Since the pandemic induced by the coronavirus SARS-CoV2 began to be spread throughout the whole world, many medical attempts to control the infection and avoid the high rate of mortality and morbidity have been made, collapsing the ICUs of many Hospitals. Many different treatments have been tested, but mortality reached very high values, especially in people in the middle/ elder age. Survivors usually develop important sequelae, even time after the infection had been controlled. In this article, we propose two different approaches to avoid the infection or mitigate their effects. One of them is based in the administration of GH, as preventive, given its known effect on the production of lymphocytes and a high number of antibodies, as well as for helping in the recovery of the damaged organs. The other one is the administration of melatonin, both to prevent the infection and to act on inflammation once the disease is established. Both hormones are safe and can synergize when the damage to organs is established. GH administration has to be interrupted if the cytokine storm appears because the hormone can increase it. This is a novel approach that will be analyzed in extent, on scientific bases, throughout this article.
- Growth Hormone
- Melatonin
- SARS-CoV2
- COVID-19
- Lungs affectation
- Cardiovascular affectation
- Brain damage
- Thrombosis
- Hepatic damage
- Immunity.
1. Introduction
Since the end of 2019, a novel coronavirus knew as SARS-Cov-2 [1], apparently from bats, spread throughout the world producing a global pandemic, due to the high rate of replication of the virus once it enters into the oropharyngeal structures from where it diffuses into the human body and from where the virus infects other people through droplets of saliva expelled when speaking, sneezing, coughing and fomites. This virus exhibits high morbidity and mortality (in Spain more than 29.000 patients died until now, and there are no lesser than 260.000 infected from January to the end of May). Although the initial severe symptoms appeared restricted to lungs affectation (bilateral pneumonia preceding acute respiratory stress syndrome), necropsies revealed that the virus practically affected the whole human body, although the type and degree of affectations were very variable, as it is the number of people recovered from the disease, in spite that it is not clear what type of medical treatment is the most beneficial in each case. For instance, while initially, a combination of hydroxychloroquine, first used in the treatment of autoimmune diseases and malaria [2], antiseptic drugs, such as azithromycin, and antiviral agents, such as remdesivir appeared to be an effective treatment, also combined with corticosteroids, nitric oxide, vitamin C and Il-6 antagonists [3], and, of course, medical interventions in the case of patients in very bad conditions (ICU).
However, hydroxychloroquine, although approved by the US FDA for being used in the treatment of COVID-19, has many adverse effects, and it is contraindicated in patients with heart problems. Currently, a number of new antivirals are being tested, as well as the administration of plasma from patients who successfully overcome the disease, a technique that allowed to save the life of a woman infected by the Ebola virus a few years ago. Without any doubt, this plasma contains significant amounts of antibodies able to neutralize the virus, but it will be a difficult task to treat millions of patients throughout the world.
In children, it has been reported that the disease is much less frequent than in adults and that the majority of cases are benign or moderate (even with high viral loads), as long as there are no other risk factors or underlying diseases [4].
While a number of pharmaceutical companies are trying to develop an effective vaccine against the COVID-19, and two of them recently reported positive results and the absence of secondary effects, it is unlikely that this or these vaccines reach the commercial market before one year. Meanwhile, many patients will die or suffer irreparable sequelae.
The purpose of this manuscript is not to analyze new treatments, but to provide two novel alternative therapies as a benefit to increase natural immunity, not only preventively but also as an adjuvant to treatment when the disease is already established., far beyond of the use of masks, isolation, etc. It is possible that many readers will consider the idea that we will propose as a crazy idea, but we will try to detail the scientific bases that give rise to it.
Summarizing, before explaining the details, we propose the use of growth hormone (GH) and melatonin for preventing the infection and/or treating it when established.
2. Why GH?
Today it is well known that GH is a pleiotropic hormone able to carry out many positive functions in the human body, far beyond its classical effects on the linear growth of the organism and its metabolic effects. Here we will analyze shallowly the main positive, and negative, effects of the hormone on the prevention of the infection, and its effects on the tissues and organs that can be affected after infection by SARS-CoV2. The first step has to be related to the immune system.
