Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Lily Guo and Version 1 by Guillermo García-Pérez-de-Sevilla.
The objective of this entry is to analyze the characteristics of multicomponent interventions aimed at reducing overweight and obesity in children in territories with an extremely cold climate.
- pediatric obesity
- obesity management
1. Introduction
The World Health Organization (WHO) has consistently reported that overweight and obesity are causing a significant deterioration in the health of the world’s population [1]. These conditions have been linked for decades to the development of diseases such as insulin resistance, type 2 diabetes mellitus, high blood pressure, dyslipidemia, and fatty liver disease [2,3,4][2][3][4]. More recently, obesity has been linked to various types of cancer [5], and it has been estimated that 14% and 20% of deaths in men and women, respectively, can be attributed to obesity [6].
Regarding the global prevalence of obesity, it has almost tripled. Specifically, in 2019 the estimation was that 38.2 million children under the age of five were overweight or obese. This is a problem in the high-, middle- and low-income countries, particularly in urban settings [7]. Besides, the prevalence of overweight and obesity among children and adolescents aged 5 to 19 years has increased dramatically, similarly among boys and girls [7].
The consequences of childhood obesity are increased school absences and doctor visits [8], so childhood obesity is not simply a risk factor for disease in adulthood, as obese children may experience more illness during childhood [9]. In this regard, early detection and treatment of obesity in children may be the best approach to prevent future increases in morbidity, as well as increases in the health care costs that are likely to occur as overweight and obese children, grow older [10,11][10][11].
Treatment strategies for childhood obesity have been carried out in multiple ways. Modifying the obesogenic environment and ensuring the acquisition of healthy lifestyle habits has been suggested for more than a decade [12]. Interventions with the family and school are considered an important strategy against obesity [13]. These strategies consist of nutrition, physical activity, or psychosocial support, and when used in combination they are called multi-component interventions [14,15][14][15].
It has been reported that there is an association between extreme cold weather and childhood overweight or obesity. Thus, it has been shown that cold environments favor the development of obesity since they could influence hormones related to hunger, increasing the appetite towards excessive intake, and promote inactivity [16,17][16][17]. Furthermore, this type of climate causes multiple systemic adaptations, such as sympathetic thermogenesis in brown adipose tissue, post-shiver thermogenesis in skeletal muscle, increased production of expired carbon dioxide due to increased metabolic activity, and tachycardia [18]. Similarly, exposure to cold temperatures alters hormonal production, observing an increase in ghrelin and cortisol, which have been associated with increased appetite, and facilitating mechanisms of lipid storage [19].
Among the coldest countries in the world are Russia, Canada, the USA (north), Iceland, Finland, Estonia, Norway, Sweden, Denmark, Latvia, France, and New Zealand (south) [20]. Scotland in the United Kingdom, the extreme south of Argentina and Chile [21], some areas of the island of Tasmania in Australia, part of the Atlantic coast of Norway, and part of the European islands in the North Atlantic Ocean belonging to the subpolar oceanic climate [22]. In this climate, months with an average temperature above 10 °C. are less than four per year.
In Punta Arenas, Chile, winds of 80 miles per hour are common during the southern hemisphere summer. The temperature varies around an average of 6.5 °C, with the lowest temperature of −16.4 °C in Winter, June, and July, and the highest of 29.9 °C in summer, January, and February [23].
The collected data on extreme cold weather is relevant for designing intervention strategies aimed at reducing overweight or obesity in children in these climates. To date, no systematic reviews have been reported that specify the characteristics of the interventions in children with overweight and obesity in territories with extremely cold climate characteristics.
2. Search Outcome
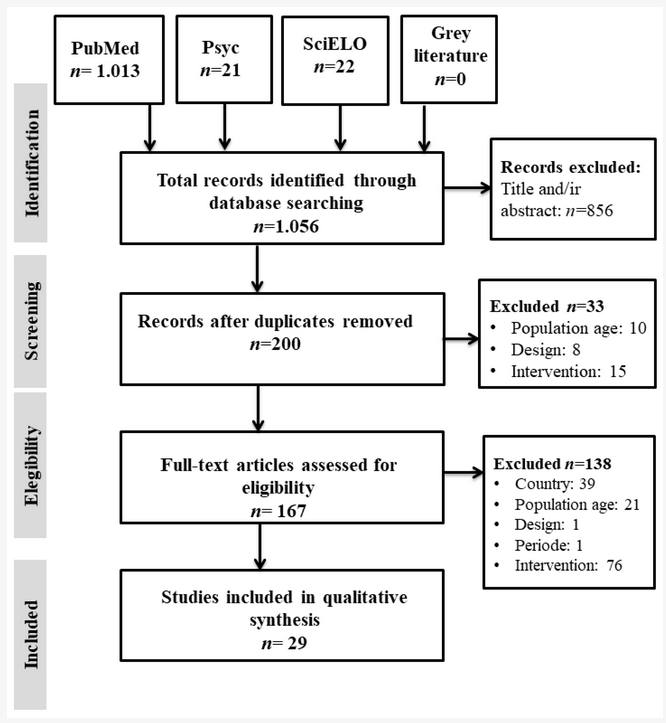
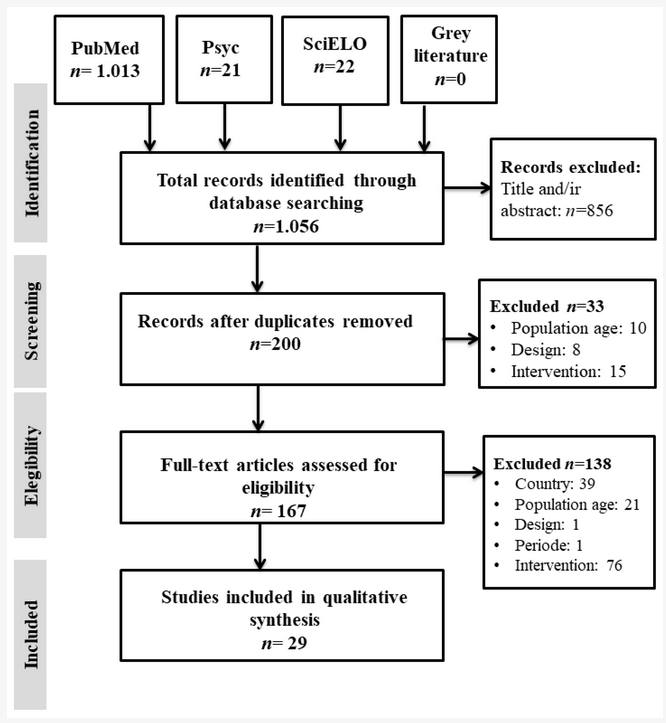
Figure 1 shows the flow chart made following the PRISMA Statement. We identified 1056 potential studies on the treatment of childhood overweight and obesity in countries with extremely cold climates. After the exclusion of the duplicates in the databases, the screening and eligibility criteria were applied. Finally, 29 articles were included for data synthesis in this review [27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55].
shows the flow chart made following the PRISMA Statement. We identified 1056 potential studies on the treatment of childhood overweight and obesity in countries with extremely cold climates. After the exclusion of the duplicates in the databases, the screening and eligibility criteria were applied. Finally, 29 articles were included for data synthesis in this review [24][25][26][27][28][29][30][31][32][33][34][35][36][37][38][39][40][41][42][43][44][45][46][47][48][49][50][51][52].
