can be adjusted appropriately according to the condition of different patients). During the exercise, the subjects should pay attention to control the heart rate to avoid dizziness, fatigue, shortness of breath, chest tightness, chest pain and other situations. If those situations happen, the exercise program should be stopped immediately. In severe cases, nitroglycerin and other drugs need to be applied.By cardiopulmonary exercise test (CPET), in the case of load increment, by breathing, circulation, nerve body fluids, such as the metabolic system of participation, patients from resting to gradually restore again to limit state motion data, including heart rate, blood pressure, ecg analysis, such as traditional information, and provide important data with oxygen metabolism as the core, such as: peak VO2 and minute ventilation/ carbon dioxide production (VE/VCO2) slope are used to describe in detail the physiological conditions of patients in exercise state through rich and comprehensive monitoring indicators [51][76]. Discharged patients still need to pay attention to protection from viruses to avoid secondary infections. After recovery, they will be left with varying degrees of respiratory damage and lung dysfunction, which may cause other organ complications impacting daily life. It is recommended that during the home care period, suitable exercise rehabilitation videos can be utilized on multimedia equipment to insist on carrying out breathing rehabilitation training, such as breathing exercises, Tai Chi, eight-section brocade Chi Kung, yoga and other light exercise training [21][52][49,77]. With nutritional support, psychological counseling, and regular follow-up visits, symptoms such as dyspnea, shortness of breath, consolidate can be alleviated, which helps to improve and promote respiratory function, immune system, and exercise capacity. The subjects need to make full use of family, community, and medical resources for systematic and scientific rehabilitation training to lay a solid foundation for returning to society as soon as possible.3.3. Remote Exercise Rehabilitation Methods for COVID-19 Patients
From the national incidence, about a quarter of the medical personnel are the direct victims of infectious disease. Epidemic prevention and control in the process of health care workers should pay attention to the cultivation of clinical thinking and judgment ability, concept not only stay on the disinfection, isolation and general knowledge, from the technical service extension to community service, and from the hospital service extension to the outside of the hospital service. The treatment and service will be placed in the same important position, penetration in the prevention, treatment, health care, rehabilitation and other aspects. Each country has also established the joint operation of “medical prescription” main attack and “exercise prescription” auxiliary attack. For example, the UK has established a national referral database and intervened in exercise prescription to strengthen the management and treatment of the national health condition [53][78]. The principles, content framework and minimum standard baseline for exercise for different populations were developed during the Australian pandemic [50][75]. Han University in the Netherlands has established an online service platform to provide the latest exercise prescription and programme support during the COVID-19 pandemic [54][79]. The United States has established a remote rehabilitation and testing system including COVID-19 physical and mental health and nursing services [55][80]. Japan makes use of TV, Internet, video and other technologies to produce the regular home version of the elderly’s physical function exercise prescription video [56][81]. Guidelines on physical activity based on social distance during COVID-19 in Korea [57][82]. The Chinese Association of Sports Science has scheduled to set up “Sports Health Promotion Centers” nationwide from 2020 to meet the public’s fitness needs and establish a library of traditional and popular exercise programs.The majority of the COVID-19 disease outbreak affected the elderly, the majority of which have heart, brain, liver, kidney and other organs complication, and studies have confirmed that traditional project prevention, treatment and rehabilitation for the elderly COVID-19 have a positive effect [58][83]. It can promote the recovery of respiratory symptoms, deep, rhythmic breathing and body movement with the concentration of slow, make people relaxed mood, pressure drops into a state of meditation, priority is recommended to use qigong to prevent COVID-19 improve infection after respiratory symptoms [59][84]. Qigong can increase the number and activity of human immune cells, reduce inflammatory factors and inflammatory responses in the body, and train specific muscle groups to enhance physical strength through exercise [60][61][85,86]. Choosing Ba Duan jin, Tai Chi such delicate, smooth, soft, light movement, slow body movements and musculoskeletal stretch should be combined with body relaxation, deep breathing and mental concentration, emphasize the balance of the body and breath free, drives the whole body movement to increase the health of the body.