2.1 GH and the immune system
2.1. GH and the immune system.
It is now well known that GH has a very important influence on the immune system. In cells of the immune system exists expression of GH and GHRH, who through autocrine/paracrine and intracrine pathways, but also endocrine, play a significant role in the immune function [5]. GH induces the maturation and activation of dendritic cells that, as antigen-presenting cells, participate in the immune response of the organism [6]. In this regard, GH is helped by IGF-I, also present in these cells, as its receptor. Therefore, the system GH/IGF-I induces lymphocyte growth and survival and maturation and activation of dendritic cells. Hence, lymphocyte GH is a very important mediator of cellular immune function mediated by the TH-1 pathway [7]. Cells of the immune system recognize the association of bacteria, viruses, and tumors, as an oxidative stress event against which GH and its receptor will fight to defend the cell against oxidative damage. This concept has been demonstrated by the group of Weigent [8].
However, the production of GH by cells of the immune system may not be important enough to cope with a major infection, such as that caused by SARS-CoV2. The lymphopenia detected in this disease is a clear exponent of this concept. In this case, the endocrine GH, or the exogenously administered hormone, would be needed, but the secretion of GH experiences important changes throughout the life. After birth, the maximal endogenous secretion of the hormone occurs during the first year of life, then there is a decrease until puberty, a stage in which the hormone reaches high values, but once the puberty ends, the endogenous secretion of the hormone begins to show a progressive exponential decrease, starting from 18 to 30 years of age, until being practically undetectable while the subject is aging (from 50-60 years old more or less). This may explain why the COVID-19 rarely affects children and it is particularly aggressive in elder people, although curiously people aged 90-100 years old have been able to recover from the disease, perhaps by genetic unknown reasons.
Recently, a very important pilot study carried out in California [9], demonstrated that the administration of GH for one year to healthy volunteers (aged 51- to 65-years old) was able to treatment regenerate the thymic functional mass, previously degenerated by thymic fat, as it occurs while aging, leading to a very significant increase in the lymphocyte to monocyte ratio, an effect that persisted 6 months after discontinuation of treatment. The researchers were impacted by the very significant increase in plasma immunoglobulins, which led to one of them to affirm that GH administration could be very useful for treating infections and even cancer. This means that GH exerts important actions on immunosenescence. In addition, as stated before, lymphocyte GH stimulates IFNγ production with a small positive effect on IL-10 production [7].
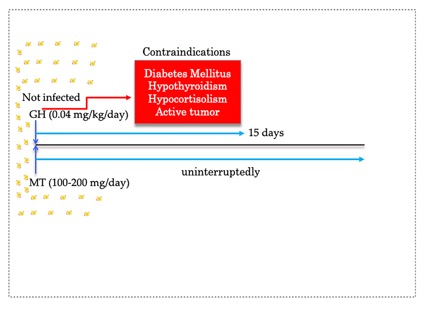
In all, it is likely that exogenous GH administration may act as a preventive factor against the infection by SARS-CoV2, at least in GH-deficient patients or elder people (Figure 1).
Figure 1. GH induces the formation of antibodies. In an environment where the possibility of SARS-Cov2 infection is high, the administration of GH can decrease the possibility that it occurs by increasing the production of lymphocytes and immunoglobulins. This administration can take place for about 15 days, more than the necessary time so that the production of antibodies is more than significant. GH doses depend on the age of the subject, although the standard dose used in children with GH deficiency is mentioned in the scheme, who should also be treated if they are not already but can reach up to 1 mg/day in people with 30-40 years and they can decrease to 0.4 mg/day in elderly people. The red arrow towards the red box indicates the contraindications for this administration of the hormone, although there are currently diabetic patients treated with insulin and GH. In the case of hypothyroidism or hypocortisolism, these must be controlled before GH can be administered. Therefore, the only real contraindication would be the existence of an active tumor. Yellow dots indicate the presence of SARS-CoV2 in the environment where the subject is performing his/her activities.
Figure 1 also shows, as it will be explained later, why Melatonin at doses ranging 100-200 mg/day (lesser in children, if needed), has to be given as a preventive factor, uninterruptedly until the risk of infection has fully disappeared.
2.2. GH effects in lungs
2.2. GH effects in lungs
Few are known about the GH effects on lungs, but most likely its effects depend on GH actions on respiratory muscle strength. In fact, reports indicate that adult patients suffering from childhood-onset GH deficiency develop impaired ventilation due to decreased lung volumes and respiratory pressures [10]. However, in severely ill patients it is not advisable to administrate GH because it can increase the cytokine storm and aggravate the situation.