3. Characteristics of the Studies Analyzed
29 articles were included in this review, whose interventions were carried out in the following countries considered as extreme cold climate zones: Sweden, Canada, Denmark, United States, Iceland, Germany, Norway, Switzerland, England, Finland, Holland, and China. Considering all the studies, the total number of subjects at baseline was 4434, with an average adherence of 86%. The adherence to the programs, depending on the type of the intervention, was: (1) Physical activity and nutrition: 100%; (2) education: 93%; (3) behavioral and education: 93%; (4) physical activity and education and nutrition: 87%; (5) behavioral and nutrition: 86%; (6) physical activity and behavioral: 86%; (7) physical activity and behavioral and education and nutrition: 84%; (8) physical activity and behavioral and nutrition: 81%. Of these studies, 93% reported losses in their sample, the main reasons being categorized as follows: lack of time (10%), personal reasons (24%), attendance (41%), health (20%), not meeting criteria during the development of the intervention (17%), did not wish to continue (27%) and unspecified (34%). 58% of the studies recruited children from health centers, 27% from educational centers, and 51% from the community. The mean age was 9.3 years. Concerning gender distribution, 56% were women and 44% men. Regarding the prevalence of diseases, only two studies detailed this information: one included a child with asthma and the other only healthy children. The main inclusion criterion (90%) was the BMI value corresponding to overweight or obesity, while in 3% of the studies it was the value of weight for height and 7% did not specify this information. 51% of the interventions were carried out in health centers, 13% in educational centers, 13% in university centers, and 13% in community centers. Of these studies, 13% did not specify this information (Table 1).
Table 1.
Characteristics of the studies analyzed in multicomponent interventions in extremely cold climates.
| ef. | Main Author, Year, Country | Sample Size | Adherence | Reason for Exclusion | Recruiting | Age | Sex | Inclusion Criteria | Place of the Intervention | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ref. | Group | Participants | Interventions Characteristics | Intervention | Primary Outcome | Main Outcome | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ♀ | ||||||||||||||||||||||||||||||||||||||||||
| ♂ | Due. | Months | Tra | |||||||||||||||||||||||||||||||||||||||
| Professional Responsible | Phys. Act | Education | Beh. Ter | Nutrition | BMI | BMI | BMI | % | LT | PR | AT | NS | HE | DNMC | DWC | HC | EC | COM | mean | % | % | BMI | W/H | NS | HC | |||||||||||||||||
Duration equal to or less than six months: Considering all types of interventions, 77% obtained significant effects for the primary outcome. All the interventions that included the physical activity component showed significant effects on the primary outcome with the recreational activities modality, while with the recommendations modality they obtained significant effects in 59% of cases, and 83% of cases using the physical exercise program modality. All the interventions that included education had significant effects on the primary outcome, whereas those that included behavioral therapy had significant effects in 65% of cases. Finally, 100% of the nutrition component interventions showed significant effects on the primary outcome when using the diet program modality, 63% with the recommendation’s modality, and 50% when using the healthy cooking workshop modality. Furthermore, considering that all the interventions included at least two components, they all presented significant effects when they included the physical activity component in the form of recreational activities. However, the interventions that combined physical activity (recommendations approach), behavioral therapy, and nutrition component (recommendations approach) only presented significant effects when they also included the education component,
Duration equal or more than twelve months: of the interventions, 89% had significant effects on the primary outcome. 67% of interventions that included a physical activity component presented significant effects with the recreational activities modality, 100% with the recommendations modality, and 100% with the physical exercise program modality. Regarding interventions that included education, 92% presented significant effects on the result. The interventions that included behavioral therapy had significant effects in 91% of cases. Finally, 100% of the nutrition component interventions showed significant effects on the primary outcome with the diet program modality, 75% with the recommendations modality, and 100% with the healthy cooking workshop modality. Furthermore, only two interventions (11%) did not present significant effects, having in common that both included the nutrition component in the modality of recommendations (Table 3).
Table 3.
Statistically significant effects of the interventions lasting 6, and 12 months.