2.3. GH and the cardiovascular system
2.3. GH and the cardiovascular system.
The many positive effects that GH plays in the cardiovascular system have been widely described by our group [11][12][13][14][11-14]. GH administration can help to recover cardiac failure, enhance angiogenesis and arteriogenesis, help to recover the damaged vascular endothelium. In the vascular system GH activates the nitric oxide (NO) system and regulates nonendothelial dependent actions: Given that NO production relaxes arterial smooth muscle cells vascular tone is reduced [11]: Moreover, GH decreases the possibility of the formation of thrombi, despite that many years ago it was described that elder men had more possibilities of developing thrombosis than elder women. However, GH lacks any effect on the platelet aggregation, although GH/IGF-I excess, as it occurs in acromegaly, have increased thrombosis risk by adversely affecting fibrin network characteristics, although it is not known whether this is a consequence of sustained GH hypersecretion for years or it depends on IGF-I [15].
In any case, GH should be administered in COVID-19 patients once the disease is controlled, unless there is a cardiac arrest. Given that these patients receive low molecular weight heparin the only risk of GH administration during the critical phase is, again, the possibility of potentiating the cytokine storm. In fact, many cases died two-three days after discharge presumably by a heart infarction.
2.4. GH and the Central Nervous System
2.4. GH and the Central Nervous System.
Many patients affected by SARS-CoV2 suffer very important brain damage, mainly as a consequence of multiple brain infarctions. GH plays a very important role in brain recovery after an injury, as it has been demonstrated by a number of studies from our [16][17][16,17] and other groups, acting as neuroprotective and neuroregenerative, even at the level of cranial pairs and modifying the turnover of important neurotransmitters (serotonin, noradrenaline, the dopaminergic system, the glutamatergic system, the opioid system, and the cholinergic system. Moreover, the hormone increases the number of arterioles and small vessels and increases the recruitment of the glucose receptor Glut4 [18]. But, as in the anterior descriptions of GH effects, it has to consider the condition of the patient before deciding whether to administer GH, which in any case could be given after discharge.
2.5. GH and Liver
2.5. GH and Liver.
As the damage that the SARS-CoV2 infection produced in the body became known, it was observed that the liver was one of the affected organs [19]. GH plays an important physiological role in hepatic triglyceride metabolism. Steatosis induces hepatic degeneration, which may be corrected by GH administration. Our group found that GH is expressed in the liver of hypophysectomized rats subjected to partial hepatectomy and that this GH promotes the hepatic regeneration, directly or by inducing HGF (Hepatic Growth Factor) expression [11]. Therefore, GH plays a very important function in non-alcoholic liver steatosis and perhaps in other liver diseases, as it could be produced by SARS-CoV2. Once again, the question would be: when GH should be given to these patients? Most likely the answer should be once they have surpassed the acute inflammatory phase of the disease.
2.6. GH and other organs and tissues
2.6. GH and other organs and tissues.
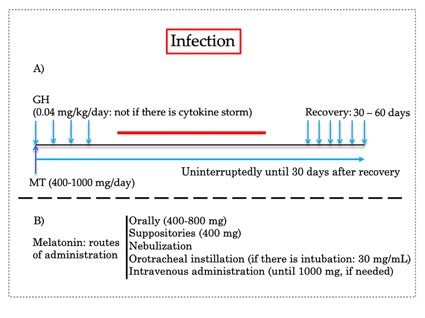
As stated before, COVID-19 produces many impairments in multi-organ function. Among them chronic kidney disease, gastrointestinal dysfunction, ocular risks, reproductive affectations, diabetes mellitus, sarcopenia, etc. Most of them, if not all, can be corrected after GH administration, but the hormone has to be given once the risk of cytokine storm had been controlled, otherwise, the risk of death is very high. But we can decrease the possibility of an infection by administering the hormone before the infection appeared and even in the first 2-3 days after it is detected, due to the ability of the hormone to increase the production of lymphocytes and immunoglobulins that could neutralize the virus (Figure 2A).
Figure 2. A) GH can be given in the early stages of the infection. Once the subject is infected, mild symptoms appear (fever, cough, etc). At this stage, GH could be administered for increasing the production of antibodies, which in fact begins to be present 4-7 days after the infection occurred. If the disease advances and the cytokine storm occurs, GH has to be interrupted (red line) because it would increase this cascade of cytokines production, putting in danger the life of the patient. Only in the case that a sudden urgent event occurs, such as cardiac infarction or brain damage, the responsible doctor should consider the need of administering GH (together with high doses of corticoids), given the known positive effects that the hormone exerts when given acutely after any of these emergencies. Once the patient is recovered and discharged, GH should be given during 30-60 days, for helping to recover the sequelae produced by the disease. B) High doses of melatonin have to be given forby the reasons soon explained. In Figure different routes of administration of this hormone are shown, depending on the situation of the patient. In the case of orotracheal instillation, since only 30 mg/mL are commercialized, there is the need toof repeat this administration 3-6 times/day. Intravenous administration is needed when severe sepsis exists.
3. Why Melatonin?
Until recent years, melatonin has been practically considered, by the majority of the medical class, as a hormone merely responsible for inducing sleep and act as a synchronizer between the organism and the environment. Perhaps this is the reason by which it can be found in drug stores, supermarkets, but at very low doses (1.9 mg – 10 mg), depending on the country. However, melatonin has many important and positive effects that can be observed at doses significantly higher. In our Medical Center, devoted to neurological rehabilitation, we are using melatonin since 2009, at doses ranging between 20 mg/capsule to 800 mg/capsule. During this time, 11 years, we treated more than 9.000 patients with many different neurological pathologies without observing any secondary adverse effect.
As it happens with GH, melatonin begins to be produced around two years old, and its secretion is maintained until the middle age of life, more or less, an age in which melatonin experiences a progressive decline until being practically undetectable in elder people. This may explain why elder people are more vulnerable when infected by SARS-CoV2, and also the reason for the lower incidence and severity among children infected by this virus.
Today we know that melatonin plays many different roles in the human body, acting as a potent antioxidant, mitochondrial protector, exerts anti-inflammatory actions by up-regulating anti-oxidative enzymes and downregulating pro-oxidative enzymes, and acts as a free radical scavenger [20]. Directly melatonin does not produce virus death, but this hormone has indirect anti-viral actions [20] due to its anti-inflammation, anti-oxidation, and immune-enhancing properties [21][22][23][24][21-24] (Figure 1). Given the known effects of melatonin on inflammation and decrease of circulating cytokine levels, as well as its positive effects in respiratory disorder models induced by infections, it is logical the deduction that its administration in the inflammatory phase of COVID-19 may be highly beneficial, as it has been recently demonstrated [25]. In fact, the NLRP3 inflammasome (a multiprotein complex of the innate immune system) plays a key role as initiator of the immune response during lung infection and the subsequent cascade of cytokines, a mechanism inactivated or reduced by melatonin [26]. Moreover, it has been postulated that mechanical ventilation increases inflammation in acute lung damage [27], and increased oxidative stress in the alveoli [28]. Hence, melatonin may solve a contradiction between the urgent clinical necessity to give patient mechanical ventilation and the threat this ventilation may possess [29]. Moreover, melatonin prevents lung[1][2][3][4][5][6][7][8][9][10][11][12][13][14][15][16][17][18][19][20][21][22][23][24][25][26][27][28][29] fibrosis in COVID-19 patients [29] and protects the heart and the brain after a sudden damaging event.
Due to this current knowledge about the effects of melatonin in COVID-19, a clinical trial began in the Hospital La Paz (Madrid, Spain, to study the efficacy of melatonin in the prophylaxis of COVID-19 among healthcare workers (Clinicaltrials.gov Identifier; NCT04353128), although the dose of melatonin they use is too low ( 2 mg/day).
A very worrying situation comes from the recent discovery that in Spain and other European countries has been identified a relatively high number of asymptomatic people with a positive number of SARS-CoV2 copies in their organism. Whether these people can be infectious remains unknown, as it is unknown if there are genetic reasons explaining this situation, but this reinforces our hypothesis about how to act for preventing infections by means of GH and melatonin.
References
- Zhou, Y.; Hou, Y.; Shen, J.; Huang, Y.; Martin, W.; Cheng, F. Network-based drug repurposing for novel coronavirus 2019-nCOV/SARS-CoV-2. Cell Disc. 2020, 6:14. ddddoi: 10.1038/s41421-020-0153-3. eCollection 2020.