| Duration of the Intervention: 6 and 12 Months | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Physical Activity | Education | Behavioral Therapy | Nutrition | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| EC | UC | CC | NS | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| P | C | P-C | FAM | Nur | Nut | PA | MD | Psy | SW | Other | NS | Rec | PEP | RA | Rec | Cond | Rec | NP | RA | (kg/t2) | (z-) | (SD) | SC | MT | NSC | ||||||||||||||||||||||||||||||
| [27] | [24] | Mårild S. (2013), Sweden | 265 | 93 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| [27] | - | - | - | 1 | - | - | [ | - | - | 24 | 1 | - | 11 | 58 | 42 | - | - | 1 | 1 | - | - | - | ] | IG1- | |||||||||||||||||||||||||||||||
| - | - | 1 | - | 12 | - | 1 | 1 | - | - | - | - | - | - | 1 | - | - | - | 1 | 1 | - | - | - | 1 | - | 1 | - | Physical exercise program | - | [28] | ||||||||||||||||||||||||||
| Statistically significant change over the primary outcomes | Recreational activities | Recommendations | Nutrition program | Recommendations | Cooking class | ||||||||||||||||||||||||||||||||||||||||||||||||||
| [25] | Cohen T. (2016) Canada | 78 | 93 | 1 | 1 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| IG2 | - | - | - | - | - | - | - | 1 | 1 | 1 | 8 | 58 | 42 | 1 | - | - | - | - | 1 | 1 | - | 12 | - | 1 | 1 | 1- | - | - | - | - | - | 1 | - | - | -- | ||||||||||||||||||||
| 1 | 1 | - | - | - | - | - | - | - | - | [29] | [26] | Traberg C. (2016) Denmark | 115 | ||||||||||||||||||||||||||||||||||||||||||
| ≤6 months | 100% | 59% | 83% | 100% | 65% | 100% | 63% | 50% | 75 | - | - | - | 1 | ||||||||||||||||||||||||||||||||||||||||||
| [28] | [25] | IG1 | - | - | 1 | - | 1 | 12 | -1 | 1 | - | - | 11 | - | - | - | -12 | 45 | 55 | 1 | -- | - | - | - | - | 1 | - | ||||||||||||||||||||||||||||
| - | - | 1 | - | - | 1 | - | |||||||||||||||||||||||||||||||||||||||||||||||||
| ≥12 months | - | 67% | 100% | 1 | - | - | 1 | - | 1 | - | - | 100% | 92% | 91% | 100% | 75% | 100% | [30] | [27] | Saelens B. (2013) USA | 89 | 80 | - | - | 1 | - | - | - | - | 1 | - | 1 | 9 | 67 | 33 | 1 | - | - | - | - | - | - | 1 | ||||||||||||
| [31] | [28] | Gunnarsdottir T. (2014) Iceland | 16 | 81 | - | 1 | 1 | - | - | - | 1 | 1 | - | - | 10 | 68 | 32 | 1 | - | - | 1 | - | - | - | - | ||||||||||||||||||||||||||||||
| [32] | [29] | Harder-Lauridsen N. (2014) Denmark | 38 | 92 | - | 1 | - | - | - | 1 | - | - | 1 | - | 8 | 80 | 20 | 1 | - | - | -- | 1 | 1 | - | -- | 1 | - | ||||||||||||||||||||||||||||
| - | - | - | - | - | - | - | [33] | [30] | Reinehr T. (2010) Germany | 66 | 91 | - | - | - | 1 | - | - | - | 1 | - | 1 | 11 | 58 | ||||||||||||||||||||||||||||||||
| [30] | [27] | IG1 | - | - | 1 | - | 5 | 1 | - | - | - | - | - | - | 1 | -42 | 1 | - | 1 | -- | - | 1 | - | -- | - | - | |||||||||||||||||||||||||||||
| 1 | - | 1 | - | - | 1 | - | 1 | 1 | - | [34] | [31] | Benestad B. (2017) Norway | 94 | 73 | - | 1 | 1 | - | - | 1 | 1 | 1 | - | - | 10 | 50 | 50 | 1 | - | - | 1 | - | - | - | - | ||||||||||||||||||||
| [35] | [32] | Danielsson P. (2016) Sweden | 589 | 100 | - | - | - | - | - | - | - | 1 | - | - | 9 | 46 | 54 | 1 | - | - | 1 | - | - | - | - | ||||||||||||||||||||||||||||||
| [36] | [33] | Epstein L. (2014) USA | 101 | 66 | - | - | - | 1 | - | - | - | - | - | 1 | 11 | 60 | 40 | 1 | - | - | - | - | |||||||||||||||||||||||||||||||||
| - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| IG2 | - | - | - | 1 | 12 | - | - | 1 | - | - | - | - | - | - | 1 | - | - | 1 | - | - | 1 | - | - | - | - | - | - | - | |||||||||||||||||||||||||||
| [29] | [26] | IG1 | - | - | - | 1 | 1.5 | 1 | 1 | 1 | - | - | - | - | - | - | - | - | 1 | - | 1 | - | 1 | - | 1 | - | - | 1 | - | - | |||||||||||||||||||||||||
| IG2 | - | - | 1 | - | 1.5 | 1 | 1 | 1 | 1 | - | - | - | - | - | - | 1 | |||||||||||||||||||||||||||||||||||||||
| IG2 | - | - | 1 | - | 5 | 1 | - | - | - | - | - | - | 1 | - | 1 | - | - | - | 1 | - | 1 | - | - | - | - | - | - | - | |||||||||||||||||||||||||||
| [31] | [28] | IG | - | - | 1 | - | 4 | 1 | - | - | - | - | - | - | - | - | 1 | - | - | 1 | 1 | - | 1 | - | - | - | 1 | 1 | 1 | - | 1 | - | - | ||||||||||||||||||||||
| [32] | [29] | IG | - | - | - | 1 | 5 | - | - | 1 | 1 | - | - | - | - | - | - | 1 | - | 1 | - | 1 | - | - | 1 | - | - | 1 | - | - | [37] | [34] | |||||||||||||||||||||||
| [33] | Wilfley D. (2017) USA | 172 | 93 | - | - | - | 1 | - | - | - | - | - | 1 | 9 | 61 | 39 | [1 | - | 30- | - | - | 1 | - | - | |||||||||||||||||||||||||||||||
| ] | IG | - | - | - | 1 | 6 | - | - | 1 | 1 | 1 | 1 | - | - | - | - | - | - | 1 | - | - | 1 | - | 1 | - | - | 1 | - | - | [38] | [35] | Larsen L. (2015) Denmark | 80 | 93 | - | - | - | 1 | - | - | - | - | - | 1 | 6 | 64 | 36 | - | - | 1 | - | - | - | - | 1 |
| [34] | [31] | IG1 | - | - | - | 1 | 6 | 1 | 1 | - | 1 | 1 | - | - | - | - | 1 | - | - | - | 1 | - | - | - | 1 | - | 1 | - | - | 1 | [39] | [36] | Farpour-Lambert N. (2019) Switzerland | 74 | 89 | - | - | ||||||||||||||||||
| IG2 | - | - | - | - | 1 | 6- | 1 | - | 1 | 11 | 1 | - | - | 9 | 51 | 49 | 1 | - | - | 1 | - | - | 1 | 1 | 1 | 1 | - | - | -- | 1 | - | - | -- | ||||||||||||||||||||||
| 1 | 1 | - | - | - | - | - | - | - | - | [40] | [37] | Wylie-Rosett J. (2018) USA | 366 | 73 | - | - | 1 | - | - | 1 | 1 | 1 | - | ||||||||||||||||||||||||||||||||
| [35] | [32] | IG | - | - | - | 1 | - | 60 | - | 9 | 52 | 48 | 1 | 1 | 1 | - | 1 | 1 | 1- | 1 | - | - | -- | - | - | - | 1- | ||||||||||||||||||||||||||||
| - | 1 | - | 1 | - | - | - | - | 1 | 1 | 1 | - | [41] | [38] | Warschburger P. (2016) Germany | 685 | ||||||||||||||||||||||||||||||||||||||||
| [36] | [33] | IG1 | 76 | - | - | - | -1 | - | 1 | - | 12- | 1 | - | 1 | -- | - | - | - | -- | 11 | 52 | 48 | -1 | - | - | 1 | 1- | - | 1 | - | - | - | - | ||||||||||||||||||||||
| - | - | - | 1 | - | 1 | - | 1 | - | - | 1 | - | - | [42] | [39] | Christison A. (2016) USA | 84 | 95 | - | - | 1 | - | 1 | - | 1 | 10 | 54 | 46 | 1 | - | - | - | - | - | 1 | - | ||||||||||||||||||||
| IG2 | - | - | 1 | - | 12 | - | - | - | - | - | - | - | - | 1 | 1 | - | - | - | 1 | - | 1 | - | - | - | - | - | - | [43] | [40] | Croker H. (2012) England | 72 | 79 | - | - | 1 | - | 1 | - | 1 | 1 | 1 | 1 | 10 | ||||||||||||
| [37 | 70 | ] | [34 | 30 | 1 | - | - | 1 | - | ] | - | - | - | ||||||||||||||||||||||||||||||||||||||||||
| IG1 | - | - | - | 1 | 12 | - | - | - | - | - | - | - | 1 | - | - | - | - | 1 | 1 | - | - | - | 1 | - | - | 1 | - | - | [44] | [41] | Kokkvoll A. (2015) Norway | 97 | 85 | - | 1 | 1 | - | 1 | - | - | - | - | 1 | 10 | 54 | ||||||||||
| 46 | 1 | IG2 | - | - | - | - | 1 | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||
| 1 | 12 | - | - | - | - | - | - | - | 1 | - | - | - | - | 1 | 1 | - | - | - | - | - | - | - | - | - | [45] | [42] | Doyle-Baker P. (2011) Canada | 27 | 93 | - | - | 1 | - | - | - | - | |||||||||||||||||||
| [38] | [35] | IG1 | - | - | - | - | 1 | 8 | 52 | 48 | 1 | 1 | - | 12 | - | - | - | - | - | - | - | - | 1 | -- | - | - | - | - | - | 1 | |||||||||||||||||||||||||
| - | - | 1 | - | - | - | - | - | 1 | - | 1 | - | - | [46] | [43] | Kalavainen M. (2012) Finland | 70 | 97 | - | - | - | - | - | - | - | - | - | 1 | 8 | 60 | 40 | - | 1 | - | 1 | - | - | - | - | |||||||||||||||||
| IG2 | - | - | 1 | - | 12 | - | - | 1 | 1 | - | 1 | - | - | - | 1 | - | - | 1 | - | 1 | - | - | - | - | - | - | - | - | [47] | [44] | Njardvik U. (2018) Iceland | 90 | 67 | - | - | - | 1 | - | - | - | - | 1 | - | 11 | 45 | 55 | 1 | - | - | 1 | - | - | - | - | |
| [39] | [36] | IG1 | - | - | 1 | - | 6 | 1 | - | 1 | 1 | 1 | - | - | - | - | 1 | - | 1 | - | 1 | 1 | - | - | - | 1 | - | 1 | 1 | - | [48] | [45] | Gerards S. (2015) The Netherlands | ||||||||||||||||||||||
| IG2 | 86 | 85 | 1 | 1 | -1 | - | 1 | - | 6- | - | - | - | 11 | - | 1 | 1 | 1- | 1 | 7 | 55 | 145 | - | - | - | 11 | - | - | 1 | -- | - | - | - | |||||||||||||||||||||||
| 1 | - | 1 | 1 | - | - | - | - | - | - | - | - | [49] | [46] | Boutelle K. (2011) USA | 80 | 63 | 1 | 1 | |||||||||||||||||||||||||||||||||||||
| [40] | [37] | IG | - | - | 1 | -- | - | 1 | - | 1 | 1 | - | 12 | 1 | -1 | 10 | 60 | 40 | 1 | - | - | - | - | 11 | - | - | |||||||||||||||||||||||||||||
| 1 | 1 | - | 1 | - | - | 1 | - | 1 | 1 | 1 | 1 | - | 1 | - | 1 | - | 1 | - | - | [50] | [47] | ||||||||||||||||||||||||||||||||||
| [41 | Robertson W. (2017) England | ] | [38105 | ] | IG184 | - | - | - | 1- | 1 | - | 1 | -- | 12 | 1 | - | -1 | 1 | 1 | 1 | -9 | 1 | 1 | - | -65 | 35 | 1 | - | -- | - | - | 1 | 1- | 1 | - | 1 | 1- | ||||||||||||||||||
| - | 1 | - | - | - | 1 | 1 | 1 | - | [51] | [48] | Ming Hao M. (2019) China | 229 | 100 | - | - | - | - | - | - | - | - | 1 | - | 10 | 45 | 55 | 1 | - | - | - | 1 | - | - | - | |||||||||||||||||||||
| IG2 | - | - | 1 | - | 12 | 1 | - | - | - | 1 | 1 | - | - | - | - | - | 1 | 1 | 1 | - | 1 | - | - | - | - | - | - | - | [52] | [49] | Steven D. (2014) USA | 72 | 97 | - | - | 1 | - | - | - | - | 1 | - | - | 6 | 36 | 64 | 1 | - | - | ||||||
| [ | 1 | 42 | - | - | ] | - | - | ||||||||||||||||||||||||||||||||||||||||||||||||
| [39] | IG | - | - | 1 | - | 6 | 1 | - | 1 | - | 1 | - | - | 1 | - | - | 1 | - | - | 1 | - | - | - | 1 | 1 | - | - | - | 1 | [53] | [50] | de Niet J. (2012) Nederlands | 144 | 98 | - | - | - | 1 | - | - | - | 1 | - | - | 10 | 64 | 36 | 1 | - | - | 1 | - | - | - | - |
| [54] | [51] | Sherwood N. (2018) USA | 421 | 86 | - | - | 1 | - | - | - | - | 1 | - | - | 6 | 50 | 50 | 1 | - | - | 1 | ||||||||||||||||||||||||||||||||||
| [43] | [40] | IG | - | - | 1 | - | 6 | 1 | - | 1 | - | - | 1 | - | 1 | - | 1 | - | - | - | 1 | 1 | - | - | - | - | 1 | - | - | 1 | - | - | |||||||||||||||||||||||
| [44 | - | ] | [41 | - | |||||||||||||||||||||||||||||||||||||||||||||||||||
| ] | IG1 | - | - | - | 1 | 24 | - | 1 | 1 | 1 | 1 | - | - | 1 | - | - | - | 1 | 1 | - | 1 | - | - | - | - | 1 | - | - | 1 | [55] | [52] | Saelens B. (2017) USA | 29 | 82 | - | - | - | 1 | - | - | - | - | - | 1 | 10 | 59 | 41 | 1 | - | - | - | - | - | - | 1 |
4. Risk of Bias Assessment
The risk of bias analysis revealed that the distribution of biases classified as “low risk” or “unclear risk” was similar, except for detection bias, in which 66% of the studies presented “unclear risk”, and reporting bias, in which 100% of the studies presented “low risk”. Among the four types of bias, studies classified as “high risk” were only for “performance bias”, where more than 10% (22%) of the studies presented “high risk” (Figure 2).