- Rynes, R. Antimalarial drugs in the treatment of rheumatological diseases. Br J Rheumatol. 1997, 36, 799-805. doi: 10.1093/rheumatology/36.7.799.
- Wu, R.; Wang, L.; Dina Kuo, H-C,; Shannar A.; Peter, R.; Jordan Chou, P. et al. An Update on Current Therapeutic Drugs Treating COVID-19. Curr Pharmacol Rep. 2020, 1-15. doi: 10.1007/s40495-020-002-16-7. [Epub ahead of print].
- Dong, Y.; Mo, X.; Hu, Y.; Qi, X.; Jiang, Z. et al. Epidemiology of COvid-19 among Children in China. Pediatrics 2020, e20200702. doi: 10.1542/peds.2020-0702 (Online ahead of print).
- Weigent, DA. Lymphocyte GH-axis hormones in immunity. Cell Immunol. 2013, 285, 118–32. doi: 10.1016/j.cellimm.2013.10.003.
- Liu, Q.L.; Zhang, J., Liu, X., Gao, JY. Role of growth hormone in maturation and activation of dendritic cells via miR-200a and the Keap1/Nrf2 pathway. Cell Prolif. 2015, 48, 573–81. doi: 10.1111/cpr.12206.
- Malarkey, W.B.; Wang, J,; Cheney, C.; Glaser, R; Nagaraja, H. Human lymphocyte growth hormone stimulates interferon-gamma production and is inhibited by cortisol and norepinephrine. J Neuroimmunol. 2002, 123, 180–7. doi: 10.1016/S0165-5728(01)00489-1.
- Weigent, D.A. High Molecular Weight Isoforms of Growth Hormone In Cells of the Immune System. Cell Immunol. 2011,271, 44–52. doi: 10.1016/j.cellimm.2011.06.001
- 9 Fahy, G.M.; Brooke, R.T.; Watson J.P-; Good, Z.; Vasanawala, S.S.; Maecker, H. et al. Reversal of epigenetic aging and immunosenescent trends in humans. Aging Cell 2019 18: e13028. doi: 10.1111/acel/.13028.
- 10 Kojima, N.; Koriyaa, N.; Tokito, A.; Ogiso, K., Kusumoto, K.; Kubo, s. et al. Growth Hormone Deficiency With Late-Onset Hypothalamic Hypoadrenocorticism Associated With Respiratory and Renal Dysfunction: A Case Report. BMC Endocr Disord. 2020 20, 50. doi: 10.1186/s12902-020-0536-3.
- Devesa, J.; Almengló, C.; Devesa, P. Multiple effects of Growth Hormone in the Body: Is it Really the Hormone for Growth?. Clin Med Insights Endocrinol Diabetes 2016, 9, 47-71. doi: 10.4137/CMED.S38201.
- Caicedo, D.; Devesa P.; Arce, V.M.; Requena, J.; Devesa, J. Chronic limb-threatening ischemia could benefit from growth hormone therapy for wound healing and limb salvage, Ther Adv Cardiovasc Dis, 2018, 12, 53-72. doi: 10.1177//175394471745492.
- Caicedo, D.; Díaz, O.; Devesa, P.; Devesa, J. Growth Hormone (GH) and Cardiovascular System. Int J Mol Sci. 2018, 19, 290. doi: 10.3390/ijms19010290.
- Caicedo, D.; Devesa, P.; Alvarez, C.V.; Devesa, J. Why Should Growth Hormone (GH) Be Considered a Promising Therapeutic Agent for Arteriogenesis? Insights from the GHAS Trial. Cells, 2020, 9, 807. doi: 10.3390/cells9040807.
- Kyriakakis, N.; Pechlivani, N.; Lynch, J.; Oxley, J.; Phoenix, F.; Seejore, K. et al. Prothrombotic Fibrin Network Characteristics in Patients with Acromegaly: A Novel Mechanism for Vascular Complications. Eur J Endocrinol. 2020, 182, 511-521. doi: 10.1530/EJE-19-0817.