5. Main Characteristics of the Interventions
The studies presented as a main result six variables related to childhood overweight and obesity: 38% reported BMI z-score, 34% reported BMI-SDS (standard deviation), 24% considered BMI (kg/m2), and 10% considered other variables, these being the percentage of body fat, body weight according to height and BMI-p (percentile). Regarding the main post-intervention result, 72% of the interventions presented significant changes, while 28% did not present significant post-intervention changes. Only nine studies analyzed the maintenance of this effect over time, obtaining statistically significant maintenance in 77% of cases. One of the inclusion criteria of 38% of the studies was that at least one of the parents was overweight or obese. Concerning the subjects who underwent the intervention, 4% included only parents, 6% only children, 52% included parents and children, and 34% included the entire family. In 59% of the studies, the duration of the intervention was equal to or less than 6 months, and in 41% it was equal to or greater than 12 months. 57% of the studies presented follow-up of post-intervention results. Of these, 43% followed up for a period equal to or less than 6 months, while 57% followed up for a period equal to or greater than 12 months. Regarding the professionals who participated in the interventions, 52% were nutritionists, 34% qualified professionals in exercise prescription (physiotherapists, physical education teachers, and personal trainers), 32% doctors, 27% psychologists, 27% other types of professional (interventionists, counselors or facilitators), 23% included a nurse, 2% a social worker and 9% did not specify this information. The interventions were based on four components: (1) physical activity, (2) education, (3) behavioral therapy, (4) and nutrition. The physical activity component was included in 86% of the interventions, being implemented in 55% of cases as recommendations (general exercise recommendations, promotion of an active life, and reduction of time spent in sedentary behaviors), in 16% of cases as physical exercise programs (structured training program including mainly aerobic exercise, circuit training, and spinning), and in 23% of cases as recreational activities (mainly games). Of the interventions. 55% included an education component, which was implemented mainly as healthy lifestyle recommendations focused on health promotion. Regarding behavioral therapy, 66% of the interventions included this component through cognitive-behavioral strategies: stimulus control, self-monitoring, coping strategies, dealing with problems, positive reinforcement, planning, goal setting, behavior skills, and parenting skills. Finally, 80% of the interventions included a nutrition component, which was implemented in 45% of cases as recommendations focused on healthy eating (such as increasing the intake of water, fruits, and vegetables and reducing the intake of high-calorie foods), in 34% of the cases as food plans using mainly the “traffic light system”, and in 6% of cases healthy eating workshops were included (Table 2).
Table 2.
Main characteristics of multicomponent interventions according to component addressed.
| IG2 | ||||||||||||||||||||||||||||||
| - | ||||||||||||||||||||||||||||||
| - | ||||||||||||||||||||||||||||||
| - | ||||||||||||||||||||||||||||||
| - | ||||||||||||||||||||||||||||||
| 24 | ||||||||||||||||||||||||||||||
| - | ||||||||||||||||||||||||||||||
| 1 | ||||||||||||||||||||||||||||||
| 1 | ||||||||||||||||||||||||||||||
| - | ||||||||||||||||||||||||||||||
| 1 | ||||||||||||||||||||||||||||||
| - | ||||||||||||||||||||||||||||||
| - | ||||||||||||||||||||||||||||||
| - | - | - | - | - | 1 | - | 1 | - | - | - | - | - | - | - | - | |||||||||||||||
| [45] | [42] | IG | - | - | 1 | - | 2.5 | - | - | - | 1 | - | - | - | 1 | - | - | 1 | - | 1 | - | 1 | - | - | - | - | - | 1 | - | - |
| [46] | [43] | IG | - | - | 1 | - | 6 | - | 1 | 1 | - | - | - | - | - | - | - | - | 1 | 1 | 1 | 1 | - | 1 | - | - | - | 1 | - | - |
| [47] | [44] | IG | - | - | 1 | - | 6 | 1 | - | 1 | 1 | 1 | 1 | - | - | - | 1 | - | - | 1 | 1 | 1 | - | - | - | - | 1 | 1 | 1 | - |
| [48] | [45] | IG | 1 | - | - | - | 4 | 1 | - | - | - | - | - | - | - | 1 | 1 | - | - | - | 1 | 1 | - | - | - | 1 | - | - | - | 1 |
| [49] | [46] | IG1 | 1 | - | - | - | 5 | 1 | - | - | - | - | 1 | - | - | - | 1 | - | - | - | 1 | - | 1 | - | - | - | - | 1 | - | - |
| IG2 | - | - | 1 | - | 5 | 1 | - | - | - | - | 1 | - | - | - | - | - | 1 | - | 1 | - | 1 | - | - | - | - | - | - | - | ||
| [50] | [47] | IG | - | - | - | 1 | 3 | 1 | - | - | - | - | - | - | 1 | - | 1 | - | - | - | 1 | 1 | - | 1 | - | 1 | - | - | - | 1 |
| [51] | [48] | IG1 | - | 1 | - | - | 2 | 1 | - | - | - | - | - | - | - | - | - | 1 | - | - | - | - | - | - | - | - | 1 | 1 | 1 | - |
| IG2 | - | 1 | - | - | 2 | 1 | - | 1 | - | - | - | - | - | - | - | - | - | 1 | - | - | - | - | - | - | - | - | - | - | ||
| IG3 | - | 1 | - | - | 2 | 1 | - | 1 | - | - | - | - | - | - | - | 1 | - | 1 | - | - | - | - | - | - | - | - | - | - | ||
| [52] | [49] | IG | - | - | 1 | - | 3 | - | - | - | - | - | - | - | 1 | - | 1 | - | - | - | 1 | 1 | - | - | - | 1 | - | - | - | 1 |
| [53] | [50] | IG | - | - | - | 1 | 12 | - | - | 1 | 1 | 1 | 1 | - | - | - | 1 | - | 1 | - | 1 | 1 | - | - | - | - | 1 | 1 | - | - |
| [54] | [51] | IG | - | - | - | 1 | 12 | 1 | - | - | - | - | - | - | 1 | - | - | - | - | - | 1 | 1 | - | - | - | - | 1 | - | - | 1 |
| [55] | [52] | IG1 | - | - | - | 1 | 6 | 1 | - | - | - | - | - | - | 1 | - | 1 | - | - | - | 1 | - | 1 | - | - | 1 | - | 1 | - | - |
| IG2 | - | - | - | 1 | 6 | 1 | - | - | - | - | - | - | - | - | 1 | - | - | - | - | - | 1 | - | - | - | - | - | - | - |
6. Effects of the Interventions on the Primary Outcome According to the Duration of the Intervention
7. Variables Studied in the Articles
The variables studied in the different studies were grouped into three categories: nutritional status, physical and health condition, and psychological variables.
7.1. Nutritional Status
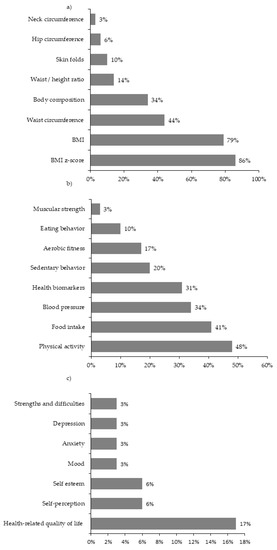
This category was considered in 100% of the studies and included eight variables: BMI z-score (86% of studies), BMI (79%), waist circumference (44%), body composition (mainly fat mass and lean mass; 34%), waist-to-height ratio (14%), skinfold (10%), hip circumference (6%) and neck circumference (3%) (Figure 3a).
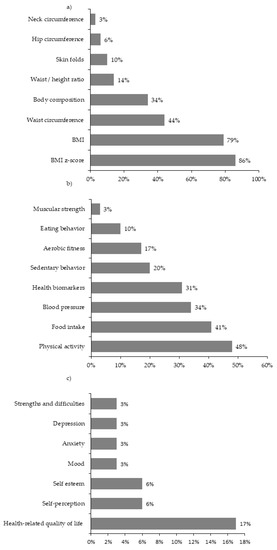
Figure 3.
Variables of (
a
) nutritional status, (
b
) physical and health condition, and (
c
) psychological health.
7.2. Physical and Health Condition
This category was considered in 76% of the studies and included eight variables: physical activity level (48% of studies), food intake (41%), blood pressure (34%), health biomarkers (31%), sedentary behavior (20%), aerobic fitness (17%), eating behavior (10%), muscular strength (3%) (Figure 3b).
7.3. Mental Health
This category was considered in 24% of the studies and included seven variables: health-related quality of life (17% of studies), self-perception (6%), self-esteem (6%), mood (3%), anxiety (3%), depression (3%), and strengths and difficulties perceived by parents (3%) (Figure 3c).
8. Assessment Instruments
The instruments used in the studies were grouped into three categories: nutritional status, physical and health condition, and psychological variables.
8.1. Nutritional Status
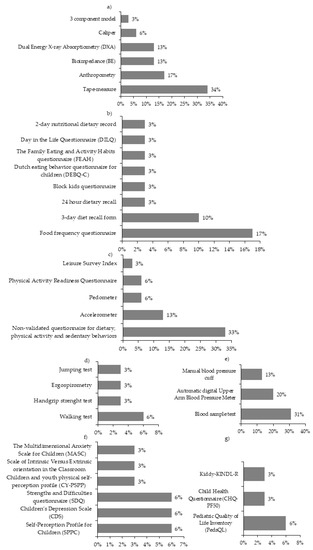
To assess these variables, six instruments were used: tape measure (34% of studies), anthropometry measurement (17%), bioimpedance measurement (13%), dual-energy x-ray absorptiometry (DXA) (13%), caliper (6%), and the three-component model of body composition (3%) (Figure 4a).
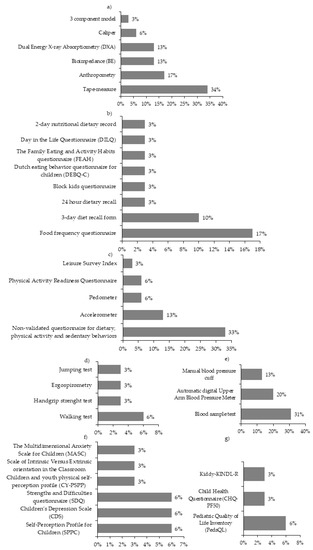
Figure 4.
Instruments for the assessment of (
a
) nutritional status, physical and health condition; (
b
) nutrition, (
c
) level of physical activity and sedentary behavior, (
d
) physical condition, (
e
) cardiovascular risk, psychological variables; (
f
) health and (
g
) health-related quality of life.
8.2. Physical and Health Condition
To assess these variables, 20 instruments were used and were sub-grouped into four categories:
Nutrition: to assess this category, the instruments used were food frequency questionnaire (17% of the studies), 3-day diet recall form (10%), 24h-dietary recall (3%), Block Kids questionnaire (3%), Dutch eating behavior questionnaire for children (DEBQ-C) (3%), The Family Eating and Activity Habits questionnaire (FEAH) (3%), Day in the life questionnaire (DiLQ) (3%) and 2-day nutritional dietary record (3%) (Figure 4b).
Level of physical activity and sedentary behavior: to assess this category, the instruments used were a non-validated questionnaire for dietary, physical activity, and sedentary behaviors (33% of studies), accelerometers (13%), pedometer (6%), Physical activity questionnaire for children (PAQ-Q) (6%), Leisure Score Index (LSI) (3%) (Figure 4c).
Physical condition: to assess this category, the instruments used were the walking test (6% of studies), handgrip strength test (3%), ergo-spirometry test (3%), jumping test (3%) (Figure 4d).
Cardiovascular risk: 31% of the studies took blood samples, while 13% measured blood pressure with a manual blood pressure cuff, and 20% with an automatic sphygmomanometer (Figure 4e).
8.3. Psychological Variables
Ten instruments were used to assess these variables and were sub-grouped into two categories:
Psychological health: to assess this category, 6% of studies used the self-perceptions profile questionnaire for children (SPPC), 6% the children’s depression scale (CDS), 6% the questionnaire of strengths and difficulties of the child reported by the parents (SDQ), 3% used the child and youth physical self-perception profile questionnaire (CY-PSPP), 3% the scale of intrinsic versus extrinsic orientation in the classroom, and 3% the multidimensional anxiety scale for children (MASC) (Figure 4f).
Health-related quality of life: of the studies, 6% used the pediatric quality of life questionnaire (PedsQL), 3% the child health questionnaire, Dutch version (CHQ-PF50), and 3% the quality of life questionnaire for children between 7 and 13 years old (KID-KINDL-R) (Figure 4g).
References
- Levesque, R.J.R. Obesity and overweight. In Encyclopedia of Adolescence; Springer: New York, NY, USA, 2011; pp. 1913–1915.
- Schattenberg, J.M.; Schuppan, D. Nonalcoholic steatohepatitis: The therapeutic challenge of a global epidemic. Curr. Opin. Lipidol. 2011, 22, 479–488.