- Devesa, J.; Díaz-Getino, G.; Rey, P.; García-Cancela, J.; Loures, I.; Nogueiras, S. et al. Brain Recovery after a Plane Crash: Treatment with Growth Hormone (GH) and Neurorehabilitation: a Case Report. Int J Mol Sci. 2015, 16, 30470-83. doi: 10.3390/ijms161226244.
- Heredia, M.; Palomero, J.; de la Fuente, A.; Criado, J.M; Yajeya, J.; Devesa, J. et al. Motor Improvement of Skilled Forelimb Use Induced by Treatment with Growth Hormone and Rehabilitation is Dependent on the Onset of the Treatment after Cortical Ablation. Neural Plast. 2018, 2018, 6125901. doi: 10.1155/2018:6125901.
- Devesa, J.; Núñez, I.; Agra, C.; Bejarano, A.; Devesa, P. Treatment with Growth Hormone (GH) Increased the Metabolic Activity of the Brain in an Elder Patient, Not GH-Deficient, Who Suffered Mild Cognitive Alterations and Had an ApoE 4/3· Genotype. Int J Mol Sci. 2018, 19, 2294. doi: 10.3390/ijms19082294.
- Renu, K.; Prasanna, P.L.; Abilash, V.G. Coronaviruses Pathogenesis, Comorbidities, and Multi-Organ Damage - A Review. Life Sci. 2020, 117839. doi: 10.1016/j.lfs.2020.117.839.
- Reiter, R.J.; Ma, Q.; Sharma, R. Treatment of Ebola and other infectious diseases: melatonin “goes viral”. Melatonin Res. 2020, 3, 43-57- doi: 10.32794/mr1 1250047.
- Junaid, A.; Tang, H.; van Reeuwijk, A.; Abouleila, Y.; Wuelfroth, P.; van Duinen, V. et al. Ebola hemorrhagic shock syndrome-on-a-chip. IScience. 2020, 23, 100765. doi: 10.1016/j.isci.2019.100765.
- Boga, J.A.; Coto-Montes, A.; Rosales-Corral, S.A.; Tan, D.X.; Reiter, R.J. Beneficial actions of melatonin in the management of viral infectios: a new use for this “molecular handyman”? Rev Med Virol. 2012, 22, 323-338. doi: 10.1002/mv.1714.
- Anderson, G.; Maes, M.; Markus, R.P.; Rodríguez,, M. Ebola virus: melatonin as a readily available treatment option. J Med Virol. 2015, 87, 537-543. doi: 10.1002/jmv.24130.
- Reiter, R.J.; Ma, Q.; Sharma, R. Melatonin in mitochondria: mitigating clear and present dangers. Physiology (Bethesda) 2020, 35, 86-95. doi: 10.1152/physiolo-00034.2019.
- Reiter, R.J.; Sharma, R.; Ma, Q.; Domínguez-Rodríguez, A.; Marik, P.E.; Abreu-González, P. Melatonin Inhibits COVID-19-induced Cytokine Storm by Reversing Aerobic Glycolysis inImmune Cells: A Mechanistic Analysis. Med Drug Discov, 2020, 6, 100044, doi:10.1016/j.medidd.2020.100044.
- Ma, S.; Chen, J.; Feng, J.; Zhang R.; Fan, M.; Han, D. et al. Melatonin ameliorates the progression of atherosclerosis via Mitophagy activation and NLRP3 Inflammasome Inhibition. Oxid Med Cell Longev. 2018, 2018: 9286458. doi: 10.1155/2018//9286458.
- Gurkan, O.U.; O’Donell, C.; Brower, R.; Ruckdeschel, E.; Becker, P.M. Differential Effects of Mechanical Ventilatory Strategy on Lung Injury and systemic Organ Inflammation in Mice. Am J Physiol Lung Cell Mol Physiol. 2003, 285, L710-8. doi: 10.1152./ajplung.000444.2003.
- Duflo, F.; Debon, R.; Goudable, J.; Chassard, D.; Allaouniche, B. Alveolar and Serum Oxidative stress in Ventilator-Associated Pneumonia. Br J Anaesth. 2002, 89, 231-6. doi: 10.1093/bja/aef169.
- Shneider, A.; Kudriatsev, A.; Vladimirovna, V.A. Can melatonin reduce the severity of COVID-19 pandemic? Int Rev Immunol. 2020, 29, 1-10. doi: 10.1080/08830185.2020.1756284.