- Daniels, S.R.; Pratt, C.A.; Hayman, L.L. Reduction of risk for cardiovascular disease in children and adolescents. Circulation 2011, 124, 1673–1686.
- O’Rahilly, S. Human obesity and insulin resistance: Lessons from human genetics. Clin. Biochem. 2011, 44, 451.
- Renehan, A.G.; Tyson, M.; Egger, M.; Heller, R.F.; Zwahlen, M. Body-mass index and incidence of cancer: A systematic review and meta-analysis of prospective observational studies. Lancet 2008, 371, 569–578.
- Amer, A.; Franchi, L.; Kanneganti, T.D.; Body-Malapel, M.; Özören, N.; Brady, G. Regulation of Legionella phagosome maturation and infection through flagellin and host Ipaf. J. Biol. Chem. 2006, 281, 35217–35223.
- Obesity and Overweight. Available online: (accessed on 17 November 2020).
- Kesztyüs, D.; Wirt, T.; Kobel, S.; Schreiber, A.; Kettner, S.; Dreyhaupt, J.; Kilian, R.; Steinacker, J.M. Is central obesity associated with poorer health and health-related quality of life in primary school children? Cross-sectional results from the Baden-Württemberg Study. BMC Public Health 2013, 13, 1–11.
- Wijga, A.H.; Scholtens, S.; Bemelmans, W.J.; de Jongste, J.C.; Kerkhof, M.; Schipper, M.; Sanders, E.A.; Gerritsen, J.; Brunekreef, B.; Smit, H.A. Comorbidities of obesity in school children: A cross-sectional study in the PIAMA birth cohort. BMC Public Health 2010, 10, 1–10.
- Verrotti, A.; Penta, L.; Zenzeri, L.; Agostinelli, S.; De Feo, P. Childhood obesity: Prevention and strategies of intervention. A systematic review of school-based interventions in primary schools. Mol. Diagn. Ther. 2014, 37, 1155–1164.
- Reinehr, T. Lifestyle intervention in childhood obesity: Changes and challenges. Nat. Rev. Endocrinol. 2013, 9, 607–614.
- Seidell, J.C.; Halberstadt, J. The global burden of obesity and the challenges of prevention. Ann. Nutr. Metab. 2015, 66, 7–12.
- Adab, P.; Pallan, M.J.; Lancashire, E.R.; Hemming, K.; Frew, E.; Barrett, T.; Bhopal, R.; Cade, J.E.; Canaway, A.; Clarke, J.L.; et al. Effectiveness of a childhood obesity prevention programme delivered through schools, targeting 6 and 7 year olds: Cluster randomised controlled trial (WAVES study). BMJ 2018, 360, k211.
- WHO. Report of the Commission on Ending Childhood Obesity: Implementation Plan: Executive Summary; WHO: Geneva, Switzerland, 2017.
- Wabitsch, M.; Moss, A.; Kromeyer-Hauschild, K. Unexpected plateauing of childhood obesity rates in developed countries. BMC Med. 2014, 12, 1–5.
- Habibzadeh, N. Why Physiologically Cold weather can Increase Obesity Rates? Int. Physiol. J. 2018, 2, 11–13.
- Young, T.K. Are the circumpolar inuit becoming obese? Am. J. Hum. Biol. 2007, 19, 181–189.
- Morrison, S.F. Central control of body temperature [version 1; referees: 3 approved]. F1000Research 2016, 5.
- Braghetto, I.; Taladriz, C.; Lanzarini, E.; Romero, C. Plasma ghrelin levels in the late postoperative period of vertical sleeve gastrectomy. Rev. Med. Chil. 2015, 143, 864–869.
- Anon. n.d. Top 15 Coldest Countries in the World 2020. Available online: (accessed on 17 November 2020).
- Köppen, W. Versuch einer Klassifikation der Klimate, vorzugsweise nach ihren Beziehungen zur Pflanzenwelt (Examination of a climate classification preferably according to its relation to the flora). Geogr. Zeitschr. 1900, 6, 593–611, 657–679.
- Sarricolea, P.; Herrera-Ossandon, M.; Meseguer-Ruiz, Ó. Climatic regionalisation of continental Chile. J. Maps 2017, 13, 66–73.
- Santana, A.; Butorovic, N.; Olave, C. Variación de la temperatura en punta arenas (chile) en los últimos 120 años. An. del Inst. la Patagon. 2009, 37, 85–96.
- Marild, S.; Gronowitz, E.; Forsell, C.; Dahlgren, J.; Friberg, P. A controlled study of lifestyle treatment in primary care for children with obesity. Pediatr. Obes. 2013, 8, 207–217.
- Cohen, T.R.; Hazell, T.J.; Vanstone, C.A.; Rodd, C.; Weiler, H.A. A family-centered lifestyle intervention for obese six-to eight-year-old children: Results from a one-year randomized controlled trial conducted in Montreal, Canada. Can. J. Public Health 2016, 107, e453–e460.
- Larsen, K.T.; Huang, T.; Ried-Larsen, M.; Andersen, L.B.; Heidemann, M.; Møller, N.C. A multi-component day-camp weight-loss program is effective in reducing bmi in children after one year: A randomized controlled trial. PLoS ONE 2016, 11, e0157182.
- Saelens, B.E.; Lozano, P.; Scholz, K. A randomized clinical trial comparing delivery of behavioral pediatric obesity treatment using standard and enhanced motivational approaches. J. Pediatr. Psychol. 2013, 38, 954–964.
- Gunnarsdottir, T.; Sigurdardottir, Z.G.; Njardvik, U.; Olafsdottir, A.S.; Bjarnason, R. A randomized-controlled pilot study of Epstein’s family-based behavioural treatment for childhood obesity in a clinical setting in Iceland. Nord. Psychol. 2011, 63, 6–19.
- Harder-Lauridsen, N.M.; Birk, N.M.; Ried-Larsen, M.; Juul, A.; Andersen, L.B.; Pedersen, B.K.; Krogh-Madsen, R. A randomized controlled trial on a multicomponent intervention for overweight school-aged children-Copenhagen, Denmark. BMC Pediatr. 2014, 14, 1–14.
- Reinehr, T.; Schaefer, A.; Winkel, K.; Finne, E.; Toschke, A.M.; Kolip, P. An effective lifestyle intervention in overweight children: Findings from a randomized controlled trial on ‘Obeldicks light’. Clin. Nutr. 2010, 29, 331–336.
- Benestad, B.; Lekhal, S.; Småstuen, M.C.; Hertel, J.K.; Halsteinli, V.; Ødegård, R.A.; Hjelmesæth, J. Camp-based family treatment of childhood obesity: Randomised controlled trial. Arch. Dis. Child. 2017, 102, 303–310.
- Danielsson, P.; Bohlin, A.; Bendito, A.; Svensson, A.; Klaesson, S. Five-year outpatient programme that provided children with continuous behavioural obesity treatment enjoyed high success rate. Acta Paediatr. Int. J. Paediatr. 2016, 105, 1181–1190.
- Epstein, L.H.; Paluch, R.A.; Wrotniak, B.H.; Daniel, T.O.; Kilanowski, C.; Wilfley, D.; Finkelstein, E. Cost-effectiveness of family-based group treatment for child and parental obesity. Child. Obes. 2014, 10, 114–121.
- Wilfley, D.E.; Saelens, B.E.; Stein, R.I.; Best, J.R.; Kolko, R.P.; Schechtman, K.B.; Wallendorf, M.; Welch, R.R.; Perri, M.G.; Epstein, L.H. Dose, content, and mediators of family-based treatment for childhood obesity a multisite randomized clinical trial. JAMA Pediatr. 2017, 171, 1151–1159.
- Larsen, L.M.; Hertel, N.T.; Mølgaard, C.; Christensen, R.D.; Husby, S.; Jarbøl, D.E. Early intervention for childhood overweight: A randomized trial in general practice. Scand. J. Prim. Health Care 2015, 33, 184–190.
- Farpour-Lambert, N.J.; Martin, X.E.; Bucher Della Torre, S.; Von Haller, L.; Ells, L.J.; Herrmann, F.R.; Aggoun, Y. Effectiveness of individual and group programmes to treat obesity and reduce cardiovascular disease risk factors in pre-pubertal children. Clin. Obes. 2019, 9, e12335.
- Wylie-Rosett, J.; Groisman-Perelstein, A.E.; Diamantis, P.M.; Jimenez, C.C.; Shankar, V.; Conlon, B.A.; Mossavar-Rahmani, Y.; Isasi, C.R.; Martin, S.N.; Ginsberg, M.; et al. Embedding weight management into safety-net pediatric primary care: Randomized controlled trial. Int. J. Behav. Nutr. Phys. 2018, 15, 1–12.
- Warschburger, P.; Kroeller, K.; Haerting, J.; Unverzagt, S.; van Egmond-Fröhlich, A. Empowering Parents of Obese Children (EPOC): A randomized controlled trial on additional long-term weight effects of parent training. Appetite 2016, 103, 148–156.
- Christison, A.L.; Evans, T.A.; Bleess, B.B.; Wang, H.; Aldag, J.C.; Binns, H.J. Exergaming for Health: A Randomized Study of Community-Based Exergaming Curriculum in Pediatric Weight Management. Games Health J. 2016, 5, 413–421.
- Croker, H.; Viner, R.M.; Nicholls, D.; Haroun, D.; Chadwick, P.; Edwards, C.; Wells, J.C.; Wardle, J. Family-based behavioural treatment of childhood obesity in a UK national health service setting: Randomized controlled trial. Int. J. Obes. 2012, 36, 16–26.
- Kokkvoll, A.; Grimsgaard, S.; Steinsbekk, S.; Flægstad, T.; Njølstad, I. Health in overweight children: 2-Year follow-up of Finnmark Activity School-A randomised trial. Arch. Dis. Child. 2015, 100, 441–448.
- Doyle-Baker, P.K.; Venner, A.A.; Lyon, M.E.; Fung, T. Impact of a combined diet and progressive exercise intervention for overweight and obese children: The BEHIP study. Appl. Physiol. Nutr. Metab. 2011, 36, 515–525.
- Kalavainen, M.P.; Korppi, M.O.; Nuutinen, O.M. Clinical efficacy of group-based treatment for childhood obesity compared with routinely given individual counseling. Int. J. Obes. 2007, 31, 1500–1508.
- Njardvik, U.; Gunnarsdottir, T.; Olafsdottir, A.S.; Craighead, L.W.; Boles, R.E.; Bjarnason, R. Incorporating appetite awareness training within family-based behavioral treatment of pediatric obesity: A randomized controlled pilot study. J. Pediatr. Psychol. 2018, 43, 1017–1027.
- Gerards, S.M.; Dagnelie, P.C.; Gubbels, J.S.; Van Buuren, S.; Hamers, F.J.; Jansen, M.W.; Van Der Goot, O.H.; De Vries, N.K.; Sanders, M.R.; Kremers, S.P. The effectiveness of lifestyle triple P in the Netherlands: A randomized controlled trial. PLoS ONE 2015, 10, e0122240.
- Boutelle, K.N.; Cafri, G.; Crow, S.J. Parent-only treatment for childhood obesity: A randomized controlled trial. Obesity 2011, 19, 574–580.
- Robertson, W.; Fleming, J.; Kamal, A.; Hamborg, T.; A Khan, K.; Griffiths, F.; Stewart-Brown, S.; Stallard, N.; Petrou, S.; Simkiss, D.; et al. Randomised controlled trial and economic evaluation of the ‘Families for Health’ programme to reduce obesity in children. Arch. Dis. Child. 2017, 102, 416–426.
- Hao, M.; Han, W.; Yamauchi, T. Short-Term and Long-Term Effects of a Combined Intervention of Rope Skipping and Nutrition Education for Overweight Children in Northeast China. Asia-Pac. J. Public Health 2019, 31, 348–358.
- Stovitz, S.D.; Berge, J.M.; Wetzsteon, R.J.; Sherwood, N.E.; Hannan, P.J.; Himes, J.H. Stage 1 treatment of pediatric overweight and obesity: A pilot and feasibility randomized controlled trial. Child. Obes. 2014, 10, 50–57.
- de Niet, J.; Timman, R.; Bauer, S.; van den Akker, E.; Buijks, H.; de Klerk, C.; Kordy, H.; Passchier, J. The effect of a short message service maintenance treatment on body mass index and psychological well-being in overweight and obese children: A randomized controlled trial. Pediatr. Obes. 2012, 7, 205–219.
- Sherwood, N.E.; Levy, R.L.; Seburg, E.M.; Crain, A.L.; Langer, S.L.; JaKa, M.M.; Kunin-Batson, A.; Jeffery, R.W. The Healthy Homes/Healthy Kids 5-10 Obesity Prevention Trial: 12 and 24-month outcomes. Pediatr. Obes. 2019, 14, e12523.
- Saelens, B.E.; Scholz, K.; Walters, K.; Simoni, J.M.; Wright, D.R. Two Pilot Randomized Trials to Examine Feasibility and Impact of Treated Parents as Peer Interventionists in Family-Based Pediatric Weight Management. Child. Obes. 2017, 13, 314–323.
More
